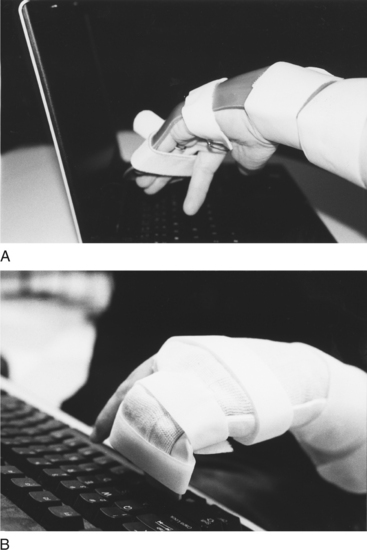
CHAPTER 2 “Man, through the use of his hands as they are energized by mind and will, can influence the state of his own health” [Reilly 1962, p. 2]. 1 Define occupation-based treatment as it relates to splint design and fabrication. 2 Describe the influence of a client’s occupational needs on splint design and selection. 3 Review evidence to support preservation of occupational engagement through splinting. 4 Describe how to utilize an occupation-based approach to splinting. 5 Review specific hand pathologies that create the potential for occupational dysfunction. 6 Describe splint design options to promote occupational engagement. 7 Apply knowledge of application of occupation-based practice to a case study. As stated eloquently by Mary Reilly [1962], this phrase reminds us that the hand, as directed by the mind and spirit, is integral to function. Occupation-based splinting is an approach that promotes the ability of the individual with hand dysfunction to engage in desired life tasks and occupations [Amini 2005]. Occupation-based splinting is defined as “attention to the occupational desires and needs of the individual, paired with the knowledge of the effects (or potential effect) of pathological conditions of the hand, and managed through client-centered splint design and provision” [Amini 2005, p. 11]. Prior to starting the splinting process, the therapist must adopt a personal philosophy that supports occupation-based and client-centered practice. Multiple models of practice exist that adopt this paradigm, including the Canadian Model of Occupational Performance (COPM), The Contemporary Task-Oriented Approach [Kamm et al. 1990], and the Model of Human Occupation and Occupational Adaptation [Law 1998]. In addition, the occupational therapist should understand the tenets of the Occupational Therapy Practice Framework (OTPF) and its relationship to the International Classification of Functioning, Disability and Health (ICF). The profession of occupational therapy adopted the use of splints, an ancient technique of immobilization and mobilization, in the mid part of the twentieth century [Fess 2002]. According to Fess, the most frequently recorded reasons for splinting include increasing function, preventing deformity, correcting deformity, protecting healing structures, restricting movement, and allowing tissue growth or remodeling [Fess et al. 2005]. Such reasons for splinting relate to changing the condition of the neuro-musculoskeletal system and body functions within the client factors category of the OTPF. However, body components comprise only a part of the overall occupational behavior of the client, and despite the importance of assisting the healing or mobility of the hand the therapist must immediately and concurrently tend to the needs of the client that transcend movement and strength of the body. This chapter provides definitions of client-centered and occupation-based practice. The process of combining both approaches to splinting is presented, with suggested assessment tools and treatment approaches that are compatible with such practice approaches. Splinting options that promote occupational functioning are described. Client-centered and occupation-based practice are compatible, but a distinction is made between the two [Pierce 2003]. Client-centered practice is defined as “an approach to service which embraces a philosophy of respect for, and partnership with, people receiving services” [Law et al. 1995, p. 253]. Law [1998] outlined concepts and actions of client-centered practice, which articulate the assumptions for shaping assessment and intervention with the client (Box 2-1). Occupation-based practice is “the degree to which occupation is used with reflective insight into how it is experienced by the individual, how it is used in natural contexts for that individual, and how much the resulting changes in occupational patterns are valued by the client” [Goldstein-Lohman et al. 2003]. Methods of employing empathy, reflection, interview, observation, and rigorous qualitative inquiry assist in understanding the occupations of others [Pierce 2003]. Christiansen and Townsend [2004] described occupation-based occupational therapy as an approach to treatment that serves to facilitate engagement or participation in recognizable life endeavors. Pierce [2003] described occupation-based treatment as including two conditions: (1) the occupation as viewed from the client’s perspective and (2) the occupation occurring within a relevant context. According to the OTPF, context relates “to a variety of interrelated conditions within and surrounding the client that influence performance” [AOTA 2002, p. 613]. Contexts include cultural, physical, social, personal, spiritual, temporal, and virtual aspects [AOTA 2002]. Thus, you should consider both factors when working with clients.Box 2-2 describes the contexts. Occupation-based splinting is a treatment approach that supports the goals of the treatment plan to promote the ability of clients to engage in meaningful and relevant life endeavors. Unlike a more traditional model of splinting that may initially focus on body structures and processes, occupation-based splinting incorporates the client’s occupational needs and desires, cognitive abilities, and motivation. When using occupation-based splinting, the therapist recognizes that the client is an active participant in the treatment and decision-making process [Amini 2005]. Splinting as occupation-based and client-centered treatment focuses on meeting client goals as opposed to therapist-designed or protocol-driven goals. Body structure healing is not the main priority. It is a priority equal to that of preservation of occupational engagement. Occupation-based splinting can be viewed as part of a top-down versus bottom-up approach to occupational therapy intervention. According to Weinstock-Zlotnick and Hinojosa [2004], the therapist who engages in a top-down approach always begins treatment by examining a client’s occupational performance and grounds treatment in a client-centered frame of reference. A therapist who uses a bottom-up approach first evaluates the pathology and then attempts to connect the body deficiencies to performance difficulties. To be truly holistic, one must never rely solely on one method or frame of reference for treatment. Treating a client’s various needs is a first and foremost priority. According to the OTPF, occupational therapy is an approach that facilitates the individual’s ability to engage in meaningful activities within specific performance areas of occupation and varied contexts of living [AOTA 2002]. The performance areas of occupation define the domain of occupational therapy and include activities of daily living (ADLs), instrumental activities of daily living (IADLs), leisure, play, work, education, and social participation [AOTA 2002]. Context is a strong component of occupational engagement that permeates all levels of treatment planning, intervention, and outcomes. An often overlooked issue surrounding splinting is attention to the client’s cultural needs. Unfortunately, to ignore culture is to potentially limit the involvement of clients in their splint programs. For example, there are cultures whereby the need to rely on a splint is viewed as an admission of vulnerability or as a weakness in character. Such feelings can exist due to large group beliefs or within smaller family dynamic units. Splinting within this context must involve a great deal of client education and possibly education of family members. Issuing small, unobtrusive splints that allow as much function as possible may diminish embarrassment and a sense of personal weakness [Salimbene 2000]. A knowledge of physical environments may contribute to an understanding of the need for splint provision. Physical environments may also hamper consistent use if clients are unable to engage in required or desired activities. For example, if a client needs to drive to work and is unable to drive while wearing a splint he might remove it despite the potential for reinjury.Figure 2-1A depicts a young woman wearing a splint because she sustained a flexor digitorum profundus injury. She found that typing at her workplace while wearing the splint was creating shoulder discomfort. She asked the therapist if she could remove her splint for work, and with physician approval the therapist created a modified protective splint (Figure 2-1B). The newly modified splint allowed improved function and protected the healing tendon. Social contexts pertain to the ability of clients to meet the demands of their specific group or family. Social contexts are taken into consideration with splint provision. For example, a new mother is recently diagnosed with de Quervain’s tenosynovitis and is issued a thumb splint. The mother feels inadequate as a mother when she cannot cuddle and feed the infant without contacting the infant with a rigid splint. In such a case, a softer prefabricated splint or alternative wearing schedule is suggested to maximize compliance with the splint program (Figure 2-2). Personal context involves attention to such issues as age, gender, and educational and socioeconomic status. When clinicians who employ occupation-based splinting fabricate splints for older adults or children, they consider specific guidelines (see Chapters 15 and 16). The choices in material selection and color may be different based on age and gender. For example, a child may prefer a bright-colored splint whereas an adult executive may prefer a neutral-colored splint. Concerns may arise about the role educational level plays in splint design and provision. For clients who have difficulty understanding new and unfamiliar concepts, it is important to have a splint that is simple in design and can be donned and doffed easily. Precautions and instructions should be given in a clear manner. Pedretti and Early [2001] described four intervention levels: adjunctive, enabling, purposeful activities, and occupations. Adjunctive methods prepare clients for purposeful activity and they do not imply activity or occupation. Examples include exercise, inhibition or facilitation techniques, and positioning devices. Enabling activities precede and simulate purposeful activity. For example, simulated activities (e.g., driving simulators) begin to prepare the client for participation in actually driving a vehicle. Purposeful activities are goal directed and have meaning and purpose to the client. In the case of driving, when a client actually gets into a vehicle and drives, the intervention level is considered purposeful activity. Occupation is the highest level of intervention. Clients participate in occupations in their natural context. The ability to drive to one’s employment site is considered an occupation. The OTPF intervention approaches are defined as “specific strategies selected to direct the process of intervention that are based on the client’s desired outcome, evaluation data and evidence” [AOTA 2002, p. 632]. These treatment approaches include processes to (1) create or promote health, (2) establish or restore health, (3) maintain health, (4) modify through compensation and adaptation, and (5) prevent disability [AOTA 2002]. Within the context of occupation-based practice, splinting is a therapeutic approach interwoven through all levels of intervention. Splinting is a facilitator of purposeful and occupation-based activity. The OTPF describes specific therapeutic outcomes expected of intervention. Outcomes are occupational performance, client satisfaction, role competence, adaptation, health and wellness, prevention, and quality of life [AOTA 2002]. Positive outcomes in occupational performance are the effect of successful intervention. Such outcomes are demonstrated either by improved performance within the presence of continued deficits resulting from injury or disease or the enhancement of function when disease is not currently present. Splinting addresses both types of occupational performance outcomes (improvement and enhancement). Splints that improve function in a person with pathology result in an “increased independence and function in an activity of daily living, instrumental activity of daily living, education, work, play, leisure, or social participation” [AOTA 2002, p. 628]. For example, a wrist immobilization splint is prescribed for a person who has carpal tunnel syndrome. The splint positions the wrist to rest the inflamed anatomical structures, thus decreasing pain and work performance improves. Splints that enhance function without specific pathology result in improved occupational performance from one’s current status or prevention of potential problems. For example, some splints position the hands to prevent overuse syndromes resulting from hand-intensive repetitive or resistive tasks. Health and wellness are collectively described as the absence of infirmity and a “state of physical, mental, and social well-being” [AOTA 2002, p. 628]. Splinting promotes health and wellness of clients by minimizing the effects of physical disruption through protection and substitution. Enabling a healthy lifestyle that allows clients to experience a sense of wellness facilitates motivation and engagement in all desired occupations [Christiansen 2000]. Prevention in the context of the OTPF involves the promotion of a healthy lifestyle at a policy creation, organizational, societal, or individual level [AOTA 2002]. When an external circumstance (e.g., environment, job requirement, and so on) exists with the potential for interference in occupational engagement, a splinting program may be a solution to prevent the ill effects of the situation. If it is not feasible to modify the job demands, clients may benefit from the use of splints in a preventative role. For example, a wrist immobilization splint and an elbow strap are fitted to prevent lateral epicondylitis of the elbow for a client who works in a job that involves repetitive and resistive lifting of the wrist with a clenched fist. In addition, the worker is educated on modifying motions and posture that contribute to the condition. Of great concern is the concept of quality of life [Sabonis-Chafee and Hussey 1998]. Although listed as a separate therapeutic outcome within the OTPF, quality of life is a subjective state of being experienced by clients. Quality of life entails one’s appraisal of abilities to engage in specific tasks that beneficially affect life and allow self-expressions that are socially valued [Christiansen 2000]. One’s state of being is determined by the ability of the client to be satisfied, engage in occupations, adapt to novel situations, and maintain health and wellness. Ultimately, splinting focused on therapeutic outcomes will improve the quality of life through facilitating engagement in meaningful life occupations.
Occupation-Based Splinting
Client-Centered versus Occupation-Based Approaches
Occupation-Based Splint Design and Fabrication
Occupation-Based Splinting and Contexts
Occupation-Based Splinting and Intervention Levels
Splinting as a Therapeutic Approach
Splinting as a Facilitator of Therapeutic Outcomes
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine