Navigation in Total Knee Arthroplasty
Alfred J. Tria Jr.
INDICATIONS
Navigation is a technology that assists the surgeon in checking the position and alignment of the total knee arthroplasty (TKA) to help decrease the number of outliers and, hopefully, extend the longevity of the implant. There is good scientific support for the use of the technology; however, there are reports in the literature that refute its efficacy and indicate that it increases the operative time for the procedure without additional accuracy for the experienced surgeon. Line-of-sight navigation remains the gold standard for the technology. Electromagnetic navigation has been introduced, and it does eliminate the problems of the line of site in the operating room; however, iron-containing instruments tend to interfere with the generated magnetic field and lead to associated inaccuracies.
CONTRAINDICATIONS
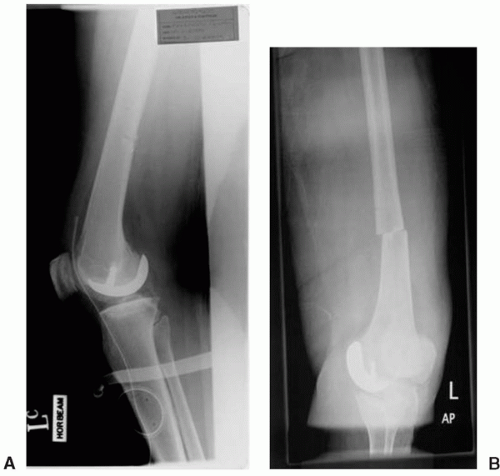
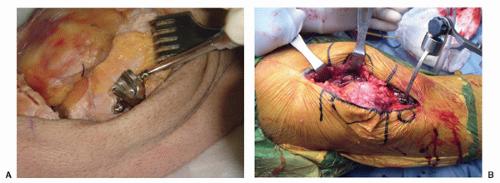
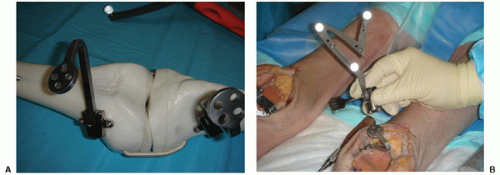
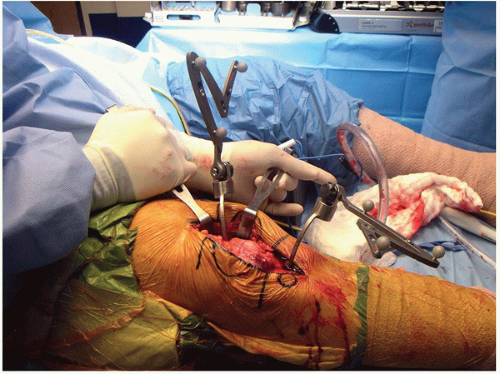
Most navigation techniques use percutaneous pins that are placed away from the operative site (Fig. 8-1). The pins can lead to fractures and can introduce infection into the area (Fig. 8-2). If the bone is particularly osteoporotic, such as in a severe rheumatoid patient, it may be difficult to stabilize the array with the pins. As the technology has improved, the pin diameter has been decreased, and most of the frames use two pins for greater stability. In an attempt to address the pin sites, some of the arrays are set within the operative incision, and there are now plates that can be attached to the metaphysis of the medial femur and tibia with small- diameter screws (Fig. 8-3). The plates form a base for the attachment of the arrays, and the arrays can be removed from the operative site when the navigation is not being used (Fig. 8-4). Navigation adds time to the operative procedure; and, if the anesthetic time is critical for a given patient, it may not be advisable to include it in the operative procedure.
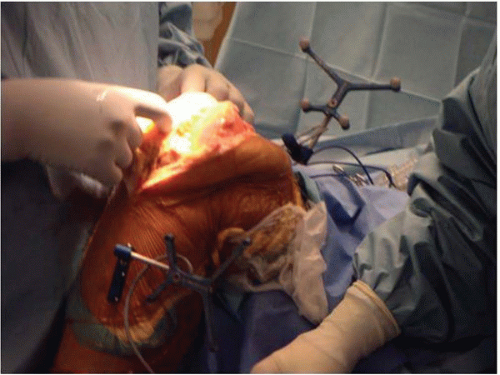 FIGURE 8-1 The percutaneous pins are placed outside the incision, and the arrays are attached to them. |
PREOPERATIVE PREPARATION
The preparation for the navigated knee arthroplasty should include the setup of the computer in the operating room so that this does not interfere with the usual procedure (Fig. 8-5). One or more of the instruments for landmarking will need to be calibrated with the computer and this step should also be completed before starting (Fig. 8-6). If percutaneous pins are going to be used, the area of preparation and draping should be extended both superiorly and inferiorly to include these areas in the sterile field. It saves time and effort if all of the instruments are prepared for the insertion of the pins or plates before beginning (Fig. 8-7).
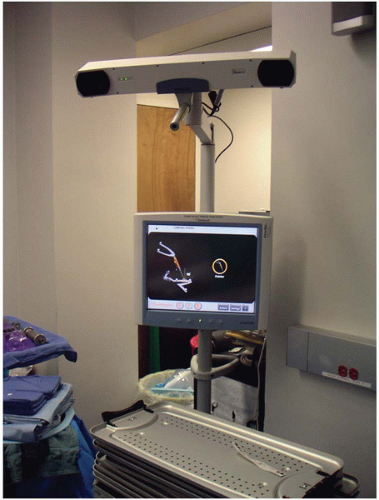 FIGURE 8-5 The navigation screen is positioned at the foot of the table with the camera aimed at the operative arrays. |
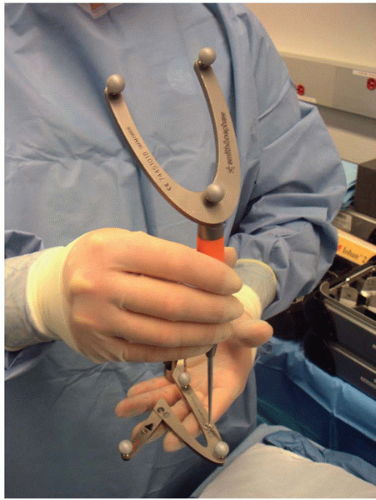 FIGURE 8-6 The calibration of the pointer for landmarking is completed before the start of the operation. In this case, there is a site on the array for the pointer for the calibration. |
 FIGURE 8-7 The navigation instruments are set up completely before the operation begins to decrease the time needed for the procedure. |
TECHNIQUE
Before the patient is brought into the operating room, it is best to have the computer screen and associated camera set at a convenient location in the room that will allow good access to the camera with as little repositioning as possible. The best location is typically at the foot of the operating room table or opposite the side of the table where the surgeon stands.
After the anesthetic has been stabilized, the lower leg will require preparation for proper sterility of the field, which must include the area for placement of the pins for the arrays. Dual-pin configurations are best applied outside the operative incision but not too far beyond the metaphyseal area to avoid pin-site fractures. Single-pin arrays usually require larger-diameter pins to ensure stability. This type of configuration can be placed more readily into the operative field but can interfere with the standard instruments used for the surgical procedure. The author favors using base plates for the arrays. These devices are placed within the operative incision, and the standard incision can be used for all cases (Fig. 8-3).
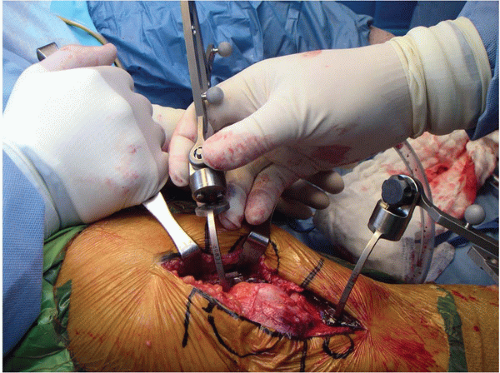
After the arthrotomy is completed, the medial femoral and tibial metaphyses are cleared as part of the standard approach. The femoral array is completely constructed including the base plate, the curved arm, and the array itself (Fig. 8-8). The plate is placed along the medial femoral metaphysis as a trial to see if it will lie in an area that will not interfere with the knee’s capsule and the standard instrumentation. After confirming the freedom of the surrounding soft tissues, the plate is fixed to the cortical bone surface with two locking screws. The tibial plate is attached next in a similar fashion. After both plates are in place, the full array is attached to both of the plates with the knee in full extension (Fig. 8-9). The arrays can still be rotated on the magnetic base and can also be moved from flexion to extension. Once the position is set in full extension, the knee should be taken through the full range of motion to check line of sight with the camera through the entire range of motion of the knee. It is much easier to check the visibility at this time before proceeding with the landmarking.
After the array positions are confirmed, the anatomic landmarks of the knee must be identified. The leg is usually moved through a series of positions with the hip and knee slightly flexed to identify the center of the femoral head in the hip joint (Fig. 8-10). Each system has a routine number of points that must be identified on the femur and the tibia. It is critical to identify these points as accurately as possible. This step requires time and patience; however, if the points are well identified, the navigation will be much more accurate and reliable.
Before proceeding with the surgery, the alignment of the knee should be established with reference to the mechanical axis. A routine mechanical axis x-ray is performed on each patient before the
surgery, which is used to confirm the accuracy of the intraoperative navigation. In most cases, the two numbers for the mechanical axis should be within 1 to 2 degrees of each other. If there is a great discrepancy, the land-marking is fully repeated, and the x-ray is measured again and checked for abnormal rotation. Once these parameters have been fully confirmed, the surgery can commence.
surgery, which is used to confirm the accuracy of the intraoperative navigation. In most cases, the two numbers for the mechanical axis should be within 1 to 2 degrees of each other. If there is a great discrepancy, the land-marking is fully repeated, and the x-ray is measured again and checked for abnormal rotation. Once these parameters have been fully confirmed, the surgery can commence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree