Neurovascular Injuries
Gregg R. Klein, Scott M. Sporer and Andrew M. Michael
Neurologic Injuries
Introduction
Neurologic injury is an uncommon but devastating complication following total hip arthroplasty (THA) that can delay patient recovery and postoperative physical therapy and can reduce quality of life; it is a leading cause of litigation following THA. With any hip procedure, there will be risk to surrounding neurovascular structures; however, with careful preoperative planning, knowledge of additional risks involved with each individual patient, and meticulous surgical technique, these risks can be minimized. It is important to diagnose and treat neurologic injury early after it has occurred and to know the likely outcomes to facilitate counseling of patients for an optimal recovery.
Neurologic injury can occur in the central or the peripheral nervous system, and it can be acute or delayed. Central nervous system injury following THA is usually the result of a vascular injury and most often is attributed to fat embolism syndrome following manipulation of the femoral canal. Peripheral nervous injury is more common after THA and can occur from a variety of insults intraoperatively, including damage from a retractor, incorrectly placed hardware, limb lengthening, or direct injury. Delayed peripheral nervous injury can be caused by a hematoma, compressive dressings, or patient positioning.1,2 The peripheral nerves most commonly injured following THA are the sciatic, femoral, superior gluteal, and obturator nerves.
Epidemiology and Risk Factors
Peripheral Nerve Injury
Peripheral neurologic injury following primary total hip arthroplasty (THA) has been reported to have a prevalence that ranges from 0.1% (1 palsy in 1287 cases) to 1.9% (7 palsies in 360 cases).2–4 The risk of nerve palsy following primary THA is increased if the indication for surgery is congenital hip dislocation or severe hip dysplasia, or if there is otherwise a need for a large degree of leg lengthening. Schmalzried and associates reviewed 3126 consecutive THAs and reported an overall rate of neurologic injury of 1.3% for diagnoses other than hip dysplasia, and 5.2% in patients receiving a primary THA for hip dysplasia (9 palsies in 172 cases).1 In the same study, nerve injury following a revision THA was reported to be 3.2%; however, this number has been reported to be as high as 7.5% in other series (5 palsies in 66 revision cases).2,5 Weber and colleagues performed preoperative and early postoperative electromyography (EMG) in 30 hips to determine the incidence of subclinical nerve injury following THA and found that the rate of asymptomatic injury may be as high as 70%.6
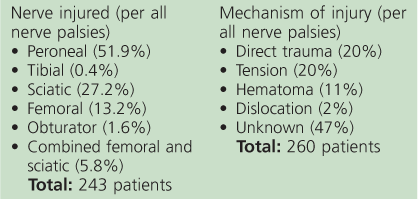
The nerves most frequently injured following THA are the sciatic, femoral, obturator, and superior gluteal nerves (Box 105-1). Peripheral nerve injuries generally occur in isolation; however, multiple nerve injuries can co-exist. Injury to the sciatic nerve remains the most common, accounting for up to 90% of all post-THA nerve palsies. The peroneal fibers of the sciatic nerve are affected in 94% to 99% of sciatic nerve injuries; up to 41% have tibial nerve involvement as well.1,2 However, isolated tibial nerve injury is rare, accounting for between 0.5% and 2% of sciatic nerve injuries, and isolated peroneal nerve injury accounts for between 47% and 65% of sciatic nerve injuries. The peroneal nerve is at increased risk owing to a combination of factors, including the density of nerve fibers at the hip, the proximity of the peroneal distribution to retractors (it lies lateral), and susceptibility to tethering or compression.7,8 Female sex, hip dysplasia, leg lengthening greater than 2.7 cm, revision surgery, a history of lumbar radiculopathy or peripheral neuropathy, excision of heterotopic bone, a deficient posterior wall, a posterior surgical approach, and the use of a cementless femoral implant increase the risk of sciatic nerve injury1,9-11 (Box 105-2). Lumbar stenosis and radiculopathy are important preoperative risk factors for nerve palsies and should be identified preoperatively because they can exacerbate intraoperative nerve damage through a double-crush phenomenon when impingement to the affected nerve proximally leaves it susceptible to damage at the surgical site.12 A history of lumbar spine disease should be noted in the preoperative visit because this may change the course or timing of treatment for postoperative nerve palsy.
The femoral nerve is the second most commonly injured nerve following THA, accounting for 13% of all peripheral nerve injuries (32 of 243 palsies).2 The most common cause of acute injury is thought to be direct compression by aberrant placement of a retractor anterior to the acetabulum. Increased risks of femoral nerve palsy include an anterior surgical approach, deficient anterior acetabular bone, and a previously released or absent psoas tendon. Expanding hematomas are found in up to 11% of patients with diagnosed nerve palsy and are the most common cause of delayed femoral nerve palsy. Schmalzried found that simultaneous femoral and sciatic nerve injury occurs together in 5.8% of nerve injuries.2
Superior gluteal nerve palsies may be increasing in prevalence owing to the use of a gluteal splitting approach for primary THA. The incidence of superior gluteal injury may be as high as 23% when a Hardinge approach is used.13 The exact incidence of superior gluteal nerve dysfunction is difficult to assess because patients present with abductor weakness or a limp that is common in the early postoperative period following uncomplicated THA.
Obturator nerve injury is extremely rare and accounts for 1.6% of all nerve palsies (4 of 243 palsies) with a prevalence of 0.016% among all cases (4 of 24,469 hips).2 Obturator nerve injury was probably more common when cemented acetabular components were routinely utilized, and cement that had extravasated into the obturator foramen was the main cause. Difficulty in diagnosis of this entity may contribute to its low reported incidence.
Central Nervous System Injury
Central nervous system injury is much less common than peripheral nervous system injury and is typically associated with fat embolism syndrome (FES). The incidence of FES following THA is not known, but it occurs in as many as 1% to 11% of the trauma population. Fat embolism syndrome is associated with femoral canal manipulation such as reaming, cementing, and implant impaction.14 In addition to FES, ischemic stroke was noted to occur in 3.9% of patients within 1 year of hip arthroplasty (67 cerebrovascular accidents [CVAs] in 1606 patients) in one large study. Ischemic stroke is associated with a number of factors, including history of atrial fibrillation, hip fracture, and previous history of stroke.15
Pathophysiology
Peripheral Nerve Injury
The pathogenesis of neurologic damage following THA differs depending on the nervous structure injured and the degree of injury (see Box 105-2). Three fundamental degrees of peripheral nerve injury have been identified: neuropraxia, axonotmesis, and neurotmesis. Neuropraxia is defined as loss of conduction in an intact nerve with an intact epineurium and neural sheath. It is often caused by disruption of blood flow or compression to the nerve. Axonotmesis is defined as disrupted axons within an intact sheath. Neurotmesis is defined as disruption of both the axon and the neural sheath. Patients with neuropraxia and axonotmesis often will go on to full recovery, whereas neurotmesis will often lead to partial or no recovery of neural function. Recovery from neuropraxia occurs early, and recovery from the other two is delayed because they must first undergo Wallerian degeneration. Each nerve is susceptible during certain surgical approaches and techniques and has different inherent risk factors that increase the probability of injury. It is crucial for the operating surgeon to anticipate these risks and take the necessary steps to avoid complications and counsel the patient.
Sciatic nerve palsies are the most common nerve injury following THA, and the peroneal division is most commonly affected.1,2 The likely mechanism of injury to this nerve varies according to the indication for THA, and whether it is a primary or revision procedure. Primary THA performed secondary to developmental dysplasia of the hip frequently results in limb lengthening and subsequent increased strain on the neurovascular structures. It has been conventionally believed that limb lengthening greater than 2.7 cm places the peroneal division at risk, and lengthening greater than 4.4 cm places the entire sciatic nerve at risk for injury.11 Stretching the nerve just 8% has been shown to reduce the blood supply to the nerve, and 15% stretch causes complete loss of blood flow.16,17 Stretching of 20% to 35% has been shown to cause functional nerve injury.17
Recent studies have shown that lengthening a congenitally shortened limb, as in developmental dysplasia of the hip (DDH), is associated with a higher risk of nerve palsy than a similar amount of lengthening in a patient with an acquired traumatic or degenerative hip who at one point had a limb and a nerve of normal length. This is most likely due to the development of a shortened sciatic nerve in the case of DDH, limiting the amount of leg lengthening that can be attained before excess tension is applied to the nerve.2 The anatomic location of the peroneal nerve, as well as its microanatomic properties, leaves it more susceptible to injury than the tibial division.
The peroneal division of the sciatic nerve lies lateral to the tibial division, making it more vulnerable to deep retractors during a posterior approach that can damage it by direct compression or increased tension along the nerve. It also has a relatively high density of nerve to connective tissue when compared with the tibial division2; this increases its susceptibility to mechanical injury because of the paucity of connective tissue available to absorb these forces. Finally, the peroneal nerve is anatomically susceptible to tension forces owing to its relative tethering at the sciatic notch and the proximal fibula.
Retractor injury to the sciatic nerve can be reduced by placing the posterior acetabular retractor between the bone and the hip capsule to reduce compressive forces to the nerve. Direct trauma can occur with posteroinferior acetabular screw fixation or, rarely, owing to scalpel, suture, or electrocautery injury. A hematoma may result in delayed sciatic nerve palsy caused by excessive internal compression. Excessive external compression from dressings or stockings (particularly at the fibular head) may result in a delayed neurologic injury.
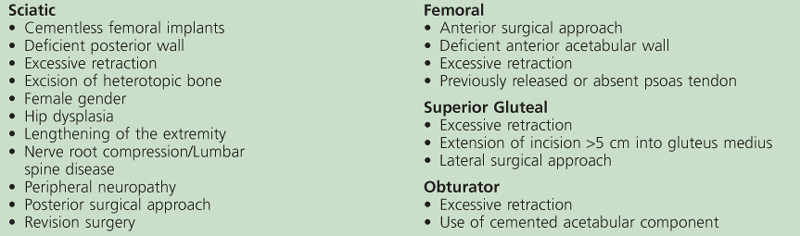
Injury to the femoral nerve is most common during an anterior or lateral approach to the hip.4 Acetabular retractors must be placed with care owing to the proximity and the sparse protection of the femoral nerve by the tendinous insertion of the iliopsoas. Special attention should be paid to avoid extracapsular or inferior placement of the anterior retractor because this aberrant positioning increases the risk of femoral nerve injury (Fig. 105-1). A deficient or released iliopsoas muscle can predispose the patient to femoral nerve injury through this mechanism. Anteroinferior acetabular screw placement can lead to direct trauma to the femoral nerve as well. Acetabular screws should be placed in the posterosuperior quadrant whenever possible, as described by Wasielewski and colleagues, to prevent nerve impingent secondary to hardware placement (Fig. 105-2).18 Delayed femoral nerve palsy is often attributed to compression from an expanding hematoma.
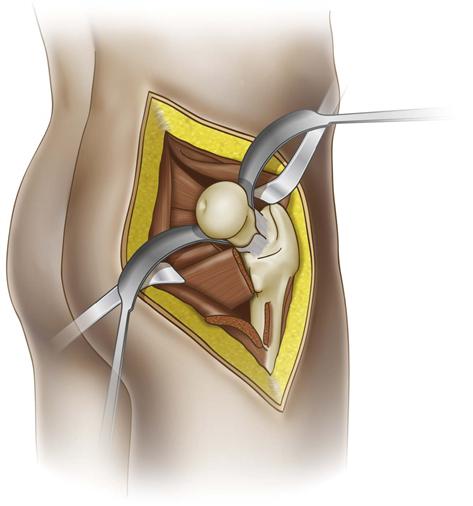
Figure 105-1 Correct acetabular retractor placement: Both anterior and posterior retractors are intracapsular. The anterior retractor is at the 1 o’clock position, and the posterior retractor is at the 7 o’clock position.
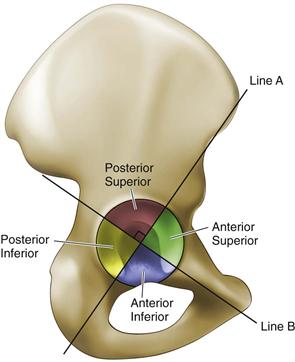
Figure 105-2 Quadrant system for safe placement of acetabular screws. The acetabular quadrant system can be used to identify the “safe zone” for screw fixation. Placing hardware in the posterior-superior quadrant minimizes neurovascular complications and is recommended for routine total hip arthroplasty (THA). ASIS, Anterosuperior iliac spine. (From Wasielewski RC, Cooperstein LA, Kruger MP, Rubash HE: Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty. J Bone Joint Surg Am 72:501–508, 1990.)
Obturator nerve injury is rare and difficult to diagnose. The most common reported cause of injury to this nerve is extravasation of cement through the obturator foramen. Other reported cases of obturator nerve palsy have cited excessive retraction and trauma from acetabular hardware such as anteroinferior screws and acetabular reinforcement rings.19
The superior gluteal nerve is susceptible to injury during a lateral approach to the hip, as described by Hardinge.13 This nerve is at risk for direct trauma when excisions are extended farther than 5 cm into the gluteus medius superior to the greater trochanter (Fig. 105-3). Cadaver studies have shown that the inferior branch of the superior gluteal nerve may be vulnerable to injury as close as 3 cm superior to the greater trochanter.13 The probability of damaging the superior gluteal nerve in a lateral approach is also increased with excessive retraction. Manual retraction has been shown to be safer than use of a self-retaining retractor.13,20 The cause of superior gluteal nerve injury is often confounded by normal postoperative abductor weakness, which frequently leads to a delayed diagnosis.
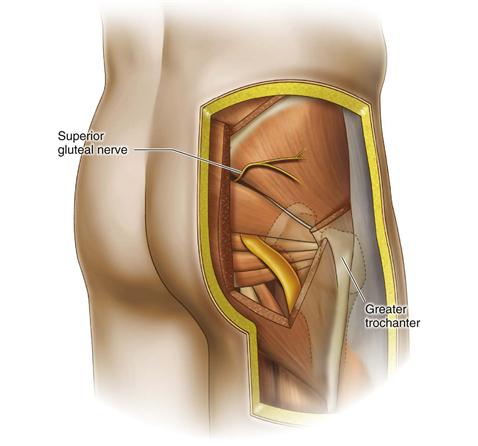
Figure 105-3 The superior gluteal nerve is susceptible to injury on the lateral approach to the hip if the incision is extended more than 5 cm superior to the greater trochanter.
Central Nervous System Injury
Central nervous system injury following THA is most often attributed to fat embolism syndrome. Fat embolism syndrome is caused by embolic fat globules from the bone marrow that travel to the lungs; this can lead to pulmonary failure and acute respiratory distress syndrome (ARDS). Paradoxical emboli are venous thrombi that travel through a patent cardiac septal defect and cause a cerebrovascular accident.21 In rare cases, the clot can travel elsewhere, blocking the blood supply to virtually any organ. It is associated most often with trauma but can occur after manipulation of the femoral canal in a THA, as in reaming, cementing, or implant impaction.22 Increased intramedullary pressure on the femur is a common cause of this entity; care should be taken when manipulating the medullary canal, although no known specific technique has been shown to reduce the incidence of fat embolism.14,22
Diagnosis
Peripheral Nerve Injury
Early clinical diagnosis is the key to successful treatment of neurologic injury following THA. A thorough physical examination must be performed, including testing of sensory and motor functions of all extremities and assessment of mental status during the preoperative visit. Preoperative radiographs can be helpful in estimating whether limb lengthening will be needed in the THA, prompting the surgeon to have a higher index of suspicion of nerve injury postoperatively. If excessive limb lengthening (greater than 2.7 cm) is anticipated, the operating surgeon must be prepared to take intraoperative measures to prevent nerve palsy.11,17 Subtrochanteric shortening may be indicated if the operating surgeon believes that tension on the sciatic nerve will be excessive, or if limb lengthening must exceed 2.7 cm to restore the native hip center. Patients who are at high risk for nerve palsies may be educated about the risks of the surgery to guide their postoperative expectations and recovery. Once the patient has recovered from anesthesia, a repeat thorough physical examination should be performed and clearly documented in the medical record. This allows the surgeon to immediately identify a change from the preoperative state and also provides a baseline for evolving neurologic injuries. Use of regional anesthesia may delay postoperative assessment of the operative limb; however, a complete physical examination should still be performed on all extremities in the immediate postoperative period, and again when the regional anesthesia has dissipated. The patient should be examined at least once a day for the remainder of the hospital stay and at follow-up visits to assess for delayed nerve injury. When nerve injury is diagnosed, the surgeon must assess for concomitant damage to other neurovascular structures and must evaluate the patient for a possible compartment syndrome.
Care should be taken to individually assess each nerve at risk when examining a patient (Table 105-1). Tibial and peroneal nerve distributions should be assessed individually when evaluating for sciatic nerve injury. The peroneal nerve can be assessed by placing the ankle in a neutral position and having the patient dorsiflex the ankle and extend the great toe. This must be done from a neutral position against resistance to minimize the confusion of ankle recoil from plantarflexion appearing as dorsiflexion. Patients may also be asked to evert the foot to test the superficial peroneal branch individually. Sensation in the peroneal nerve distribution can be assessed by testing light touch and sharp/dull differentiation to the dorsum of the foot, especially in the first dorsal web space. The tibial nerve can be assessed by once again placing the foot in a neutral position and asking the patient to plantarflex the ankle and flex the great toe. Sensation in the tibial nerve distribution can be tested through light touch and sharp dull differentiation on the plantar surface of the foot.
Table 105-1
Physical Examination Findings of Nerve Injury Following Total Hip Arthroplasty
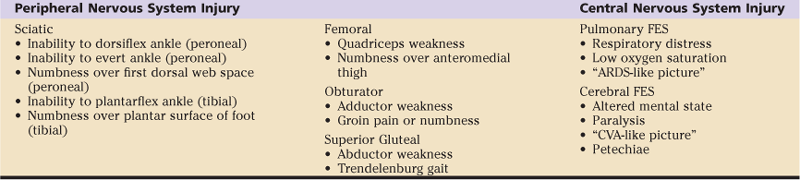
ARDS, Adult respiratory distress syndrome; CVA, cerebrovascular accident; FES, fat embolism syndrome.
Femoral nerve function can be examined most accurately by evaluating for knee extensor mechanism weakness and decreased sensation at the anteromedial aspect of the thigh or medial calf. If femoral nerve palsy is found in the immediate postoperative phase, it is most likely a result of retractor injury; however, an expanding hematoma remains the most common cause for delayed femoral nerve palsy.2 If a hematoma is suspected, serial hemoglobin levels and a coagulation panel should be collected, and the circumference of the upper thigh should be compared with the contralateral limb. Computed tomography (CT) scan or ultrasound may be useful in quantifying the size of the hematoma and in determining whether operative decompression is indicated.
Obturator nerve palsy following THA is difficult to diagnose owing to its rarity, its vague symptoms, and frequently a low index of suspicion. Patients who have consistent groin pain following hip surgery and a radiograph showing cement extravasation or inferior acetabular screws may be further evaluated. These patients may also have hip adductor weakness.
The diagnosis of superior gluteal nerve palsy is often confounded because of its similar presentation to normal postoperative limp or abducotr muscle avlusion. On physical examination, the patient will present with abductor weakness and a Trendelenburg gait. Suspicion should be high if these symptoms persist for more than three months postoperatively, particularly if a hardinge type approach to the hip was utilized. Electrophysiologic studies are helpful in confirming the diagnosis in any nerve palsy but are especially helpful when the diagnosis is unclear, as is often the case with obturator or superior gluteal nerve injury. Magnetic resonance imaging (MRI) with metal subtraction algorithms may have a role in differentiating between superior gluteal nerve palsy and abductor avulsion when the cause of the abductor weakness is unknown.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree