Fig. 10.1
Illustration highlighting the most common causes of cervical radiculopathy. (a) Bone spurs can occur along the articular facets which can impinge upon exiting nerve roots. (b) Thickening of the ligamentum flavum may also produce a mass effect that can encroach upon the dorsal root ganglion. (c) Disc herniation often occurs along the posterolateral aspect of the vertebral disc and may also irritate exiting nerve roots.
Fig. 10.2
Dermatome map of the upper extremity. Because the boundaries of dermatome maps often overlap, clinical correlation is needed before an interpretation can be made.
10.2.2 Physical Examination
Initial physical findings in patients with cervical spine pathology may include postural imbalances, such as changes in lordosis or forward head positioning, as a result of contracture of paravertebral and/or periscapular musculature. Shoulder muscle atrophy can also be an important clue since the innervation for many of the shoulder muscles are derived from the C5 and C6 nerve roots (especially the suprascapular nerve and the dorsal scapular nerve). Prominence of the scapular spine may indicate atrophy of the supraspinatus or infraspinatus muscles (innervated by the suprascapular nerve) and prominence of the medial scapular border with excessive lateral position of the scapula may indicate the presence of a lesion affecting the dorsal scapular nerve. Tenderness to palpation over the posterior aspect of the cervical spine may also indicate cervical pathology, especially when the pain radiates towards the shoulder; however, this is not always reliable [3]. Tenderness of the trapezius muscle is not reliable since this can indicate pathology of either the shoulder or the cervical spine; however, trapezius muscle wasting with lateral scapular winging suggests involvement of the spinal accessory nerve (Fig. 10.3).


Fig. 10.3
Clinical photographs of a patient with spinal accessory nerve palsy [4]. (a) The right trapezius muscle is visibly atrophied (arrow) when compared to the contralateral side. (b) When viewing from posteriorly, scapular winging can be seen during humeral elevation.
There are several methods by which physical examination can be used to differentiate between disorders of the shoulder or cervical spine. One method is to simply test the range of motion capacity of the neck and shoulder. Patients who demonstrate full, active, and painless neck range of motion and who demonstrate difficulty with isolated shoulder motion are more likely to have a shoulder condition as opposed to cervical spine pathology. The opposite would also be true for a patient with a disorder related to the cervical spine—that is, painful neck motion with normal shoulder motion. Provocative maneuvers are also designed to differentiate between disorders of the cervical spine and that of the shoulder girdle (see below).
10.2.2.1 Spurling’s Test
Spurling’s test [5] is performed by bending the neck laterally towards the affected shoulder. The examiner then applies a downward axial force (classically, ~7 kg) to the top of the head, thus narrowing the space for cervical nerve roots to exit the spinal cord (Fig. 10.4). Reproduction of neck and shoulder pain with this maneuver is suggestive of a cervical nerve root lesion. Other authors have suggested various modifications to Spurling’s original test, such as the addition of rotation and/or extension prior to applying a downward pressure to the top of the head [3]. L’hermitte’s sign, which also indicates cervical spine pathology, occurs when a “shooting” or “electric-like” pain propagates down the neck and down the ipsilateral arm with rotation or flexion of the neck without application of an axial load. Although a few studies have evaluated the validity of L’hermitte’s sign, these studies appear to have significant methodological flaws that hinder interpretation of their results [6, 7]. Thus, the value of L’hermitte’s sign to detect cervical spine pathology remains anecdotal at best.


Fig. 10.4
Spurling’s test. While sitting, the patient laterally bends the neck towards the affected shoulder. The examiner then applies a downward axial force to the top of the head (approximately 7 kg of force). This maneuver is thought to decrease the space available for cervical nerve roots to exit the spinal cord, thus reproducing the patient’s symptoms.
Shah and Rajshekhar [8] studied the reliability of Spurling’s test in the diagnosis of cervical disc disease with the reference standard of magnetic resonance imaging (MRI) in 25 patients who were treated nonoperatively and direct visualization at surgery in 25 patients who were treated operatively. The test was performed by extending and laterally bending the neck and then applying an axial load to the top of the head. The investigators did not rotate the head prior to application of an axial load. The sensitivity and specificity of Spurling’s test was found to range between 0.90 and 1.00, depending on whether MRI or surgery was used as the reference standard. In contrast, Wainner et al. [9] performed the same test; however, they also rotated the head towards the ipsilateral side before applying an axial load. In that study, they used electromyography (EMG) as the reference standard. The investigators calculated a sensitivity of 0.50 and a specificity of 0.93 for this version of Spurling’s test. In addition, Tong et al. [10] calculated an even lower sensitivity (0.30) when rotating the neck towards the contralateral shoulder. Combining the results of these three studies, it appears that lateral rotation of the neck decreases the sensitivity of the test for the detection of cervical radiculopathy. This rationale is supported by Anekstein et al. [11] who found the greatest sensitivity with the combination of lateral bending and extension without rotation. Thus, we prefer to perform the Spurling’s test in neutral rotation to improve diagnostic efficacy.
10.2.2.2 Shoulder Abduction Test
The shoulder abduction test is performed by simply having the patient abduct the humerus such that the hand is placed on the top of the head (Fig. 10.5). This maneuver is thought to increase the space available for the cervical nerve roots to exit the spinal cord, thus diminishing symptoms. A cadaveric study by Farmer and Wisneski [12] confirmed the theoretical rationale for the test. In their study, pressure transducers were placed within cervical foramina and pressure readings were recorded with the humerus and the neck in various positions. They found that extension of the neck produced the greatest intra-foraminal pressure while abduction of the humerus decreased this pressure, thus further solidifying this maneuver as a viable technique for the detection of cervical nerve root compression. Wainner et al. [9] later found that this maneuver was 17 % sensitive and 92 % specific for the detection of cervical spine-related pathology.


Fig. 10.5
Shoulder abduction Test. In a patient with suspected radiculopathy, asking the patient to place the palm of their hand on top of their head with the elbow pointed laterally may relieve their symptoms by increasing the space available for the cervical nerve roots to exit the spinal cord.
Farshad and Min [13] recently described an abduction extension test that was reported to have a sensitivity of 0.79 and a specificity of 0.98 in the detection of cervical nerve root compression. This test was performed by laterally abducting the humerus to 80° with the neck rotated towards the contralateral shoulder. With the patient in this position, an anteriorly directed pressure was applied to the posterior aspect of the humeral head (Fig. 10.6). Reproduction of symptoms was considered a positive test. In their preliminary cadaveric study using this maneuver, nerve roots were displaced by approximately 4–5 mm in all cases, potentially explaining the resulting high sensitivity and specificity values.


Fig. 10.6
Modified shoulder abduction test proposed by Frashad and Min [13]. In this test, the arm is laterally abducted to approximately 80° and the neck is bent and/or rotated towards the contralateral shoulder. While applying a gentle pressure to the posterior aspect of the humeral head, the examiner applies a gentle traction force along the axis of abduction.
10.2.2.3 Valsalva Maneuver
The Valsalva maneuver is performed with the patient in the seated position. The patient is then asked to take a deep breath and to “bear down” against a closed glottis for 2–3 s. This technique increases intra-abdominal pressure which, in turn, increases pressure within the thecal sac. The test is positive for cervical radiculopathy when neck and shoulder symptoms are reproduced. Wainner et al. found the sensitivity of this test to be only 0.22; however, the specificity was 0.94. Therefore, it is suggested to combine this test with a more sensitive test, such as Spurling’s test or the upper limb tension test (described below), to improve diagnostic accuracy.
10.2.2.4 Cervical Distraction Test
The cervical distraction test is performed with the patient in the supine position. The examiner cradles the jaw and occiput with their hands and slightly flexes the neck to improve patient comfort. A distraction force is applied gently and gradually until significant resistance is felt (classically, ~14 kg of force) (Fig. 10.7). This maneuver is thought to increase the space available for exiting nerve roots. Relief of symptoms indicates a positive test and is indicative of cervical pathology. Wainner et al. [9] determined that the cervical distraction test was 44 % sensitive and 90 % specific for the detection of cervical spine pathology. Similarly, Viikari-Juntura [3] calculated a sensitivity of 0.44 and a specificity of 0.97. Thus, similar to the Valsalva maneuver mentioned above, it is important to combine this test with other, more sensitive provocative maneuvers to improve diagnostic efficacy.


Fig. 10.7
Cervical distraction test. With the patient lying supine on the examination table, the examiner cradles the jaw and occiput with their hands. The neck is placed in a slightly flexed position and a gentle superiorly directed distraction force is applied (approximately 14 kg of force). This maneuver is also thought to increase the space available for exiting nerves.
10.2.2.5 Brachial Plexus Tension Test
The brachial plexus tension test was first described by Elvey [14] in 1986 and has been modified on a few occasions [9, 15]. Although less descriptive, some researchers refer to this maneuver as the “upper limb tension test.” The test is performed as a series of steps with the patient in the supine position. The first step is to place the hand over the posterior aspect of the scapula and to depress the scapula against the thoracic wall. Sequentially, the shoulder is then abducted, the forearm is supinated, the wrist and fingers are extended, the humerus is externally rotated, the elbow is extended, and the neck is bent towards the contralateral side and then towards the ipsilateral side (Fig. 10.8). Reproduction of the patient’s symptoms was considered a positive test. Wainner et al. [9] found that the sensitivity and specificity values for this test were 0.97 and 0.22, respectively. Quintner [15] found slightly lower sensitivity and specificity values; however, they used cervical radiography to confirm the diagnosis as opposed to EMG which was performed by Wainner et al. [9].


Fig. 10.8
Brachial plexus distraction test. With the patient supine, the examiner uses one hand to stabilize the scapula while the other hand is used to place the humerus in abduction and external rotation, the elbow extended, the forearm supinated, the wrist and fingers extended and the neck bent towards the contralateral shoulder. The neck is then slowly bent laterally towards the affected shoulder which may reproduce the patient’s symptoms.
As an adjunct to this test, Wainner et al. [9] proposed a second method to evaluate for cervical spine pathology. In this maneuver, the patient was positioned supine with the shoulder abducted to 30°. The examiner then sequentially depressed the scapula, internally rotated the humerus, extended the elbow, flexed the wrist and fingers and, finally, contralateral followed by ipsilateral side-bending of the neck (Fig. 10.9). Reproduction of the patient’s symptoms was considered a positive test. The sensitivity and specificity values for this maneuver were 0.72 and 0.33, respectively, representing an inferior result compared to Elvey’s original test described above.


Fig. 10.9
Modified brachial plexus distraction test. With the patient supine, the examiner uses one hand to depress the scapula while the other hand is used to place the humerus in 30° of abduction with internal rotation, extend the elbow, and flex the wrist and fingers. The neck is then laterally bent towards the contralateral shoulder. The neck is then slowly bent laterally towards the affected shoulder, potentially reproducing the patient’s symptoms.
10.3 Thoracic Outlet Syndrome
In 1956, Peet et al. [16] were the first to coin the term “thoracic outlet syndrome” (TOS) as a result of neurovascular compression between the anterior and middle scalene muscles (i.e., the interscalene triangle). It is one of the most controversial conditions in the orthopedic literature with regard to anatomy, diagnosis, and management. In 2004, Huang and Zager [17] reported that the incidence of TOS was approximately 3–80 cases per 1,000 people. This wide variability is likely due to misdiagnoses and confusing clinical presentations, especially since there are numerous conditions that can mimic TOS, such as brachial neuritis, peripheral nerve entrapments, and cervical spine disease among many other possibilities (Table 10.1).
Table 10.1
List of possible conditions that may mimic thoracic outlet syndrome
Conditions that can mimic thoracic outlet syndrome | |
|---|---|
Cervical radiculitis | Malignancy (e.g. spinal cord tumors) |
Brachial plexopathy | Shoulder pathology |
Fibromyalgia | Spastic disorders |
Angina/acute coronary syndrome | Raynaud’s phenomenon/disease |
Complex regional pain syndrome | Peripheral nerve entrapment |
Neurologic disorders | Vasculitides |
10.3.1 Pathogenesis
As the brachial plexus and subclavian vessels course towards the axilla and the upper arm, there are at least four areas of potential narrowing that can result in TOS. The first potential site of compression occurs in patients with a congenital bony or fibrous extension of the transverse process of the seventh cervical vertebra (cervical rib; Fig. 10.10) [18, 19]. The interscalene triangle is the second of these stenotic areas and is the most common site of compression (scalenus anticus syndrome; Fig. 10.11). The interscalene triangle is bordered by the anterior scalene muscle anteriorly, the middle scalene posteriorly, and the superiomedial aspect of the first rib inferiorly. The subclavian artery, subclavian vein, and the trunks of the brachial plexus are located within this triangle and is thus a potential site of neurovascular impingement. The costoclavicular space is the third site of narrowing and is located between the middle 1/3 of the clavicle and the first rib (costoclavicular syndrome; Fig. 10.12). Impingement in this area primarily involves the subclavian artery and/or vein. The fourth potential site of neurovascular compression is within the subcoracoid space in an area beneath the pectoralis minor muscle-tendon unit (pectoralis minor syndrome; Fig. 10.13).
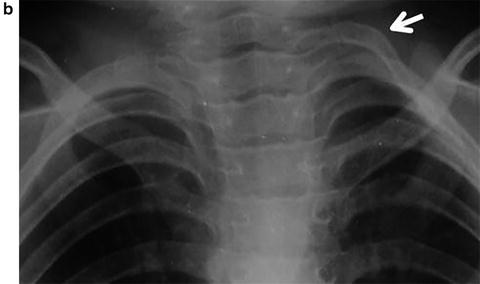
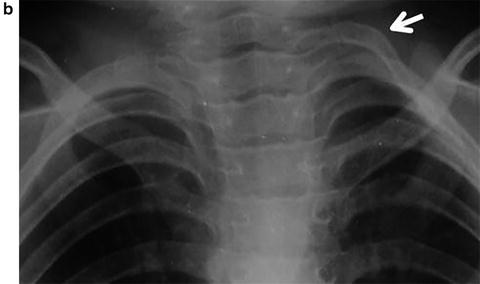
Fig. 10.10
Cervical rib. (a) Illustration depicting the anatomy of a cervical rib and its relationship with the nearby subclavian vessels and brachial plexus. (b) Radiograph demonstrating a cervical rib arising from the seventh cervical vertebra.
Fig. 10.11
Illustration depicting the interscalene triangle with the brachial plexus and subclavian vessels situated between the middle and anterior scalene muscles.
Fig. 10.12
Illustration of the contents of the costoclavicular space. Regardless of cause, compression of the neurovascular structures as they pass through the costoclavicular space can result in thoracic outlet syndrome. Vascular symptoms are most common when impingement occurs within the costoclavicular space.
Fig. 10.13
Illustration of the mechanism of neurovascular compression beneath the coracoid process and pectoralis minor tendon (within the subcoracoid space) as the humerus is maximally abducted (also known as pectoralis minor syndrome).
The numerous potential etiologies for TOS can be divided into static and dynamic causes. Static causes might include cervical ribs, fracture callus, fibrous bands, anomalous or fibrotic musculature (such as pectoralis minor syndrome [20, 21]), poor posture, and pathologic lesions with significant mass effect such as a Pancoast tumor, tuberculosis, or osteomyelitis. Reproduction of symptoms with scapulothoracic or glenohumeral motion typically indicates a dynamic cause which can occur within any of the three typically stenotic areas mentioned above. Repetitive microtrauma, as which occurs commonly in athletes and manual laborers, can also play an important role in the pathogenesis of TOS; however, the exact pathomechanism behind repetitive microtrauma and the development of TOS has not been clearly defined [21, 22].
The potential causes of TOS can also be divided by the structure involved. Neurogenic TOS, which has been reported to account for more than 95 % of all cases of TOS [23], involves compression of the nerves within the brachial plexus and is often the result of neck trauma. Vascular TOS, as the name suggests, involves compression of the subclavian artery and/or vein. Compression of the subclavian artery is typically associated with a cervical rib or rudimentary first rib [24, 25] (see Fig. 10.10). In contrast, compression of the subclavian vein usually occurs within the costoclavicular space [26] (see Fig. 10.12). Mixed TOS is more nonspecific and may involve compression of nerves, arteries, and/or veins simultaneously with varying magnitudes of compressive force.
Many patients with TOS report an aching sensation over the shoulder or neck accompanied by upper limb paresthesias such as numbness or tingling. Sensory dysfunction of the arm and/or hand often occurs simultaneously with occipital headaches. Compression of the subclavian vein may result in ipsilateral swelling and/or discoloration of the arm whereas compression of the subclavian artery can produce a subclavian bruit. Cold, pale skin distal to the elbow may indicate proximal compression of a sympathetic nerve. In reality, however, most patients with TOS present with vague symptoms that are often difficult to differentiate from other causes of shoulder pain.
10.3.2 Physical Examination
It is important to inspect the entire upper extremity, including the intrinsic muscles of the hand, for muscle atrophy, wasting, or fasciculations since these may suggest the presence of a neuropathy or myelopathy. Hoffman’s sign is a useful test for the detection of cervical myelopathy (Fig. 10.14). Combined supraspinatus and infraspinatus atrophy can occur since innervation for both of these muscles is derived from the C5 nerve root of the brachial plexus (suprascapular nerve). Weakness or atrophy of the rhomboid musculature may indicate compression of the dorsal scapular nerve (also from the C5 nerve root). The radial, median, and ulnar nerves are also derived from the brachial plexus, and care must be taken to evaluate the appropriate musculature to potentially locate the site of impingement. Tinel’s sign should also be performed to rule out cubital tunnel syndrome at the elbow and carpal tunnel syndrome at the wrist.


Fig. 10.14
Hoffman’s sign. The examiner gentle flicks the dorsum of the patient’s middle finger in a downward direction. Reflexive thumb flexion is a common indicator of cervical myelopathy.
There are several provocative maneuvers that can be used to help determine the site of impingement and the structure involved in TOS. However, interpretation of clinical tests for TOS is controversial and there is no individual test that is universally diagnostic. This is due to the wide variation in potential pathomechanisms involved with its development. In addition, the high false positive rate for many of these tests calls to question their application in clinical practice [27, 28]. Rayan and Jensen [27] found that 91 % of asymptomatic subjects developed symptoms from at least one of the tests designed to detect TOS.
10.3.2.1 Adson’s Test
Adson’s test was first described by Adson and Coffey [19] in 1927 as a method to assess for circulatory disruption due to a cervical rib. The test is performed with the patient sitting on the examination table. The radial pulse is then palpated prior to initiating the test. The patient is then asked to rotate the neck towards the affected shoulder, extend the neck, and to take a deep breath while the examiner simultaneously palpates the radial pulse (Fig. 10.15). When there is a decrease in pulse amplitude, the test is positive and indicates that the vascular component of the neurovascular bundle is being compressed within either the interscalene triangle or the costoclavicular triangle. Reproduction of paresthesias with this maneuver can also occur, indicating compression of a neural structure. However, in 1951, Adson [18] suggested that subclavian artery compression can also indicate compression and/or microtrauma of neural elements even in the absence of paresthesias.


Fig. 10.15
Adson’s test. In this test, the examiner first palpates the radial pulse to confirm adequate pulse amplitude. The patient is then asked to rotate the neck towards the affected shoulder and to inhale deeply. The examiner again palpates the radial pulse. A decrease in pulse amplitude suggests that proximal arterial compression, possibly at the interscalene triangle, may be causative of the patient’s symptoms.
Adson’s test has been reported to have a sensitivity between 0.79 and 0.94 and a specificity ranging from 0.74 to 1.00 [27, 29–32]. However, the studies by Nord et al. [31] and Plewa and Delinger [32] displayed conflicting results regarding the rate of false positives—Nord et al. [31] calculated a false positive rate of nearly 50 % while Plewa and Delinger [32] calculated a false positive rate of only 7 %. Several other authors have suggested that a positive test result may be associated with worse outcomes after either surgery or rehabilitation, especially in those with mixed neural and vascular symptoms [33, 34]. Clearly, it is important to consider the entire clinical picture before making the diagnosis of TOS using any physical examination maneuver. This includes a combination of the history, other physical findings and, potentially, imaging studies that serve to improve diagnostic accuracy [29, 35].
10.3.2.2 Halsted Maneuver
Dr. William Halsted was the first to identify and treat lesions of the subclavian artery due to the presence of cervical ribs in the late 1910s. The “Halsted maneuver” was developed to induce compression of the subclavian vessels and/or the brachial plexus within the costoclavicular space; however, the test is also purported to identify compression within the interscalene triangle and may be a useful adjunct to Adson’s test [36].
The Halsted maneuver is performed with the patient sitting on the examination table with the arms in a neutral position. The patient is then asked to extend the neck while the examiner simultaneously palpates the radial pulse at the wrist. A positive test occurs when the pulse amplitude decreases as the neck is extended and may indicate compression within either the interscalene triangle or the costoclavicular space (Fig. 10.16). The examiner can also apply gentle traction to the arm to help elicit symptoms. An MRI study by Demirbag et al. [35] found that the Halsted maneuver produced a significantly decreased distance between neurovascular structures and the inferior border of the clavicle within the costoclavicular space. Although this test has been widely referenced in the literature, there have been no clinical studies that have evaluated the validity or reliability of the test for diagnosing TOS.


Fig. 10.16
Halsted maneuver. This test is performed exactly as described for Adson’s test; however, rather than rotating the neck, the neck is extended posteriorly. Compression is thought to occur either at the interscalene triangle or the costoclavicular space.
10.3.2.3 Costoclavicular Test
Compression of the subclavian vessels within the costoclavicular space was first described in 1943 by Falconer and Weddel [37]. They described a maneuver in which the sitting patient was asked to retract the scapulae and flex the cervical spine, bringing the chin towards the chest. The examiner simultaneously palpated the radial pulse (Fig. 10.17). A decrease in pulse amplitude during this test indicated that compression of the neurovascular structures between the clavicle and the first rib was likely. Falconer and Weddel [37] found a 60 % false positive rate indicating that this maneuver may cause compression even in the absence of predisposing anatomy. Similarly, Telford and Mottershead [38] found radial pulse diminution in 68 % of normal subjects after shoulder retraction. Although this technique has been used extensively, there have been no studies that have evaluated its actual sensitivity or specificity in the diagnosis of TOS.


Fig. 10.17
Costoclavicular test. In this test, the patient is asked to maximally retract the shoulders and to simultaneously bend the neck into forward flexion. The radial pulse is palpated both before and after this positioning. Compression is thought to occur within the costoclavicular space.
10.3.2.4 Wright’s Test
In 1945, Wright [39] described the diminution of the radial pulse in 93 % of 150 asymptomatic individuals with the arm hyperabducted to an overhead position and the elbow flexed to 90° (Fig. 10.18). He suggested this finding was the result of axillary artery compression beneath the pectoralis minor tendon within the subcoracoid space (see Fig. 10.13). Along with Raaf [40], Gilroy and Meyer [41] also found positive results in up to 70 % of asymptomatic volunteers. Rayan and Jensen [27] suggested that positive symptoms could be the result of ulnar nerve compression behind the medial epicondyle since the original description of the test involved flexion of the elbow. They proposed that the test be performed with the elbow extended; however, they did not evaluate the reliability or validity of this technique. Tanaka et al. [42] performed a study in which nerve contact pressures were measured with different tests for TOS in a series of eight cadavers without a history of TOS. They found that Wright’s test induced the greatest amount of nerve compression compared to any of the other tested positions, further implying that nerve compression in the hyperabducted position may be a normal phenomenon—a concept that was originally suggested by Roos [43] in 1976.


Fig. 10.18
Wright’s test. With the elbow flexed to 90°, the humerus is maximally abducted to an overhead position. Reproduction of symptoms may indicate neurovascular compression beneath the coracoid and pectoralis minor tendon.
10.3.2.5 Roos Test
Roos [43] also developed a test designed to detect vascular compression at the level of the brachial plexus. In this test, the humerus is flexed to 90° and externally rotated with the elbow also flexed to 90°. The patient is then instructed to repeatedly open and close the fist at moderate speed for approximately 3 min (Fig. 10.19). Reproduction of symptoms within the 3-min interval indicates a positive test. However, this test has also been reported to produce a high rate of false positives on at least one occasion [32]. The sensitivity of this test has been reported to range from 0.52 to 0.84 with a specificity between 0.30 and 1.00 [27, 29, 31, 32, 44, 45].


Fig. 10.19
Roos test. With the arm in the 90/90 position (90° of abduction, 90° of external rotation with the elbow flexed 90°), the patient is asked to rapidly open and close their fist for a minimum of 3 min. The clinical utility of this test has not been firmly established.
10.4 Quadrilateral Space Syndrome and Axillary Neuropathy
10.4.1 Pathogenesis
There are numerous potential etiologies of axillary nerve palsy, many of which occur as a result of blunt trauma, iatrogenic injury, or nerve compression. The axillary nerve branches from the C5–C6 nerve root and courses towards the quadrilateral space, passing just inferior to the subscapularis and anteroinferolateral to the inferior glenoid rim. The quadrilateral space, as the name suggests, is bordered by four structures—namely, the teres minor superiorly, the teres major inferiorly, the proximal humerus laterally, and the long head of the triceps medially (Fig. 10.20). The posterior circumflex humeral artery, a branch of the axillary artery, travels with the axillary nerve through the quadrilateral space. Compression of the neurovascular bundle within this space, termed the “quadrilateral space syndrome” by Cahill and Palmer [46] in 1983, can occur from anomalous fibrous bands, traumatic scarring, mass lesions, glenolabral cysts, large humeral head osteophytes, and/or muscle hypertrophy [47–51]. Cahill and Palmer [46], along with McKowen and Voorhies [52], observed that axillary nerve compression within the quadrilateral space commonly occurred with the humerus in a hyperabducted and externally rotated position (such as which occurs during the throwing motion). Although uncommon, this position may also cause arterial compression more proximally where the axillary artery travels beneath a hypertrophied pectoralis minor muscle, potentially resulting in thrombosis and distal embolization [53–56].
Fig. 10.20
(a) Illustration depicting the anatomy of the quadrilateral space. See text for anatomic description. (b) Illustration showing the narrowing of the quadrilateral space as the arm is abducted to approximately 90° in the coronal plane.
10.4.2 Physical Examination
Quadrilateral space syndrome typically presents as a vague posterior or lateral pain over the dominant shoulder of young, athletic individuals. Patients may also complain of night pain and mild weakness, especially with forward elevation and/or abduction. The presence of paresthesias over the lateral deltoid is not uncommon and strongly indicates axillary nerve involvement. Aside from these typical complaints, other historical findings are largely nonspecific and generally do not contribute to the diagnosis.
Although physical examination findings are nonspecific in many cases, it is most important to rule out other, more common causes of shoulder pain such as rotator cuff tears and labral lesions, especially in overhead throwing athletes. Tenderness to palpation directly over the quadrilateral space may occur with concomitant weakness and/or atrophy of the posterior deltoid. This finding should alert the clinician to the potential for neurovascular compromise within the quadrilateral space.
Provocative maneuvers for the diagnosis of quadrilateral space syndrome are rarely reported; however, there are a few techniques that can be used to piece together the diagnosis. Although not always present, the deltoid lag sign may indicate posterior deltoid weakness (see Chap. 3), and the Hornblower’s sign (see Chap. 4) may indicate concomitant weakness of the teres minor muscle (both the deltoid and the teres minor muscles are innervated by the axillary nerve). In addition, abnormal sensation may be noted over the lateral deltoid since the sensory branch of the axillary nerve provides innervation to the skin overlying this area. Some authors suggest that forward flexion, abduction, and external rotation of the humerus can reproduce symptoms when the position is held for approximately 2 min; however, this method has not been evaluated in the literature [48]. Because of vague presenting signs and symptoms, a high index of suspicion is needed to correctly diagnose quadrilateral space syndrome by physical examination. Subclavian arteriography demonstrating stenosis or blockage of the posterior circumflex humeral artery with the arm abducted and externally rotated is thought to confirm the suspected diagnosis even though most patients do not have vascular symptoms [46].
10.5 Brachial Neuritis
Brachial plexus injuries, although most commonly idiopathic, have been reported to result from inflammation, trauma, malignancy, and even excessive radiation [49, 57–59]. Parsonage and Turner [60] first described these disorders in 136 patients, labeling the condition as “neuralgic amyotrophy.” Others have labeled the condition as a brachial radiculitis, neuropathy, neuritis and, most commonly, Parsonage–Turner syndrome.
10.5.1 Pathogenesis
Several types of brachial neuritis exist and differ in clinical presentation depending on the most likely cause. These include idiopathic, hypertrophic, hereditary, and traumatic types.
Idiopathic brachial neuritis is most commonly asymmetric (bilateral in 1/3 of cases [58]) and affects men more than women at a rate of at least 2:1 [49]. The condition typically has a bimodal age distribution, occurring most commonly in patients in their 20s and 60s [58]. Approximately half of patients report preceding events such as flu-like symptoms [59], recent vaccination [61, 62], and/or recent surgery [63] in the days just prior to the onset of symptoms, leading some to believe the condition may be immune-modulated [58]. Pierre et al. [64] demonstrated oligoclonal banding consisting of elevated IgG titers against herpes simplex and varicella zoster viruses in the cerebrospinal fluid of patients with brachial neuritis. Biopsies of the brachial plexus have also revealed mononuclear infiltrates, further suggesting an immunological basis for the disease [65, 66]. In addition, treatment with immune-modulating drugs such as corticosteroids and IVIg has been helpful on occasion [67–71].
Hypertrophic brachial neuritis has an unknown cause; however, its features differ from that of the above condition in that evidence of demyelination is evident on histologic examination, similar to other demyelinating diseases such as Gullain–Barre syndrome [72, 73]. Signs of generalized polyneuropathy, however, are absent. In addition, brachial plexus edema manifests as an enlarged appearance on MRI that suggests the diagnosis of hypertrophic brachial neuritis (Fig. 10.21) [58, 74].










