CHAPTER 23 Nonunion and Malunion of Distal Humerus Fractures
INTRODUCTION
Nonunion and malunion are two of the most common and challenging complications of distal humerus fractures. Newer internal fixation principles and techniques have improved our ability to achieve stable fixation of complex distal humerus fractures18 (see Chapter 22, Current Concepts in Fractures of the Distal Humerus). However, some fractures will fail to unite, leaving the patient with an unstable, dysfunctional, and oftentimes painful upper extremity requiring additional surgery. Distal humeral malunion is well characterized in the pediatric population after supracondylar fractures (see Chapters 14 and 15) but has not been analyzed as extensively in the adult population.4,8 This chapter reviews the prevalence, risk factors, pathology and treatment options for distal humeral nonunions and the clinical relevance and treatment options for distal humeral malunion.
DISTAL HUMERAL NONUNION
PREVALENCE AND RISK FACTORS
Distal humerus nonunion with hardware failure and fracture redisplacement usually presents within the first few months after surgery. The prevalence of hardware failure is difficult to determine, because in some cases, hardware failure may allow ultimate fracture healing with residual secondary displacement. In addition, some potential failures of fixation may be avoided by prolonged postoperative immobilization, leading to fracture healing but very limited motion. Nonunion or hardware failure have been reported in approximately 8% to 25% of recent series on distal humerus fractures.6,9,14,19,20
PATHOLOGY
Distal humeral nonunions share a constellation of pathologic findings that need to be addressed at the time of surgery (Fig. 23-1). The nonunion is usually located at the supracondylar level; most of the time, the distal fragments heal in a more or less anatomic position. Progressive bone reabsorption at the nonunion site may lead to severely compromised bone stock. Previously placed hardware may compromise bone stock even further, especially when screw loosening results in a windshield-wiper effect.
Additionally, severe stiffness develops, and when the patient tries to flex and extend the elbow, most motion occurs through the nonunion site, not through the joint.7 Failure to release the associated elbow contracture at the time of fixation of the nonunion may contribute to failure; otherwise, when elbow motion is rehabilitated excessive loads are transmitted through the nonunion site. Not uncommonly, ulnar nerve excursion is compromised by scarring, especially when there has been previous surgery. Excessive motion at the nonunion site may further compromise the function of the ulnar nerve by stretching. Attention should be paid to the ulnar nerve at the time of surgery.
EVALUATION AND TREATMENT OPTIONS
Imaging Studies
Simple Radiographs
When possible, sequential radiographs should be evaluated to understand the initial fracture pattern, assess the quality of the initial fixation when previously attempted, and determine the amount of bone loss. Recent radiographs will help determine the feasibility of repeated internal fixation versus arthroplasty and the need for structural bone graft and special tools for hardware removal.
Computed Tomography
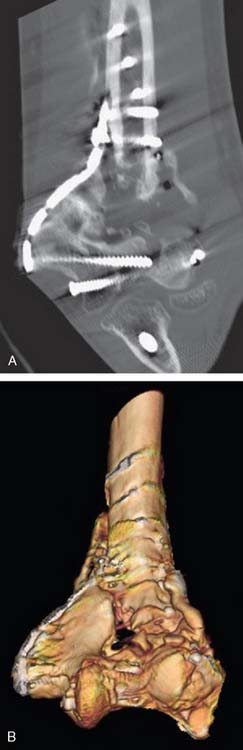
Computed tomography with three-dimensional reconstruction is an invaluable tool when repeated internal fixation is planned (Fig. 23-2), because it provides a better understanding of the remaining bone stock and any degree of associated malunion, and facilitates planning of plate and screw placement in order to achieve the maximum anchorage of the fixation devices.
INTERNAL FIXATION
Surgical Technique
Surgical Approach and Ulnar Nerve Decompression
Most patients with previous surgery will have a posterior midline skin scar that may be used for the revision procedure. If the previous fixation was attempted through separate lateral and medial incisions, most of the time, it is better to ignore those and create a new posterior midline skin incision, unless the skin quality is compromised and wound problems are anticipated. Next, the ulnar nerve should be identified; when a previously transposed ulnar nerve is asymptomatic, additional nerve dissection should be avoided as long as the procedure can be performed without further nerve exposure and the ulnar nerve can be protected and reassessed at the end of the procedure. The nerve should be formally isolated and transposed when it was left in situ during previous surgeries.7 Neurolysis should be considered in patients with a previously transposed symptomatic ulnar nerve.
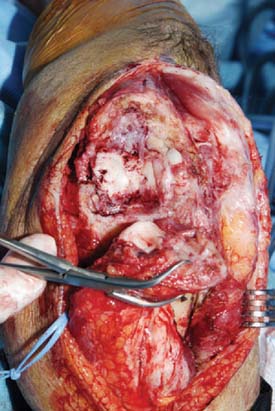
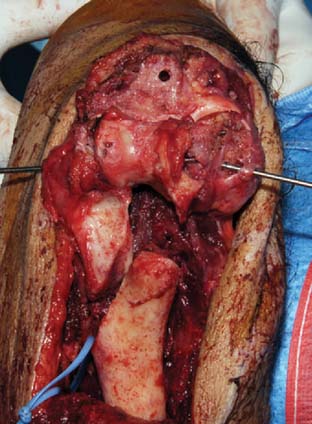
Several deep exposures may be used. A nonunited previous olecranon osteotomy should be used for exposure whenever present. Similarly, when a triceps-reflecting or triceps reflecting anconeus pedicle (TRAP) approach was used for previous surgeries, the same approach should be used if incomplete healing of the extensor mechanism to the olecranon is found at the time of surgery.11 For extra-articular nonunions with an intact extensor mechanism, the so-called bilaterotricipital approach (working on both sides of the triceps without violating the extensor mechanism) provides good exposure while preventing complications such as olecranon nonunion or triceps weakness (Fig. 23-3).2 Olecranon osteotomy provides an excellent exposure and is used by many surgeons for fixation of distal humerus nonunion (Fig. 23-4).15 Alternatively, a triceps-reflecting (Bryan-Morrey or Mayo-modified extensile Kücher) or TRAP approach is selected when the decision to proceed with fixation versus arthroplasty will be taken intraoperatively.3 Once the deep exposure is complete, tissue should be sent routinely for pathology and microbiology.
Capsular Release
Capsular contracture is a constant feature of distal humerus nonunions. Failure to release the contracture will limit final range of motion and increase the stress transmitted to the nonunion site, which may contribute to fixation failure. The posterior capsule and posterior band of the medial collateral ligament can been accessed and resected easily through any of the posterior approaches mentioned earlier. The anterior capsule may be released through the nonunion site (Fig. 23-5). Care should be taken to identify and protect the radial and median nerves at the time of the anterior capsular release. The anterior band of the medial collateral ligament and the lateral collateral ligament complexes should be preserved, along with the muscular attachments on the medial and lateral epicondyles, which are responsible for most of the blood supply to the distal segments.
Fixation Technique and Bone Grafting
The fixation technique that we recommend for internal fixation of distal humerus nonunions follows the same principles, objectives, and steps described for fixation of acute distal humerus fractures in the previous chapter (see Chapter 22).18 However, bone reabsorption at the nonunion site usually makes it difficult to apply compression at the supracondylar level if the reduction is anatomic, and the concept of metaphyseal shortening (see Chapter 22) often needs to be applied.12
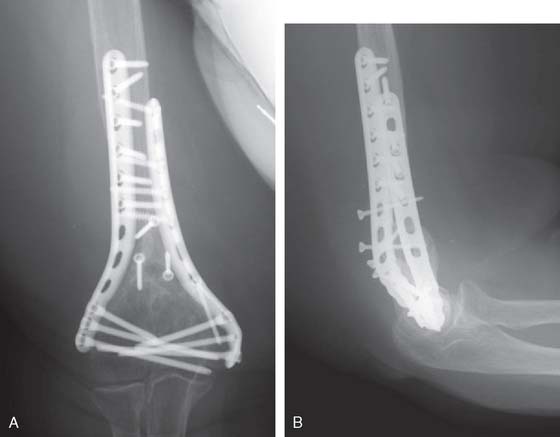
Two parallel plates are then applied medially and laterally, and fixed with multiple distal long screws, which most of the time will interdigitate and interlock, increasing the stability of the construct (Fig. 23-6). Compression at the nonunion site is achieved by a combination of maneuvers including the use of a large reduction clamp, proximal screw insertion in the compression mode, and slight undercontouring of the plates. Cancellous bone autograft or a bone graft substitute is then placed at the nonunion site to promote bone healing. Our preference is to fashion two thin corticocancellous plates from the iliac crest and fix them with one or more screws across the nonunion site on the medial and lateral columns (Figs. 23-6 and 23-7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree