Open Reduction and Internal Fixation of Peritrochanteric Hip Fractures
Andrea Halim
Michael R. Baumgaertner
DEFINITION
Peritrochanteric hip fractures are defined as extracapsular hip fractures, always involving the trochanter and frequently with extension into the subtrochanteric region.
Medicare data indicates that as management of osteoporosis has improved, individual risk of sustaining a hip fracture has declined.4 However, with an aging population, the total number of hip fractures increases each year. According to a Medicare database, 786,717 hip fractures were reported between 1986 and 2005. These fractures account for approximately 20% of Medicare claims.
These fractures require operative intervention to achieve stable fracture fixation to allow immediate patient mobilization.
ANATOMY
The intertrochanteric region of the hip is notable for the anatomic transition from the femoral neck to the femoral shaft.
The angle subtended by the femoral neck and long axis of the femoral shaft in the coronal plane (the neck-shaft angle) is usually between 120 and 135 degrees in adults.
Studies have shown that this angle tends to decrease slightly with age.
The average femoral neck is anteverted between 10 and 15 degrees with respect to the femoral shaft.15
The peritrochanteric region of the femur is composed of multiple thickenings of trabecular bone distributed in compressive and tensile groups.5
The thickest and most structural are the primary compressive trabeculae located along the posterior medial aspect of the femoral neck and shaft, also known as the calcar.
Multiple muscle groups attach to this region of the femur:
Iliopsoas: attaches to the lesser trochanter and exerts a flexion and external rotation force to the hip
Abductors and short external rotators: attach to the greater trochanter
Adductors: attach to the femoral shaft distal to the peritrochanteric region
The blood supply to the peritrochanteric region of the femur is rich and abundant. The medial and lateral femoral circumflex arteries supply the cancellous bone of the trochanteric region through muscle attachments at the vastus origin and the insertion of the gluteus medius.
PATHOGENESIS
In the elderly population, most peritrochanteric fractures are caused by a fall onto the lateral aspect of the hip.
Numerous factors, such as structurally weak bone, lack of subcutaneous padding, and slowed protective reflexes lead to increased risk of hip fracture in the elderly population.
Pathologic lesions in the peritrochanteric region are not uncommon and may lead to fractures after relatively minor trauma.
Young patients who sustain peritrochanteric fractures are typically victims of high-energy trauma. In these cases, the fracture must be approached differently, with an attitude toward anatomic restoration of joint mechanics.
NATURAL HISTORY
Almost all peritrochanteric hip fractures will heal without intervention. However, owing to the pull of the musculature in this region, the fracture will heal in gross malalignment, leading to subsequent functional limitations.17
Early operative intervention of these fractures is undertaken to restore anatomic alignment and ensure that patients are mobilized quickly. Early fixation has been demonstrated to decrease incidence of pressure sores, pneumonia, and 30-day mortality.
PATIENT HISTORY AND PHYSICAL FINDINGS
It is important to elicit the cause of the patient’s fall, as many falls in the elderly population that result in hip fractures are due to medical comorbidities.
Elderly patients should be carefully evaluated and treated for rhabdomyolysis, dehydration, urinary tract infection, and malnutrition. In cases of preexisting poor mobility, consider deep vein thrombosis, and in anticoagulated patients it may be appropriate to obtain brain imaging.
Complaints of hip pain before falling may indicate a preexisting pathologic process that requires further evaluation.
A thorough whole-body musculoskeletal examination of the patient is necessary because of the high incidence of associated fractures (especially of the wrist and proximal humerus) in the elderly population sustaining hip fractures from simple falls. In cases of visible head trauma, cervical spine imaging can obviate prolonged cervical collar immobilization.
Examination of the soft tissue overlying the lateral hip, sacrum, and heels is necessary to ensure that no pressure ulcers or abrasions have occurred in these areas.
The classic physical finding in a patient with a peritrochanteric hip fracture is a shortened, externally rotated lower extremity.
Passive logrolling of the leg will elicit pain. This may be an especially helpful finding in occult hip fractures with no obvious fracture deformity.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographic anteroposterior (AP) pelvis and cross-table lateral images of the injured hip should be obtained initially.
AP and lateral views of the femur, including the knee joint, should be obtained both to assess the femoral bow as well as to evaluate the femoral canal in the event that an intramedullary device is required.
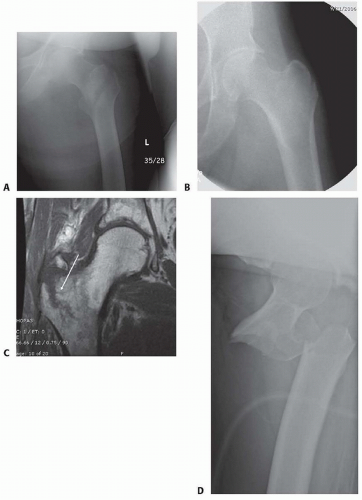
A traction radiograph (radiograph taken with firm manual traction and internal rotation of the leg) will provide more information on the fracture pattern and will allow a better comparison to the uninjured hip (FIG 1A,B). Alternatively, an obturator oblique view of the pelvis can allow for this comparison without requiring additional analgesic medication.
A fine-cut (2 mm) computed tomography (CT) scan with reconstruction images (sagittal and coronal) set to bone windows may help assess the fracture when ipsilateral femoral neck or other fractures are suspected.
Magnetic resonance imaging (MRI) is the modality of choice to assess for the presence of an occult peritrochanteric hip fracture in the setting of significant hip pain and normal radiographs (FIG 1C).
DIFFERENTIAL DIAGNOSIS
Femoral neck fracture
Hip dislocation
Femoral shaft fracture
Greater trochanter fracture
Septic hip
Pelvic ring injury
NONOPERATIVE MANAGEMENT
Early operative management of peritrochanteric fractures is associated with decreased patient morbidity and improved patient function compared to nonoperative management.
Relative indications for nonoperative management include nonambulatory patients with little pain, patients with active sepsis, patients with soft tissue compromise at the intended surgical site, and patients with severe and irreversible medical comorbidities precluding operative intervention.
Nonoperative management consists of two regimens:
Early mobilization
No attempt at axial realignment
Used for nonambulatory patients if contraindications to surgical management exist and consists of pain control and mobilization out of bed to chair as tolerated to avoid systemic complications of prolonged bed rest.
Traction
Attempted realignment with nonoperative management for ambulatory patients
Balanced traction for 8 to 12 weeks, with serial radiographs to assess healing
Progressive weight bearing as the fracture shows signs of healing
Skeletal traction is associated with fewer complications than skin traction. Skeletal traction through the distal femur is less likely to lead to knee stiffness and pain than traction placed through the proximal tibia.
SURGICAL MANAGEMENT
Once surgical management is chosen, the timing of intervention becomes important.
The balance between medical optimization and early operative management in this mostly elderly patient population is delicate.
Implant Selection
Implant selection for fracture fixation should be guided based on fracture pattern and patient age.
Implants that may be used include side plates with sliding hip screws, intramedullary devices (discussed in other chapters), blade plates, and proximal femoral locking plates.
All implants discussed are angular stable devices, in that they are designed to preserve the neck-shaft angle. Sliding hip screws and many intramedullary devices allow for sliding of the bone along the axis of the screw, which allows compression and shortening with weight bearing. With these devices, early weight bearing is allowed and some degree of shortening is expected.
Blade plates and proximal femoral locking plates are fixed length and preserve proximal femoral bone stock. These implants do not allow further compression or shortening across the fracture site, and patients often have restricted weight bearing following surgery.
Length-stable devices are generally indicated in younger patients because preserving abductor lever arm allows for preserved joint mechanics and the best chance at maintaining joint anatomy.
Preoperative Planning
Radiographs are reviewed to determine the fracture pattern.
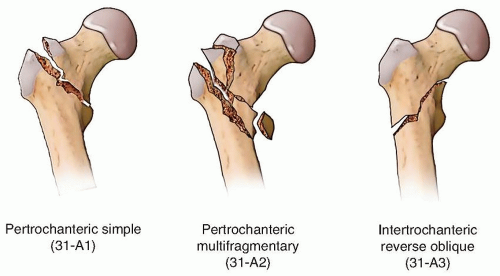
We find the AO Orthopaedic Trauma Association (AO/OTA) fracture classification system to be useful and reliable for peritrochanteric fractures. It is divided into groups based on fracture geometry (FIG 2):
Group 1 has a single fracture line extending to the medial cortex.
Group 2 has more than one fracture line extending to the medial cortex.
Group 3 has a fracture geometry that runs in a more transverse or reverse oblique pattern, with the fracture line exiting the lateral cortex below the vastus ridge.
Implant selection for peritrochanteric fractures in elderly, low-demand patients may be guided by an understanding of this fracture classification.
Group 1 fractures are fixed reliably with good results using either a sliding hip screw or intramedullary device.
Group 2 fractures have been shown to be amenable to treatment with either side plate and screw devices or intramedullary devices. Recent studies have shown improved patient outcomes and better maintenance of fracture alignment with the use of intramedullary devices in this type of fracture.13, 16
Group 3 fractures are treated best with intramedullary devices or angular stable plates.9
Sliding hip screw devices are contraindicated in these fractures because of the high incidence of implant failure.7
In a meta-analysis, intramedullary implants were found to have a lower failure rate than angular stable plates when used to treat this type of fracture pattern and should be considered the implant of choice for most surgeons for the elderly patient.7
The neck-shaft angle of the nonfractured femur should be measured preoperatively to estimate the reduction to be achieved (FIG 3).
Preoperative planning is vital for a satisfactory outcome when a peritrochanteric fracture is fixed with a blade plate.
Multiple views of the intact contralateral hip and femur, as well as multiple traction views of the fractured hip, are required to properly plan the surgical sequence for this type of fixation.
Proximal femoral locking plates are fixed-angle devices, which may be used as an alternative to blade plates.
These plates may be used for patients who have sustained ipsilateral shaft fractures, as length-stable implants in young patients, and in cases of periprosthetic fractures in combination with cerclage wires or cables when it is not possible to use intramedullary fixation.
Positioning
When fixing a peritrochanteric fracture with a sliding hip screw device, the patient is positioned on a well-padded fracture table, with the fractured leg placed in traction using a boot or heel cup. The well leg is carefully positioned in flexion and abduction in a well-leg holder, with care taken to pad the lateral knee and protect the peroneal nerve.
Use of a fracture table and thoughtful positioning of the contralateral well leg facilitate access by the fluoroscopic C-arm to the fractured hip (FIG 4A).
We prefer to secure the affected foot to a well-padded heel cup with tape, leaving the posteromedial neurovascular bundle uncompromised. The foot is then dorsiflexed and secured against a well-padded metatarsal bar to lock the transverse tarsal joint and allow strong traction and rotational forces to be transmitted to the fracture (FIG 4B).
Alternatively, if a fixed-angle plate is the selected implant, the patient is placed on a completely radiolucent flat-top table. The affected hip is bumped up at a 20- to 30-degree angle and the leg is draped free.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree