• How did it all start? The possibilities are: no apparent cause, trauma or post-immobilization. A spontaneous onset indicates the possibility of rheumatoid arthritis or of a simple arthrosis. Trauma suggests traumatic arthritis. • Are other joints affected as well? If they are, this suggests a rheumatoid condition. • Which joints were affected first, the distal or the proximal joints? Arthrosis usually starts at the distal interphalangeal joints, whereas rheumatoid arthritis tends to start at the metacarpophalangeal joints. • Is the joint capsule swollen? Swelling often occurs in a rheumatoid or traumatic arthritis. • Does the joint change colour? The joint becomes red in gout. Rheumatoid arthritis is undoubtedly the most deforming and most incapacitating disorder of the hand.1 As in any other patient, symptoms may develop that have nothing to do with the patient’s rheumatoid arthritis. Trigger finger, carpal tunnel syndrome and de Quervain’s disease are common, and another possibility is a ganglion lying between the heads of the second and third metacarpal bones, which gives rise to vague local aching and responds well to aspiration.2 Traumatic arthritis of the finger joints does not respond satisfactorily to any treatment. Intra-articular injection with a steroid, so useful in traumatic arthritis in the toe joints, affords no corresponding benefit in the fingers. Recovery is spontaneous over 6–18 months, depending on the severity of the original trauma and the age of the patient. Sometimes manual therapeutic techniques may favourably alter the natural course.3 Immobilization is strongly contraindicated. Occasionally arthrosis in one joint develops as the result of severe injury but more often the condition has a spontaneous onset and affects several joints. Women between 40 and 60 years of age are often affected, and there is a strong familial predisposition.4 Arthrosis begins at the distal interphalangeal joints, and its knobbly appearance is quite different from rheumatoid arthritis. Both hands are usually affected more or less symmetrically. The index, middle and ring fingers are most usually affected. At the base of the distal phalanx, two small rounded bosses on the dorsum of the joint (Heberden’s nodes)5 can be seen. A varus deformity may develop at a distal joint, usually at the index. Some years later, the arthrosis may spread to the proximal interphalangeal joints (with the formation of nodes at index and middle fingers – Bouchard’s nodes); it seldom reaches the metacarpophalangeal joints. From time to time, a new node forms at an affected joint and the patient will mention some aching or slight pain over 1 or 2 months, during which time the fingertip may occasionally become pink. The colour is mottled and different from the shiny red of gout. After a month or two the discolouration passes off and the node ceases to be painful. The radiograph clearly shows the usual arthrotic changes – osteophytes and erosion of cartilage. Strains of muscles and tendons in the hand are not infrequent. They have no tendency to spontaneous cure. Diagnosis is not difficult and conservative treatment leads to good results. All the intrinsic muscles of the hand and their short tendons respond immediately to adequate deep transverse friction but not to infiltrations with steroids. In contrast, friction has no effect on the long flexor tendons in the palm but triamcinolone infiltration is successful.7
Disorders of the hand and fingers
Disorders of the inert structures
The capsular pattern
Rheumatoid arthritis
Traumatic arthritis
Arthrosis
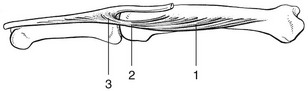
Disorders of the contractile structures