CHAPTER 7 Nonoperative Management and Rehabilitation of the Hip
Introduction
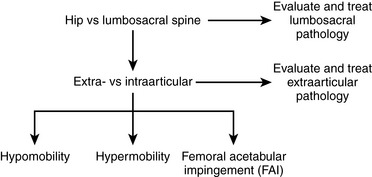
Evaluation algorithms and classification-based treatment systems are commonly used in the orthopedic community to assist with determining a diagnosis, prognosis, and intervention plan. An algorithm implemented during the patient evaluation allows for the systematic collection of information, whereas classification-based treatment defines subgroups of patients who are likely to respond to a specific treatment approach. A number of evaluation algorithms and classification-based treatment systems have been developed for various body regions; however, there are few that are specific to the hip. We have integrated an evaluation algorithm and classification-based treatment to help conservatively manage individuals with hip pain; this plan includes the consideration of the lumbosacral spine, the extra-articular soft tissue, and the intra-articular structures. Intra-articular pathologies are further divided to consider the issues of impingement, hypermobility, and hypomobility. An outline of our proposed algorithm can be found in Figure 7-1.
Lumbosacral spine
Examination and treatment with the mobilization of the lumbosacral complex are supported in the literature for individuals with hip pain. Cibulka and Delitto found that athletes with anterior or lateral hip pain and positive signs of sacroiliac joint dysfunction have a favorable treatment outcome with mobilization directed at the sacroiliac joint. The technique we use as an intervention for patients who we feel meet the criteria for the mobilization subgroup is depicted in Figure 7-2. The technique involves positioning the patient in a side-bending position toward and with rotation away from the painful side, with respect to the lumbar spine. A force directed anterior to posterior is applied to the ipsilateral anterior superior iliac spine with a Grade 5 thrusting maneuver. It should be noted that, before this manipulation is applied, contraindications for a thrust mobilization must be thoroughly cleared. The effect of this technique for reducing the patient’s hip pain is assessed. Depending on the amount of pain reduction and the results of reassessing previously positive signs, the evaluation can continue accordingly. In general, patients who fall into this category are also given lumbopelvic range-of-motion and stabilizing exercises. We find that patients with hip pain commonly have signs and symptoms that are consistent with this category and that they often positively respond to some degree to this mobilization technique.
Extra-articular soft-tissue disorders
The treatment of trochanteric bursitis with proximal ITB syndrome can involve a generic progression of therapy: decrease inflammation, improve the range of motion, increase strength, and return to activity. Proper ITB stretching is done with adduction, slight extension, and slight external rotation, as outlined in Figure 7-3. We also find benefit from the manual stretching depicted in Figure 7-4. It makes sense to incorporate components of both hip flexion and hip extension into the adduction stretch because of the attachments of both the tensor and gluteus maximus to the ITB. Other manual stretching, deep soft-tissue mobilization and massage, and other modalities may be indicated. We find that the most successful treatments include interventions that address more than the lateral hip pain and that also correct any biomechanical abnormalities and muscle imbalances.
Intra-articular pathology
Capsular laxity of the hip may be comparable with capsular laxity of the shoulder. Generally, individuals with this condition have engaged in repetitive forceful rotational activities. We commonly find that repeated forceful external rotation to the end of the range of motion causes iliofemoral ligament insufficiency. The logroll test typically demonstrates an increase in motion on the involved side as compared with the uninvolved side in these individuals. Treatment generally emphasizes strengthening the surrounding musculature and performing neuromuscular training and proprioceptive exercises. Patients with anterior hip laxity commonly elicit symptoms of instability with external rotation of the hip (e.g., when swinging a golf club). Exercises that reproduce these movements are avoided, whereas closed-chain activities with internal rotation are encouraged. We commonly use an exercise that incorporates the use of a resistive rubber cord, as depicted in Figure 7-5. During this exercise, it is important to maintain a neutral and stable pelvis to work the internal rotators and to engage the gluteus medius and the lumbopelvic stabilizers.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree