Neck Pain
Jerome Van Ruiswyk
 |
A 62-year-old man presents with chronic neck and left arm pain that have been getting progressively worse over the last 2 years. The pain radiates down to the left forearm and up into the head; he does admit some associated numbness in the left hand and occasionally in the right hand. He denies bowel or bladder incontinence but feels that his sense of balance has been off for years. He has a history of prior lumbar decompression for lumbar spinal stenosis and radiculopathy.
On examination, he has diminished light touch sensation on the dorsum of the left forearm and hand. Strength in the arms is 5/5 in the deltoids, biceps, triceps, and handgrip. Deep tendon reflexes in the arms and legs are normal except the left biceps is 3+. Hoffman’s reflex is negative. There is no ankle clonus.
A magnetic resonance imaging of the cervical spine shows severe multilevel degenerative disc disease with broad-based disc protrusion at C3-C4 resulting in spinal cord deformity (see image), severe foraminal narrowing at bilateral C5, left C7, and bilateral C8 nerve roots. Electromyogram shows a chronic neurogenic lesion affecting the left C7 nerve root.
He is initially managed conservatively. However, 3 months later he presents with a worsening of symptoms with numbness and tingling in both arms and hands that is exacerbated by movement of his neck. He continues to deny bowel or bladder incontinence. His neurologic examination is unchanged except that he now has a positive Hoffman’s reflex in the right arm.
Because of progression of symptoms and subtle signs of myelopathy, he undergoes posterior cervical decompression and fusion. Postoperatively, his neurologic symptoms abate, but his pain continues, and his neurologic examination continues to show diminished light touch sensation on the dorsum of the left hand and 5/5 motor strength in both arms except for 4+/5 motor strength in the left wrist extensors and triceps.
Clinical Presentation
Neck pain is a common presenting complaint in primary care settings. Studies suggest that up to two thirds of individuals experience neck pain at least once during their lifetime. The prevalence of neck pain increases with age and is more common in women than in men. Although up to 10% of the adult population has neck pain at any one time, most neck pain is self-limited. Consequently, patients seeking care for neck pain tend to have more severe pain, other associated symptoms, or chronic symptoms that have not responded to rest or over-the-counter analgesics; or they report neck pain as a secondary symptom of a more generalized condition. Those patients seeking care with neck pain as a primary complaint tend to have symptoms bothersome enough to cause functional limitations. Functional classification systems such as the World Health Organization’s International Classification of Functioning, Disability, and Health (ICF) can be used to more fully describe patient impairments.
Multiple-risk factors for neck pain have been identified (1) including increasing age, obesity, smoking, unusual postures, and heavy lifting or
other heavy work. However, an even greater number of psychosocial factors have been associated with neck pain including depression, drug abuse, low job satisfaction, monotonous or dissatisfying work, lack of coworker support, and lack of control over the work situation. Psychosocial and cultural factors can also impact the prevalence and natural history of neck pain. For example, in Australia, after legislation removed financial compensation for pain and suffering from whiplash injuries, subsequent whiplash patients reported lower pain scores and better functional outcomes compared with historical controls (2). Interestingly, in Lithuania where there is no legal tort system, late whiplash syndrome does not exist (3).
other heavy work. However, an even greater number of psychosocial factors have been associated with neck pain including depression, drug abuse, low job satisfaction, monotonous or dissatisfying work, lack of coworker support, and lack of control over the work situation. Psychosocial and cultural factors can also impact the prevalence and natural history of neck pain. For example, in Australia, after legislation removed financial compensation for pain and suffering from whiplash injuries, subsequent whiplash patients reported lower pain scores and better functional outcomes compared with historical controls (2). Interestingly, in Lithuania where there is no legal tort system, late whiplash syndrome does not exist (3).
Clinical Points
Patients presenting with neck pain can represent a diagnostic challenge because of an extensive differential diagnosis that includes emergent and serious underlying conditions.
Patients with a history of trauma and those with possible myelopathy, infection, or malignancy should have further prompt evaluation with imaging.
Because of the poor correlation of imaging findings with symptoms, it can be difficult to localize neck pain to a specific anatomic source.
Diagnostic specificity in the evaluation of neck pain relies on recognition of patterns of symptoms, signs, and test results since a high proportion of asymptomatic patients will have degenerative changes on imaging.
Patients without underlying spinal instability, infection, cancer, or myelopathy can initially be managed conservatively.
When evaluating neck pain, the history should include the elements of all basic pain histories including location, severity, quality, onset, duration, aggravating and alleviating factors, radiation, history of injury or overuse, any associated symptoms especially neurologic or constitutional symptoms, chronic and prior conditions especially infections or malignancy, common work or leisure activities and any recent unusual activities, and response to prior interventions or treatments.
In clinical practice, patients present much more commonly with posterior neck pain than with anterior neck pain. The most common ICD-10 codes specifically associated with neck pain include cervicalgia (M54.2), sprain and strain of cervical spine (S13.4), spondylosis with radiculopathy (M47.2), cervical disc disorder with radiculopathy (M50.1), and cervicocranial syndrome (M53.0).
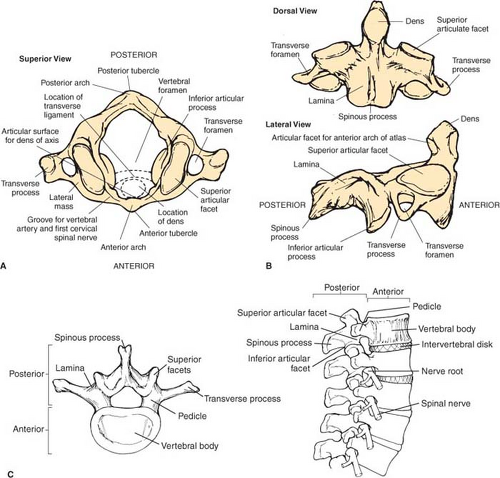
The neck is the most flexible part of the spinal column. The less rigid bony structure that allows this flexibility, particularly the unique structure of C1 and C2, means that the neck must rely more heavily on soft tissue structures for support which contributes to the pathophysiology of some important cervical spine conditions. The atlas (C1) is a ring without any vertebral body (Fig. 2.1A). The superior lateral bodies of the atlas articulate with the occipital condyles to form the atlanto-occipital joint, which is responsible for about 50% of the flexion and extension in the neck. The axis (C2) more closely resembles the remainder of the vertebrae with a vertebral body, ring, and prominent spinous process (especially noticeable on lateral cervical spine x-rays), but it also has an odontoid process or dens projecting superiorly off its vertebral body (Fig. 2.1B). A transverse ligament holds the dens to the anterior arch of the atlas; this functional peg-in-hole joint provides about 50% of the rotation of the neck. Inflammation of the synovial joint that articulates the axis to the atlas, from conditions such as rheumatoid arthritis, can damage this ligament leading to subluxation of the C1-C2 joint. Radiologic evidence of C1-C2 subluxation can be seen on flexion–extension views of 20% patients with rheumatoid arthritis. Therefore, screening lateral flexion–extension x-rays should be obtained during preoperative evaluation of patients with rheumatoid arthritis who will be undergoing endotracheal intubation.
The remainder of the cervical vertebrae have standard vertebral anatomy with a body, a posterior arch that provides bony protection for the spinal cord and with intervertebral discs between the vertebral bodies of all the remaining cervical vertebrae (Fig. 2.1C). The intervertebral disc has an outer annulus fibrosis and an inner nucleus pulposus with superior and inferior end plates. The gelatinous nucleus pulposus acts as a shock absorber for compressive forces, whereas the annulus fibrosis acts as a fibrous sheath restraining the nucleus pulposus. When rents occur in the annulus fibrosis, the inner nucleus pulposus may protrude or be partially extruded; when the resulting bulge occurs in a posterolateral location it may compress a nerve root, and when it occurs in a posterior midline location it may compress the anterior spinal cord. Anterior and posterior longitudinal ligaments run along the vertebral body front and back, respectively. The posterior longitudinal ligament can become calcified in conditions such as diffuse idiopathic skeletal hyperostosis. In patients with either acquired or congenital stenosis of the spinal column, this calcified ligament
may compress the anterior spinal cord, especially with neck flexion which causes a 3-mm reduction in spinal canal diameter.
may compress the anterior spinal cord, especially with neck flexion which causes a 3-mm reduction in spinal canal diameter.
The posterior arch of each vertebra is formed by pedicles, lateral bodies, and laminae. The lateral body is formed on each side where the pedicle meets the lamina. There are five articulations between each of the typical vertebra: the intervertebral disk, along with uncovertebral joints (joints of Luchska), and facet (zygapophyseal) joints along each side of the vertebra. The uncinate process is a vertical projection from the posterolateral vertebral body that contacts the adjoining vertebral body to form the uncovertebral joint. The uncovertebral joint is not a true synovial joint but it is a frequent site of osteophytes. Two articular projections arise from each lateral body—a superior articular projection that
faces posteriorly and an inferior articular projection that faces anteriorly. Each projection forms a true synovial joint with its neighboring vertebra, and notches anterior to these projections coapt with complementary notches on adjacent vertebrae to form the intervertebral foramina. The facet joints formed by the articulation of these projections with neighboring vertebra are subject to degeneration or can be affected by inflammatory arthritis. Pain arising from arthritis in these joints typically is exacerbated by extension of the neck. For patients with focal posterior neck pain, injection of local anesthetic into the facet joint is sometimes used to confirm the joint as the generator of pain symptoms. Osteophytes arising from uncovertebral joints can cause anterior narrowing of the intervertebral foramina and osteophytes arising from the facet joints can cause posterior narrowing of the intervertebral foramina, which in either case can contribute to cervical spinal nerve compression causing radicular symptoms. The ligamentum flavum joins adjacent laminae; thickening of this ligament by degenerative processes can contribute to spinal stenosis and to spinal cord injuries in patients with spondylosis who suffer a hyperextension injury of the neck.
faces posteriorly and an inferior articular projection that faces anteriorly. Each projection forms a true synovial joint with its neighboring vertebra, and notches anterior to these projections coapt with complementary notches on adjacent vertebrae to form the intervertebral foramina. The facet joints formed by the articulation of these projections with neighboring vertebra are subject to degeneration or can be affected by inflammatory arthritis. Pain arising from arthritis in these joints typically is exacerbated by extension of the neck. For patients with focal posterior neck pain, injection of local anesthetic into the facet joint is sometimes used to confirm the joint as the generator of pain symptoms. Osteophytes arising from uncovertebral joints can cause anterior narrowing of the intervertebral foramina and osteophytes arising from the facet joints can cause posterior narrowing of the intervertebral foramina, which in either case can contribute to cervical spinal nerve compression causing radicular symptoms. The ligamentum flavum joins adjacent laminae; thickening of this ligament by degenerative processes can contribute to spinal stenosis and to spinal cord injuries in patients with spondylosis who suffer a hyperextension injury of the neck.
A transverse process off the side of the arch in the area of each lateral body and a midline posterior spinous process serve as anchor levers for musculature and ligaments. An intraspinous ligament joins adjacent spinous processes and helps prevent hyperflexion of the neck. The transverse process from C1 to C6 also has a transverse foramen where the vertebral artery courses until it enters the skull; in some patients extreme extension of the neck has been shown to lead to occlusion of the vertebral artery.
There are eight cervical spinal nerves with each cervical nerve root exiting through the intervertebral foramina above its corresponding vertebra except C8 which exits between C7 and T1. Each cervical spinal nerve is formed from an anterior root arising from motor neurons in the ventral horn of the spinal cord and a posterior root that carries afferent sensory fibers from the dorsal root ganglion. After exiting through the intervertebral foramina, the spinal nerves split into anterior and posterior rami. The anterior rami form the brachial plexus and provide motor innervation to the prevertebral and paravertebral muscles, whereas the posterior rami provide motor and sensory function of the posterior neck muscles, bones, and skin. Temporary and permanent blocks of the medial branch of the posterior rami can be used to diagnose and treat pain arising from posterior neck structures.
Since the major structures of the posterior neck are the spinal column and its contents and the supporting musculature, it can be helpful to elicit more detailed history about prior spinal column conditions such as lumbar degenerative disk disease, degenerative joint disease, radiculopathy, or nonspecific low back pain. It can also be helpful to inquire about ergonomic positions of the neck during work or sleep and the effect of positional or postural changes on symptoms. For patients with onset of neck pain after trauma, it is important to obtain a detailed history of the event to help estimate the amount, direction, and location of major forces acting on the neck and any protective or restraint systems such as seat belts or head rests in motor vehicles that may have mitigated the impact of the forces; this detailed data can help determine the likelihood of serious musculoskeletal or neurologic injuries. In patients with potential major trauma to the head or the neck, the neck should be immobilized until the possibility of underlying cervical fracture or spinal instability is ruled out.
Despite a detailed history, it can be difficult to localize neck pain to a specific anatomic source. Neck pain may be referred from multiple organs or areas including the heart, brachial plexus, jaw or esophagus, upper thorax, or the shoulder girdle or upper arm. Even for pain originating from somatic nerves, patients usually present with nonfocal pain making it difficult to pinpoint the inciting anatomic pathology, and degenerative changes on imaging studies have very poor correlation with the presence or severity of patient symptoms. Therefore, diagnostic specificity in the evaluation of neck pain relies on recognition
of patterns of symptoms, signs, and test results, while excluding emergent or other serious underlying conditions. In particular, patients should be asked about constitutional symptoms and risk factors for infections, history of or symptoms of malignancy, prior trauma, and symptoms suggestive of myelopathy such as clumsiness of the hands, weakness of the arms, bowel or bladder dysfunction, lower extremity weakness or numbness, or gait problems. Pain from tumor or infections is typically constant and progressive and unrelieved by rest or change in position. When morning stiffness is a prominent symptom, a rheumatologic condition such as rheumatoid arthritis, ankylosing spondylitis, or polymyalgia rheumatic should be considered.
of patterns of symptoms, signs, and test results, while excluding emergent or other serious underlying conditions. In particular, patients should be asked about constitutional symptoms and risk factors for infections, history of or symptoms of malignancy, prior trauma, and symptoms suggestive of myelopathy such as clumsiness of the hands, weakness of the arms, bowel or bladder dysfunction, lower extremity weakness or numbness, or gait problems. Pain from tumor or infections is typically constant and progressive and unrelieved by rest or change in position. When morning stiffness is a prominent symptom, a rheumatologic condition such as rheumatoid arthritis, ankylosing spondylitis, or polymyalgia rheumatic should be considered.
The history should include the elements of all basic pain histories, plus details about any preceding trauma, a history or risk factors for infection or cancer, and any constitutional or neurologic symptoms.
The physical examination should screen for neurologic abnormalities of the upper and lower extremities; specialized maneuvers may add additional sensitivity and specificity to the examination.
The need for and the type of diagnostic testing are determined by the working differential diagnosis after a careful history and physical examination.
Patients with axial neck pain without neurologic symptoms or signs and who are not suspected of having an emergent or serious underlying condition do not require initial imaging.
An understanding of cervical spinal anatomy is required to allow interpretation of imaging findings and reports.
Physical Examination
The physical examination of a patient with neck pain should start with general elements such as review of vital signs and observation of patient posture, movement, and gait. Presence of fever should raise suspicion of infection—particularly in IV drug abusers, patients with vascular access devices, or immunocompromised hosts. Abnormal carrying positions of the neck may be due to either a primary underlying musculoskeletal abnormality or a reflex spasm of the posterior neck muscles. In either case, spontaneous movement of the head is typically reduced. It is important to observe for a spastic gait that may originate from cervical spinal cord dysfunction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree