Multiple Ligament Knee Reconstruction
Peter S. Cha MD
Jeffrey A. Rihn MD
Christopher D. Harner MD
History of the Technique
Traumatic knee dislocation has long been recognized as a serious injury. Injury to the cruciate and collateral ligaments, menisci, articular cartilage, and neurovascular structures complicate the evaluation and management of traumatic knee dislocation. The potentially disastrous consequences of mismanagement are known well, particularly in knee dislocation that involves limb-threatening vascular injury. The multiple-ligament-injured knee is a difficult problem that requires thorough evaluation and treatment by an experienced knee surgeon.
Treatment of multiligament knee injury has evolved over the past century. In the early to mid-1900s, traumatic knee dislocation was treated with cast immobilization. The majority of patients treated conservatively experienced a poor outcome. Surgical repair became a viable treatment option in the mid-1900s. Primary repair of the injured ligaments in the dislocated knee was reported by O’Donoghue1 in 1955 with good results; the best results were obtained in those patients treated within 2 weeks of their initial injury. Several reports in the literature from the 1960s to the 1980s supported primary ligamentous repair as the recommended form of treatment of knee dislocation and multiple ligament injury.2,3,4,5,6 Because of the limited potential for primary healing of the cruciate ligaments, cruciate ligament reconstruction has been the preferred method of treatment since the 1980s. Except in cases of osseous avulsion, primary repair of the cruciate ligaments has fallen out of favor. Most experienced knee surgeons currently approach the surgical management of acute knee dislocations with a goal of anatomic repair and reconstruction of all associated ligamentous and meniscal injuries.7,8,9,10 This involves combined, arthroscopically assisted anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) reconstruction, meniscal repair or resection, and either primary repair or reconstruction of posterolateral corner (PLC) injuries, depending on the timing of the treatment and condition of the soft tissues. This chapter will review, in detail, our preferred method for surgical management of the multiple-ligament-injured knee with emphasis on the technical considerations.
Indications and Contraindications
Knee dislocation is a severe injury with potentially devastating consequences. Whereas surgical treatment of the majority of knee dislocations can be delayed 2 to 3 weeks from the time of initial injury, certain cases require immediate surgical intervention. Evaluation and initial management must be performed expeditiously to prevent limb-threatening complications and to identify indications for emergent intervention. Initial assessment includes a brief history, a directed physical examination, thorough neurovascular evaluation, and plain radiographs of the injured knee. Knee dislocation can be either a high-energy (e.g., motor vehicle accident), or low-energy (e.g., twisting injury during sports activity) injury. Up to 50% of knee dislocations spontaneously reduce prior to evaluation. Therefore, if the exam reveals substantial laxity of two or more of the major ligaments of the knee, then a presumptive diagnosis of knee dislocation should be made. In cases of gross knee dislocation, the knee should be reduced immediately through gentle traction-countertraction under conscious sedation and the limb should be stabilized in a long leg splint. A postreduction neurovascular exam should be performed, and reduction should be confirmed with anteroposterior and lateral radiographs.
Popliteal artery injury and peroneal nerve injury are reported to occur in up to 45% and 40% of knee dislocations,
respectively.5,11 The presence of these associated injuries will affect the surgical treatment plan and must be detected promptly. Some authors recommend the use of selective popliteal artery angiography in the setting of acute knee dislocation, performing angiography only in the presence of asymmetric distal pulses or an abnormal ankle brachial index (ABI).12,13,14,15 Unfortunately, normal pulses, a warm foot, and brisk capillary refill can exist in the face of an intimal tear of the popliteal artery, which may not manifest itself for several days after the initial injury.11,16 We currently perform popliteal artery angiography or CT angiography on all cases of suspected knee dislocation to rule out such an injury. The routine use of angiography in this setting is justified by the relatively low morbidity of the test, the high incidence of popliteal artery injury, and the potentially devastating consequences of any delay in diagnosis.
respectively.5,11 The presence of these associated injuries will affect the surgical treatment plan and must be detected promptly. Some authors recommend the use of selective popliteal artery angiography in the setting of acute knee dislocation, performing angiography only in the presence of asymmetric distal pulses or an abnormal ankle brachial index (ABI).12,13,14,15 Unfortunately, normal pulses, a warm foot, and brisk capillary refill can exist in the face of an intimal tear of the popliteal artery, which may not manifest itself for several days after the initial injury.11,16 We currently perform popliteal artery angiography or CT angiography on all cases of suspected knee dislocation to rule out such an injury. The routine use of angiography in this setting is justified by the relatively low morbidity of the test, the high incidence of popliteal artery injury, and the potentially devastating consequences of any delay in diagnosis.
Emergent surgery is indicated in open or irreducible dislocations of the knee and in those cases of knee dislocation with associated vascular injury or compartment syndrome. In cases of open knee dislocation, the standard principles of wound management prevail. These include serial irrigation and debridement, intravenous antibiotics, and adequate soft tissue coverage. Ligament reconstruction should not be performed acutely in open knee dislocations. In some cases, soft tissue coverage problems may force ligament reconstruction to be delayed for several months. Irreducible dislocations are not common. When encountered, they require prompt surgical reduction to avoid prolonged traction on the neurovascular structures. Although ligament reconstruction can be done at the time of the reduction, we prefer to delay the definitive reconstruction to allow for more complete knee imaging, planning, and resource mobilization. Popliteal artery injuries require emergent intervention by a vascular surgeon. An orthopedic surgeon’s input as to the location of incisions is often helpful for future reconstructive efforts. Saphenous vein grafting is often required, as are fasciotomies, following revascularization. Compartment syndrome is an orthopedic emergency. The presence of a knee dislocation does not change its management. Prompt diagnosis and fasciotomies are necessary for a successful outcome. During emergent surgery on a dislocated knee, it is acceptable to perform simple primary repair of injured soft tissue structures as they are encountered during the surgical exposure. Excessive foreign material, including suture, is avoided in open injuries. Additional incisions are avoided in the emergent setting. Definitive ligament reconstruction should be delayed several days to allow for recovery of the soft tissues and decreased swelling. In cases of vascular injury, additional time is required to ensure that the vascular repair is adequate and to allow limb swelling to subside.
The majority of multiple-ligament-injured knees are currently treated surgically, with the goal of anatomic repair and reconstruction of all associated ligamentous and meniscal injuries. This approach has been reported to provide adequate knee stability and motion and allow the patient to return to normal daily activities.7,8,9,10,17 Closed reduction and cast immobilization of knee dislocation currently has few relative indications, including elderly or sedentary patients and patients who have debilitating medical or posttraumatic co-morbidities. Patients who initially undergo a trial of conservative management often require surgery at a later date due to problems with knee function, including loss of motion and persistent instability. Prior to surgical treatment, additional evaluation is necessary to characterize the pattern of injury (i.e., which structures are injured) and determine an appropriate surgical plan. In addition to disruption of the cruciate ligaments, the majority of knee dislocations involve injury to the collateral ligaments, the posterolateral structures of the knee, or the menisci. The key components of this evaluation are physical examination, magnetic resonance imaging (MRI), and arthroscopy. A thorough ligamentous exam is performed after survival of the limb is ensured and the patient is stabilized. Because guarding can obscure the examination in an awake patient, examination under anesthesia should be performed prior to operative treatment. MRI is used to characterize soft tissue and occult osseous injuries only after the patient has been acutely stabilized. MRI results are helpful in determining which structures are reparable and which must be reconstructed. Arthroscopic examination at the start of the definitive operative procedure is necessary to confirm the preoperative diagnosis and detect additional injuries not detected during the preoperative workup.
Surgical Techniques
Anesthesia
The choice of anesthesia is made in conjunction with the surgeon, the anesthesiologist, and the patient. The factors influencing the preferred anesthesia technique include the age of the patient, the patient’s comorbid medical problems, and the previous anesthesia history of the patient. The anesthesia team typically chooses between a general anesthesia or an epidural anesthetic with concomitant intravenous (IV) sedation. If the anesthesiologist is at all concerned about airway management, then general anesthesia is used. At our center, preoperative femoral or sciatic nerve blocks are routinely performed. The nerve blocks have not only been useful during the surgical procedure, but they offer 9 to 12 hours of postoperative pain relief. A Foley catheter is placed to help monitor the fluid status during the case. We recommend that a vascular surgeon be on call during the procedure as unexpected injuries to the vessels may occur.
Surface Anatomy and Skin Incision
The patient is seen in the preoperative holding area and the correct extremity is identified by both the surgeon and the patient. The correctly selected extremity should correlate with the written consent. Using an indelible marker, the surgeon then places his or her initials on the correct extremity
with the word yes; this should be strategically placed so that the signature is within the operative field.
with the word yes; this should be strategically placed so that the signature is within the operative field.
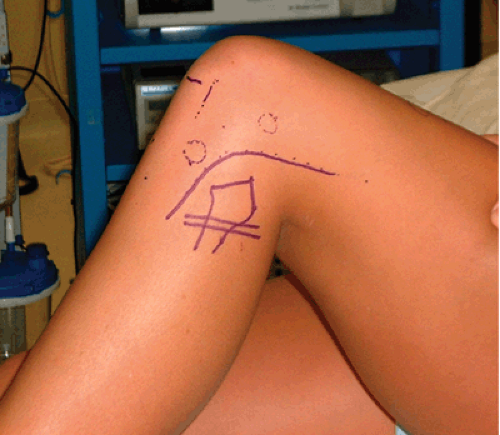
A marker is used to identify the surface anatomy and the incisions that will be utilized during the procedure (Fig. 49-1). The important osseous landmarks that include the patella, the tibial tubercle, Gerdy tubercle, and the fibular head are identified. The peroneal nerve is palpated and marked superficial to the fibular neck. The medial and lateral joint lines are identified. The potential skin incisions are then drawn. The anterolateral arthroscopy portal is placed adjacent to the lateral border of the patella above the joint line. The anteromedial arthroscopy portal is placed approximately 1 cm medial to the patellar tendon at the same level. A superolateral outflow portal is placed proximal to the superior border of the patella and posterior to the quadriceps tendon. The posteromedial portal is established if needed from an inside-out technique and thus is not initially marked. A longitudinal 3-cm incision that originates approximately 2 cm distal to the joint line and 2 cm medial to the tibial tubercle is drawn on the anteromedial proximal tibia for the ACL and PCL tibial tunnels. Also, a 2-cm incision is placed just medial to the medial trochlea articular surface and along the subvastus interval for the PCL femoral tunnel. If there is a medial ligament injury, then the distal incision for the tibial tunnels is traced proximally to the medial epicondyle and extended to the level of the vastus medialis in a curvilinear fashion. The incision for the lateral and posterolateral injuries is a curvilinear 12-cm incision that is drawn midway between the Gerdy tubercle and the fibular head and traced proximally just inferior to the lateral epicondyle while the knee is flexed 90 degrees.18 The proximal extent of this incision parallels the plane between the biceps femoris tendon and the iliotibial band (Fig. 49-2). We prefer the medial and lateral incisions as previously described and avoid the used of a midline incision as this could potentially be complicated by skin breakdown over the patella and often can limit access to the collateral ligaments. Finally, the dorsalis pedis pulse is palpated and marked.
Specifics of the Procedure
The patient is evaluated in the preoperative area for a detailed neurovascular examination with documentation of the status of the popliteal, dorsalis pedis, and posterior tibial pulses and the function of the tibial and peroneal nerves. After successful induction of anesthesia in the operating room suite, a thorough examination under anesthesia is performed and correlated with the preoperative impression from the office notes. It is of utmost importance to examine the opposite extremity and use it as a reference. The examination begins by taking the knee through a range of motion and noting any deficits. The anterior drawer, Lachman, and pivot shift tests reveal any deficits to the ACL. The PCL is examined by appreciating any posterior sag with associated step-off and by testing a posterior drawer at 90 degrees of flexion. The lateral collateral ligament (LCL) is palpated in the figure-four position and tested with a varus stress at 0 degrees and 30 degrees. The PLC is tested at 30 degrees and by holding the proximal tibia and externally rotating the leg; also, the PLC is tested by applying an external rotation force on the proximal tibia and fibula while the knee is flexed 90 degrees to feel for lateral dropout. The medial collateral ligament (MCL) is examined with a valgus stress at 0 degrees and 30 degrees. Once a thorough exam is completed, the extent of the ligamentous injuries is better understood, which helps guide the surgical procedure.
The two most common combined injury patterns with knee dislocations include the ACL, PCL, and MCL and the ACL, PCL, LCL, and PLC. Less commonly, the PCL is intact or only partially torn and does not require a reconstruction.19,20 At our institution we are recognizing injury patterns with PCL injuries that preserve specific bundles of the PCL. Most commonly, we are observing that the anterolateral bundle is ruptured; however, the meniscofemoral ligament (MFL) and the posteromedial bundle may remain
intact. If we see this injury pattern, an attempt is made to preserve the intact portion of the PCL and MFL and to simply reconstruct the ruptured portion via a single bundle technique. Our approach is to reconstruct or repair all injured structures. The intrasubstance tears for the ACL, PCL, LCL, and PLC typically require reconstruction, while intrasubstance tears of the MCL and avulsed ligaments are usually repaired. Also, concomitant injuries to the articular cartilage and menisci are operatively addressed at the time of surgery.
intact. If we see this injury pattern, an attempt is made to preserve the intact portion of the PCL and MFL and to simply reconstruct the ruptured portion via a single bundle technique. Our approach is to reconstruct or repair all injured structures. The intrasubstance tears for the ACL, PCL, LCL, and PLC typically require reconstruction, while intrasubstance tears of the MCL and avulsed ligaments are usually repaired. Also, concomitant injuries to the articular cartilage and menisci are operatively addressed at the time of surgery.
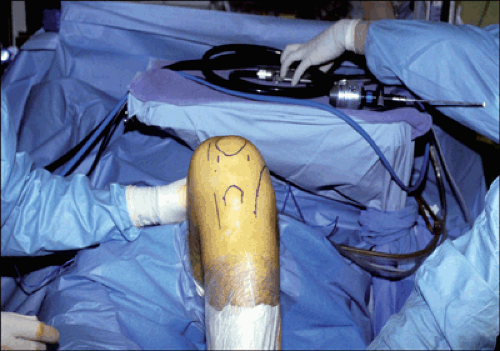
Patient Positioning
The supine patient is properly positioned on the operating room table. Our goal is to have a full free range of motion of the involved extremity during the procedure with the ability to have the knee statically flexed at 80 degrees to 90 degrees without any manual assistance. We accomplish this by placing a small gel pad bump under the ipsilateral hip with a post placed on the side of the bed just distal to the greater trochanter; a sterile bump of towels or drapes is wedged between the post and the thigh. The heel rests on a 10 lb sandbag that is taped to the bed during the initial positioning (Fig. 49-1). A well-padded tourniquet is placed on the proximal thigh; however, it is not inflated unless necessary and thus rarely used. Intravenous antibiotics are administered prior to the skin incision. The previously described skin incisions are drawn and the pulses are once again palpated and marked. The extremity is prepped with alcohol and Betadine solution and draped in a meticulous fashion. The skin incisions are injected with 0.25% Marcaine with 1:100,000 epinephrine. The mini C-arm fluoroscopy machine is in the operating suite and draped.
Repair versus Reconstruction
With knee dislocations, the decision to repair or reconstruct the injured structures depends on numerous factors. Concerning cruciate injuries, the majority of injuries are intrasubstance tears that are not amenable to surgical repair but are best treated with ligament reconstruction. However, we do recommend a primary repair of the ACL or PCL if a large bony fragment remains on their respective tibial insertions.21,22 The primary repair can be accomplished by passing large nonabsorbable sutures (no. 5) into the bony fragment and through bone tunnels in the tibia. Also, a primary repair of the PCL insertion may be advocated in the case of a “peel off” or a soft tissue avulsion of the PCL at its femoral insertion by a similar technique.23 Concerning the MCL, LCL, and PLC, it is our experience that a primary repair may have successful results if operatively addressed within 3 weeks of injury. If the injury is chronic, scar formation and soft tissue contracture usually limit the success of a primary ligamentous repair and a ligament reconstruction is often necessary. The MCL can be directly repaired with intrasubstance sutures or with suture anchors if avulsed off the bone. Repair of the posterolateral corner structures and the LCL can be accomplished with direct suture repair or by repair to bone via drill-holes versus suture anchors. If direct repair is not possible due to the quality of the tissue, then the involved structures should be augmented with hamstring tendons, biceps femoris, iliotibial band, or allograft; otherwise the involved structures should be reconstructed.24
Diagnostic Arthroscopy
The arthroscope is introduced into the anterolateral portal and the intra-articular findings are correlated with the preoperative MRI and exam under anesthesia. An arthroscopic approach is advocated to assist in the planning in the potential skin incisions (medial or lateral) needed for the procedure based on the pattern of injury. Gravity inflow is used with a superolateral outflow. Care must be taken to avoid a compartment syndrome, and the posterior leg and calf region must be palpated intermittently during the procedure. Factors that influence a potential compartment syndrome include an acute reconstruction (less than 2 weeks from the time of injury) in which the capsular healing was insufficient to maintain joint distension or if the capsule has been breeched iatrogenically during the procedure. If extravasation is noted and a potential compartment syndrome is suspected, then the arthroscopic technique is abandoned and the remainder of the procedure is performed via an open technique. However, the arthroscope can still be a valuable tool when used in a dry field by improving the visualization and magnification during the open procedure.
All compartments are assessed within the knee. The MCL is visualized in the medial compartment and the meniscal attachment to the deep MCL is assessed to determine if a femoral, midsubstance, or tibial-sided injury has occurred. The popliteus tendon is visualized and probed in the lateral compartment to determine where the injury occurred or if there is any functional compromise. The PCL is examined at both its femoral and tibial insertions. The PCL most often undergoes an interstitial tear of the ligament. A posteromedial portal is needed to completely visualize the tibial insertion of the ligament. This is established under direct visualization by placing the 70-degree arthroscope into the anterolateral portal and through the intercondylar notch adjacent to the posterior aspect of the medial femoral condyle. The spinal needle and trocar is delivered just anterior to the saphenous nerve and vein.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree