Neglected Calcaneal Fractures
George T. Liu
Calcaneal fractures represent 2% of all fractures of the body and 60% of all tarsal bone fractures of the lower extremity (1,2). These fractures often occur from high-energy trauma, such as a fall from height or motor vehicle collision. Up to 84% of calcaneal fractures are intra-articular and are associated with concomitant loss of height, increased width, and varus malalignment of the calcaneal tuberosity (3).
Treatment of displaced intra-articular fractures of the calcaneus remains controversial. Though short-term studies demonstrate favorable outcomes with operative management of displaced calcaneal fractures (4,5,6,7,8 and 9), long-term studies show little functional improvement between operative and conservatively treated calcaneal fractures (3,10,11 and 12). However, calcaneal fractures that are managed nonoperatively are five to six times more likely to require a subtalar joint arthrodesis due to posttraumatic arthritis (3,13). Other variables that predict the likelihood for subtalar joint arthrodesis following nonoperative management of calcaneal fractures include workman’s compensation status (3 times), Sanders 4 classification (5 times), and Böhler’s angle less than 0 degrees (11 times) (13).
Preservation of the native architecture of the calcaneus affects overall outcome of subtalar joint arthrodesis. When late-stage subtalar joint arthrodesis for posttraumatic arthritis is required, improved functional outcome is seen in patients who initially underwent an open reduction internal fixation for a displaced calcaneal fracture compared with displaced calcaneal fractures that were initially treated conservatively requiring deformity correction with arthrodesis of the arthritic subtalar joint (14).
Displaced calcaneal fractures may often be managed nonoperatively due to misdiagnosis, surgeon’s lack of familiarity with operative method, or concern for potential complications associated with operative intervention. Though operative complications may be averted with conservative treatment, the likelihood of developing a symptomatic malunion from a displaced calcaneal fracture is high. The resultant calcaneal malunion can produce pain and disability from loss of hindfoot and ankle motion, posttraumatic arthritis, and angular deformity. Most calcaneal fracture malunions often require subtalar joint arthrodesis to address the symptomatic arthritis but may also require restoration of the talocalcaneal alignment to achieve a satisfactory functional result.
ANATOMY, PATHOMECHANICS, AND EVALUATION
Patient with a neglected calcaneal fracture may present with complaints of pain due to two component problems: arthritis and deformity. Intra-articular malunion of the subtalar joint of the calcaneus is associated with altered joint contact pressures and symptomatic arthritic changes seen as early as 2 years (15,16 and 17). Loss of calcaneal height and flattening of the talar declination angle result in altered alignment of the subtalar joint axis, which leads to locking of the transverse midtarsal joint in supination and overload to lateral column of the foot (18,19). Loss of the talocalcaneal angle causes anterior ankle impingement from loss of available dorsiflexion (18) (Fig. 112.1). Varus malalignment of the calcaneal tuberosity also decreases available subtalar joint eversion, which diminishes shock absorption capacity of the foot during heel strike. Lastly, heel widening from the expansion of the lateral wall of the calcaneal fracture may be associated with peroneal tendinopathy and subfibular impingement (20,21).
CLINICAL EVALUATION
Foot pain in neglected calcaneal fractures may be intra- or extra-articular in origin. Lateral foot pain and loss of hindfoot eversion may be caused by calcaneofibular impingement, peroneal tendonitis, or posttraumatic arthritis of the subtalar joint. Examination may reveal pain along the peroneal tendons accentuated with diminished ability to plantarflex the first ray and evert the foot. Pain in the sinus tarsi may indicate subtalar joint pathology, most likely arthritis. A diagnostic injection into the posterior facet of the subtalar joint may help distinguish between articular versus nonarticular source of pain. Subtalar joint often reveals decreased range of motion. Fracture extension into the calcaneocuboid joint may produce arthritic pain to the lateral midfoot, which may be elicited with direct palpation and range of motion of the transverse midtarsal joint. The increased width of the heel may cause tighter shoe fit and sural nerve irritation (Fig. 112.2). Sural nerve pathology should be suspected in patients who report paresthesias, particularly burning or numbness, along the lateral aspect of the foot. Palpation or percussion of the sural nerve may produce a Tinel sign.
Pain along the anterior ankle is commonly caused by anterior tibiotalar impingement from loss of talar declination and calcaneal height. With loss of available dorsiflexion of the tibiotalar joint, the talar neck impinges against the anterior lip of the tibial plafond. The patient will often complain of difficulty dorsiflexing the ankle with walking or negotiating stairs. Forced dorsiflexion of the ankle may often reproduce pain (22).
Injury to the plantar heel fat pad or fracture to the calcaneal tuberosity may cause persistent plantar heel pain. Atrophy of the plantar fat pad may be observed on examination of the heel.
 Figure 112.1 Subtalar joint depression fracture of the calcaneus results in loss of calcaneal height, talar declination, and available dorsiflexion of the tibiotalar joint. |
Though less frequently occurring, expansion of the medial calcaneal wall may occur, causing scarring and impingement of the flexor hallucis longus tendon. Pain to the medial hindfoot may be reproduced with excursion of the flexor hallucis longus with passive range of motion at the level of the first metatarsophalangeal joint. Medial wall expansion may cause bony impingement against the posterior tibial nerve. Tarsal tunnel syndrome should be considered if patients report paresthesias to the medial heel and the sole of the foot. Percussion of the posterior tibial nerve may elicit a Tinel sign.
Hindfoot varus malalignment as well as limb-length discrepancies may be identified with the standing evaluation of the lower extremity.
Asymmetric limb length and hindfoot pain may produce an antalgic gait with altered cadence.
RADIOGRAPHIC EVALUATION
Radiographic studies are used to identify relative position and angulation of the calcaneus to the talus and tibia.
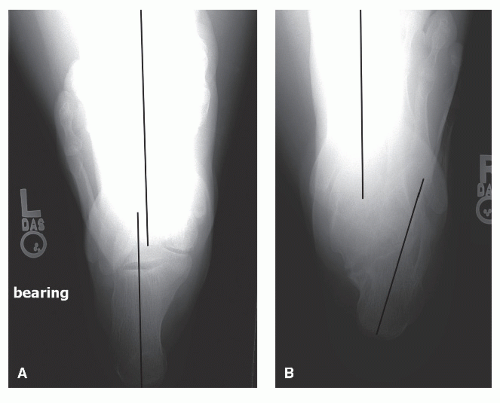
Bilateral weight-bearing radiographic studies, particularly of the uninjured foot, are necessary for comparison and to guide deformity correction. Standing bilateral calcaneal axial views of the calcanei can identify the level of varus or valgus angular deformity between the middiaphyseal axis of the calcaneus and the middiaphyseal axis of the tibia (Fig. 112.3). The middiaphyseal axis of the calcaneus should be parallel and slightly lateral to the middiaphyseal axis of the tibia (23). The Böhler’s angle and the critical angle of Gissane are two primary radiographic references from the lateral views of the calcanei used in correction of calcaneal deformities. The Böhler’s angle is measured between the intersection of the line extending from the superior portion of the calcaneal tuberosity to the most superior point of the posterior facet and a second line from this point to the anterior process of the calcaneus. Normal Böhler’s angle is 20 to 40 degrees (24). The critical angle of Gissane is formed by the convergence of a line drawn from the posterior facet of the subtalar joint and a second line from the anterior process of the calcaneus. The normal critical angle of Gissane is approximately 90 to 105 degrees (25). Decrease in the Böhler’s angle and increase in the critical angle of Gissane is seen in the lateral view (Fig. 112.4). Weight-bearing bilateral lateral views can identify calcaneal height needed to alleviate anterior tibiotalar impingement (Fig. 112.5). Presence of subtalar joint pathology of the posterior facet can be visualized with Broden’s views (Fig. 112.6). Ankle mortise view can be useful in identifying subfibular impingement.
Computed tomography may be obtained to further define the degree of arthritic changes within the subtalar and calcaneocuboid joint, hindfoot alignment, lateral wall prominence, and subfibular impingement. Additionally, computed tomography three-dimensional reconstruction with rendering software may assist in preoperative planning of complex multilane calcaneal fracture malunions.
INDICATIONS FOR REALIGNMENT ARTHRODESIS OF THE SUBTALAR JOINT AND PERIARTICULAR OSTEOTOMIES
Deformity correction to reestablish the anatomic relationship between the calcaneus and the talus, realignment of the tibial middiaphyseal and calcaneal middiaphyseal axes, and arthrodesis of the arthritic subtalar joint are procedures needed to restore satisfactory limb function. Restoring height of the calcaneus and correcting hindfoot alignment can oftentimes be achieved at the subtalar joint level. In cases of severe deformity, periarticular calcaneal osteotomies may be needed to realign the anatomic axis of the calcaneus to the tibia or improve anatomic positioning between talus and calcaneus.
LATERAL WALL DECOMPRESSION
Lateral wall decompression may be performed if lateral calcaneal exostosis is causing peroneal tendon or subfibular impingement. Concomitant peroneal tenolysis should be performed. The lateral exostosis may be accessed through
a lateral extensile, posterolateral approach, or through a lateral extensile hockey-stick incision. Lateral wall decompression has been successful in cases of calcaneal fracture malunion with isolated lateral wall exostosis and minimal subtalar arthrosis (26).
a lateral extensile, posterolateral approach, or through a lateral extensile hockey-stick incision. Lateral wall decompression has been successful in cases of calcaneal fracture malunion with isolated lateral wall exostosis and minimal subtalar arthrosis (26).
SUBTALAR JOINT-LEVEL CORRECTION
Subtalar Joint In Situ Arthrodesis
In situ arthrodesis of the subtalar joint may be performed in patients with symptomatic arthritis without loss of calcaneal height or varus deformity of the heel. Additionally, a patient who has neither pain nor restriction with ankle dorsiflexion may be considered for this procedure. In situ arthrodesis of the subtalar joint for posttraumatic arthritis is associated with greater than 90% fusion rates, improved function, decreased pain, and low rate of complications (22,26,27,28 and 29).
Distraction Arthrodesis with Structural or Nonstructural Bone Graft
Distraction arthrodesis of the subtalar joint with structural bone block or nonstructural bone graft is considered in patients with loss of calcaneal height, anterior ankle impingement from decreased talar declination, and posttraumatic
arthritis of the subtalar joint. Restoration of calcaneal height and talar declination can alleviate symptomatic anterior tibiotalar impingement (22). Varus deformities of the calcaneus may be corrected provided the center of angulation of the deformity is at the level of the subtalar joint. Results of distraction arthrodesis of the subtalar joints for joint depression fracture malunions of the calcaneus have been associated with satisfactory fusion rates, good functional outcomes, and restoration of both calcaneal height and talocalcaneal relationship (18,30,31,32 and 33).
arthritis of the subtalar joint. Restoration of calcaneal height and talar declination can alleviate symptomatic anterior tibiotalar impingement (22). Varus deformities of the calcaneus may be corrected provided the center of angulation of the deformity is at the level of the subtalar joint. Results of distraction arthrodesis of the subtalar joints for joint depression fracture malunions of the calcaneus have been associated with satisfactory fusion rates, good functional outcomes, and restoration of both calcaneal height and talocalcaneal relationship (18,30,31,32 and 33).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree