Open Achilles Tendon Repair
Sameh A. Labib
DEFINITION
The Achilles tendon is the strongest tendon in the body and is the primary plantarflexor of the ankle joint.16
Sudden stretch of the tendon tissue can result in complete or partial rupture, with an estimated incidence of 8 to 18 per 100,000 persons.1, 3
With complete rupture, the ruptured ends of the tendon may pull apart, leading to a significant plantarflexion weakness and to the creation of a gap that is palpated clinically.
A common source of confusion is that patients may continue to have active ankle plantarflexion due to the action of other flexors of the ankle.
As a result, the diagnosis is initially missed in an estimated 20% to 25% of cases.5
ANATOMY
Three calf muscles—the medial, lateral gastrocnemius, and soleus—converge together to form the “triceps surae” or the Achilles tendon (FIG 1).
The plantaris muscle originates from the lateral femoral condyle and passes obliquely between the gastrocnemius and soleus to reside medial to the Achilles tendon and inserts into it or the calcaneus. In an anatomic study, the plantaris muscle was absent in 7.3% of specimens.16
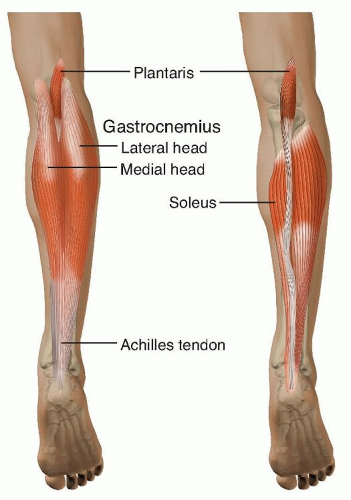
FIG 1 • The triceps surae (Achilles tendon) is formed by the convergence of the medial, lateral gastrocnemius, and soleus muscles.
The Achilles tendon courses distally, rotates 90 degrees internally, the soleus contribution being medial to that of the gastrocnemius, and inserts into the middle third of the flat surface of the posterior calcaneal tuberosity.10
The middle section of the tendon, 2 to 6 cm proximal to its insertion site, is a hypovascular zone.
This zone is the narrowest in cross-section and corresponds to the most common site of tendon pathology, including paratenonitis, tendinosis, and tendon rupture.10
The tendon is surrounded by a paratenon that has a single layer of cells with variable structure, not a true tenosynovium.
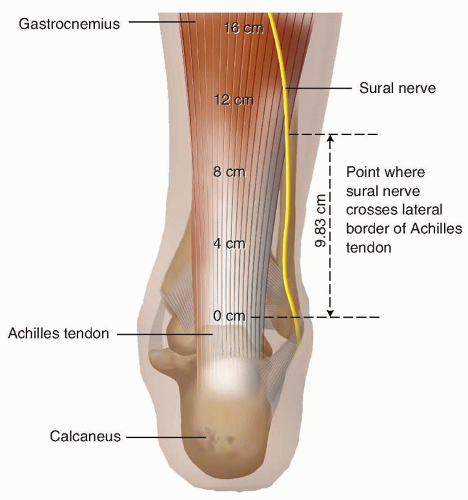
Webb et al17 documented the highly variable position of the sural nerve in relation to the Achilles tendon.
As measured from the calcaneal insertion, the sural nerve crossed the tendon from medial to lateral at a mean distance of 9.8 cm, then coursed distally to lie a mean of 18.8 mm laterally (FIG 2).
PATHOGENESIS
Achilles ruptures are usually caused by noncontact injuries. Common injury mechanisms leading to Achilles rupture are forceful push-off with an extended knee, sudden unexpected ankle dorsiflexion, or violent dorsiflexion of a plantarflexed foot.13
Achilles rupture can occur high, near the muscle-tendon juncture (9%), at the tendon midportion (72%), or at the calcaneal insertion (19%).5
Concomitant injuries such as ankle ligament sprains or ankle or tarsal fractures should be ruled out.
NATURAL HISTORY
Most Achilles ruptures do not have any antecedent symptoms.
A study of histologic scores comparing ruptured tendons with unruptured tendons, however, showed that there were significant histopathologic changes in the ruptured group that were not present in the older, asymptomatic, and unruptured group. Therefore, tendinosis may play a role, but the extent of this role remains unknown.14
Achilles rupture is more common in men. Studies have shown a male-to-female ratio of up to 12:1.
From an epidemiologic standpoint, middle-aged men with white-collar professions and recreational athletic activity constitute most of the patients.
Other predisposing factors are leg muscle imbalance, training errors, foot pronation, and use of corticosteroids and fluoroquinolones.13
In a longitudinal observational study, there was a contralateral Achilles rupture in 6% of patients who had a previously repaired Achilles rupture with a median delay of 3.1 years.1
PATIENT HISTORY AND PHYSICAL FINDINGS
Most ruptures occur during athletic activity. Patients usually describe a sudden painful snap or shooting pain followed by sudden weakness to foot push-off.
Athletes will be unable to bear weight and will report distal leg swelling and stiffness.
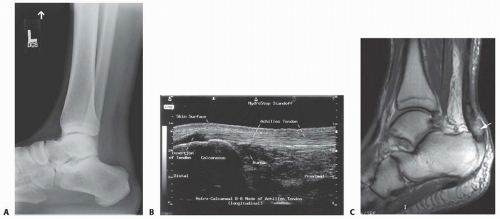
FIG 3 • A. Ankle radiograph showing a disrupted Kager triangle. B. Normal Achilles ultrasound image. C. Ankle MRI (T1-weighted image) showing a distal Achilles tendon rupture.
Examination for ruptured Achilles tendon can include the following:
Palpable gap test. A gap present indicates complete Achilles rupture with separation of the ruptured ends. It is more reliable when done early after rupture. It is 73% sensitive.13
Calf squeeze test (Thompson test). With patient prone, squeeze the calf and observe foot movement. Compare with the contralateral side. It is 96% sensitive.13
Knee flexion test. With patient prone, patient actively flexes knee. Observe foot position and compare with other. It is 88% sensitive.13
Active plantarflexion. This is poorly sensitive and unreliable because powerful plantarflexion may still be possible due to the action of other ankle plantarflexors.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP), lateral, and mortise view plain radiographs of the ankle should be obtained to rule out concomitant fractures or calcific changes of the Achilles tendon.
On a lateral view, the examiner should look for a disruption of the normal triangular fat pad seen anterior to the Achilles tendon (Kager triangle; FIG 3A).
Ultrasonography can provide a dynamic study of the tendon structure and accurately measure gapping of the ruptured tendon ends.
The quality of images is highly dependent on the equipment and operator (FIG 3B).
Magnetic resonance imaging (MRI) is highly sensitive and specific in diagnosing Achilles tendon rupture.
NONOPERATIVE MANAGEMENT
Traditionally, nonoperative treatment usually entailed casting the foot in plantarflexion to allow apposition of the tendon ends, followed by casting the foot in neutral. Treatment continues for 12 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree