reaching a critical mass must be present, and the species and the number of bacteria present must overwhelm host defenses in the particular anatomic site in question. Although random chance may have a role in determining where and when bone and joint infection occurs, specific patterns of infection have been observed that can lead to no other conclusion than that specific factors influence where and in whom musculoskeletal infection occurs.
forming a sequestrum. Because the periosteum retains its blood supply, it remains viable and produces osteoid. The new bone forming around the necrotic sequestrum is known as involucrum. If the metaphysis is intra-articular at the site where infection breaches the metaphyseal cortex, septic arthritis results. Infection generally does not spread down the medullary cavity because the well-developed reticuloendothelial system of the diaphysis is able to prevent its expansion in this direction.
cause the treating physician to maintain greater vigilance for subacute osteomyelitis.
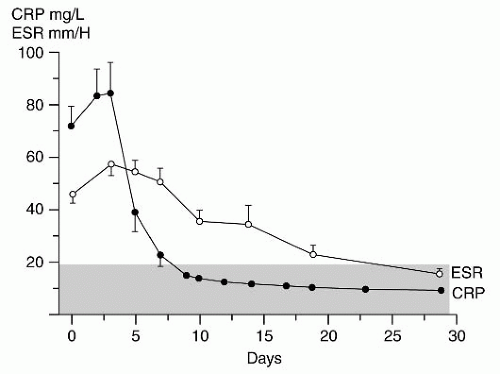
concentration of fibrinogen. The ESR result can be affected by the size, shape, and number of erythrocytes present, as well as by other proteins in plasma. Therefore, the ESR is less reliable in the neonate, in the presence of anemia, in patients with sickle cell disease, or when the patient is taking steroids (64, 65).
promotes binding of a polymerase that replicates the target segment in a series of temperature-dependent cycles. The amplification products are then identified by gel electrophoresis. PCR has produced some promising results in the diagnosis of periprosthetic infections and septic arthritis, but a high falsepositive rate has been reported (75). Recently, success has been reported performing molecular diagnosis of musculoskeletal K. kingae infection by specific, real-time PCR assay (76, 77 and 78). These authors report the K. kingae PCR assays to be reliable and especially helpful in identifying infection caused by this fastidious organism.
temperature, resting pulse rate, ESR, length of hospital stay, and rate of surgical intervention compared to patients with hot scan osteomyelitis.
or deposition of calcium phosphate. Tumor, trauma, and bone resorption due to disuse may cause increased uptake. The scans may be negative in the first 24 hours of infection before stimulation of bone turnover, and there may be a 4% to 20% false-negative rate with technetium scanning (64). In neonatal infection, the reported sensitivity for technetium scanning has ranged from 30% to 86%, and standard radiography may be more helpful (6, 7, 95). Overall specificity and sensitivity are improved when the scan is interpreted with knowledge of the clinical findings and initial laboratory studies, compared to when the interpretation was a blind reading of the scan (96).
with suspected osteomyelitis or septic arthritis and found that iatrogenic soft tissue and bone edema related to recent surgery in children with suspected osteomyelitis or septic arthritis has minimal effect on diagnostic accuracy of MRI (108). Spiegel et al. (109) at Children’s Hospital of Philadelphia evaluated the usefulness of MRI as a routine follow-up test used to assess surgical treatment of musculoskeletal infection and noted that if patients’ clinical course was unremarkable, MRI did not add clinically significant additional information. From these two studies, we can conclude that if patients demonstrate clinical improvement with treatment, then routine follow-up MRI is not necessary, but if the treatment course is complicated by clinical evidence of persistent or recurrent infection, then MRI can provide helpful, reliable information that is not degraded by previous surgery.
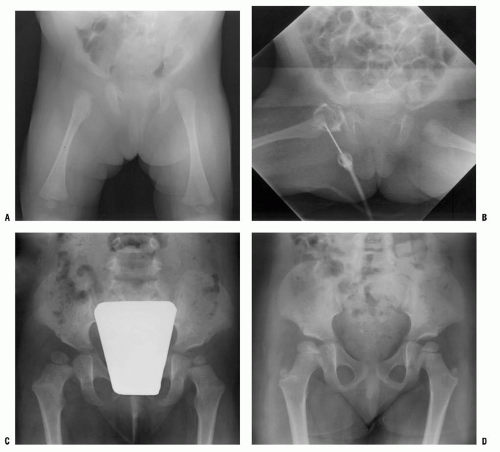
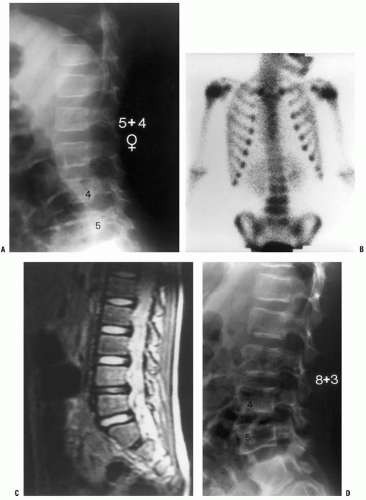
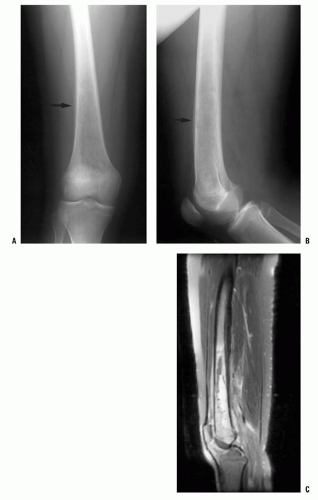
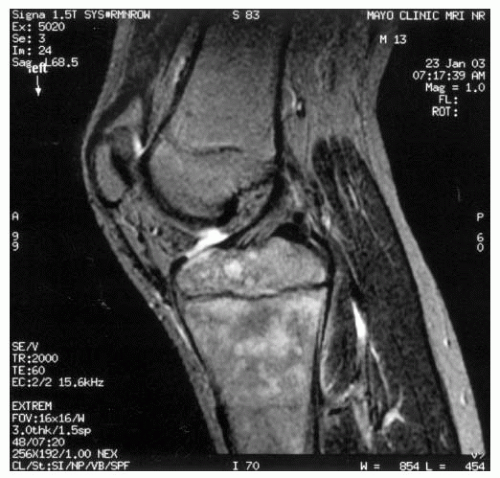
of the process, then technetium bone scintigraphy is an appropriate next imaging study (Fig. 12-4). If additional imaging is needed to establish a diagnosis or characterize a pathologic process once the process has been localized, then MRI is the imaging study of choice to provide maximal information about the bone and soft-tissue pathology. For straightforward musculoskeletal infection in the appendicular skeleton, MRI is often not necessary; but for patients whose history, examination, laboratory evaluation, and plain film radiographs are not concordant, or for patients with suspected infection of the pelvis or axial skeleton, MRI is a very helpful imaging study.
TABLE 12-1 Synovial Fluid Analysis | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
had a cell count of >50,000 per mL. Brucella melitensis was recovered from the synovial fluid culture in all patients (119).
thought to be a postinfectious arthritis. Both may present with a history of a few to several days of hip pain and with limp progressing to the inability to walk. The physical signs are similar in both, with limited and painful internal rotation, abduction, and extension. A longer history of symptoms, with cyclic improvement and worsening, suggests toxic synovitis. The pain is usually worse and the motion more restricted in septic arthritis.
TABLE 12-2 Empiric Antibiotic Treatment Recommendations for Musculoskeletal Infection | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
appropriate intravenous antibiotic. Similar to the antibiotic treatment of septic arthritis, the administration route and the duration of treatment of AHO are controversial and depend upon the clinical situation of each patient. At one time, nearly all children with AHO were routinely treated with 6 weeks of intravenous antibiotics as a hospital inpatient. Over the last two decades, several trends have developed: (a) treatment has moved from inpatient to an outpatient setting and (b) treatment has shifted from entirely parenteral to a parenteral then oral antibiotic regimen. Intravenous therapy is initiated in the hospital setting, but once therapeutic response to treatment is confirmed, conversion to oral antibiotic treatment is made and continued on an outpatient basis.
TABLE 12-3 Antibiotics Commonly Used in the Treatment of Bone and Joint Sepsis | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
necrotic sequestrum. A valuable general treatment principle is to aggressively debride the necrotic sequestrum but to leave in place the viable involucrum.
1. Recurrent/persistent infection despite a course of reasonable and appropriate treatment
2. Extensive chronic infection that cannot be completely débrided surgically
3. Extensive osseous defects and dead space to be treated by delayed bone grafting (Fig. 12-7)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree