CHAPTER 28 Multiple-Ligament Knee Injuries and Management of Knee Dislocations
The combined anterior cruciate ligament–posterior cruciate ligament (ACL-PCL) injured (dislocated) knee is a severe injury that can result from high- or low-energy trauma. Both cruciates are torn, plus one or both collateral ligament complexes. The frequency of popliteal artery injuries occurs with the same frequency in bicruciate knee ligament injuries and frank tibiofemoral dislocations. Nerve injuries, associated fractures, other structural injuries, functional instability, and post-traumatic arthrosis may all occur with this injury complex.1,2
ANATOMY
Knee dislocations can be classified by the direction of tibial displacement, anatomic classification, open or closed injury status, and the energy level associated with the knee dislocation.3 Hyperextension of the tibiofemoral joint leads to anterior tibiofemoral dislocation. This mechanism may result in popliteal artery stretch, leading to intimal arterial damage, delayed thrombus formation, and ultimate arterial occlusion. The dashboard knee mechanism of injury leads to abrupt posterior tibial dislocation with the knee at 90 degrees of flexion, and may result in arterial transection. Varus force inducing tibiofemoral dislocation may result in peroneal nerve injury.1–3
PATIENT EVALUATION
History and Physical Examination
Initial evaluation of the acute bicruciate ligament injured knee includes evaluation of the deformity, location of abrasions or contusions, neurovascular status of the extremity, and presence or absence of a dimple sign. The presence of normal pulses, normal Doppler, and normal capillary refill in the presence of a reduced bicruciate (dislocated) knee does not guarantee the absence of vascular injury. Serial physical examinations, ankle brachial indices, and arteriography all must be used as necessary to document intact arterial circulation to the injured lower extremity.4–19
TREATMENT
Indications and Contraindications
The current consensus indicates that surgical treatment yields better results than nonsurgical treatment of the multiple-ligament injured knee.20–25 Technical advancements in the procurement, processing, and use of allograft tissue, arthroscopic surgical instruments, graft fixation methods, and improved surgical techniques, and an improved understanding of the ligament structures and the biomechanics of the knee, have led to more predictable and successful results in the treatment of these complex knee injuries. Various studies have published excellent results with return to preinjury level of function documented with physical examination, arthrometer measurements, knee ligament rating scales, and stress radiography.2,26–33
Arthroscopic Technique
Surgical Timing
Surgical timing in the acute bicruciate multiple-ligament injured knee is dependent on the vascular status of the involved extremity, collateral ligament injury severity, degree of instability, and postreduction stability. Delayed or staged reconstruction of 2 to 3 weeks postinjury has demonstrated a lower incidence of arthrofibrosis.30,31
Surgical timing in acute ACL-PCL lateral side injuries is dependent on the lateral side classification.34 We have described three types of posterolateral instability, A, B, and C.34 Posterolateral instability (PLI) type A has increased external rotation only, corresponding to injury to the popliteofibular ligament and popliteus tendon. PLI type B presents with increased external rotation and mild varus of approximately 5 to 10 mm, with increased lateral joint line opening to varus stress at 30 degrees of knee flexion. This occurs with damage to the popliteofibular ligament and popliteus tendon, and attenuation of the fibular collateral ligament. PLI type C presents with increased tibial external rotation and varus instability of 10 mm more than the normal knee tested at 30 degrees of knee flexion with varus stress. This occurs with injury to the popliteofibular ligament, popliteus tendon, fibular collateral ligament, and lateral capsular avulsion in addition to cruciate ligament disruption. The intact medial collateral ligament, tested with valgus stress at 30 degrees of knee flexion, is the stable hinge in the ACL-PCL- posterolateral corner (PLC)–injured knee.
Surgical timing in acute ACL-PCL medial side injuries is also dependent on the medial side classification. Some medial side injuries will heal with 4 to 6 weeks of brace treatment, provided that the tibiofemoral joint is reduced in all planes. Other medial side injuries require surgical intervention. Types A and B medial side injuries are repaired or reconstructed as a single-stage procedure with combined arthroscopic ACL-PCL reconstruction. Type C medial side injuries combined, with ACL-PCL tears are often treated with staged reconstruction. The medial posteromedial repair or reconstruction is performed within the first week after injury, followed by arthroscopic combined ACL-PCL reconstruction 3 to 6 weeks later.1,2,30,31,35,36
Surgical timing may be affected by factors beyond the surgeon’s control, and may cause the surgical treatment to be performed earlier or later than desired. These include injured extremity vascular status, open or closed injury, reduction stability, skin conditions, multiple system injuries, other orthopedic injuries, and meniscal and articular surface injuries.1,2
Patient Positioning
When there is a posterior cruciate ligament tear, the tear of the PCL is identified and the intact anterior cruciate ligament is confirmed. The residual stump of the posterior cruciate ligament is débrided with the synovial shaver and hand tools, as necessary. In the case of a combined ACL-PCL injury, the residual stumps of both the anterior and posterior cruciate ligaments are débrided. In patients with combined ACL-PCL injuries, the notchplasty for the ACL portion of the procedure is performed at this time.
Initial Incision
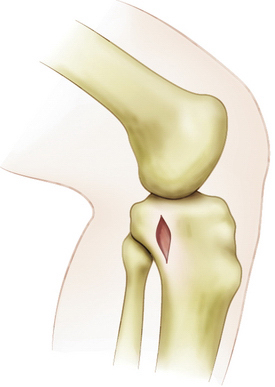
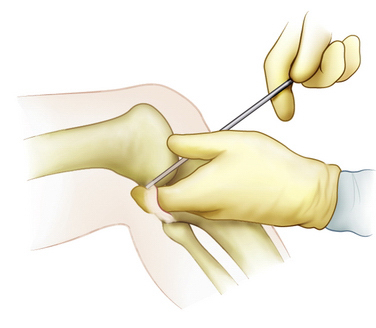
An extracapsular extra-articular posteromedial safety incision is made by creating an incision approximately 1.5 to 2 cm long, starting at the posteromedial border of the tibia approximately 1 inch below the level of the joint line and extending distally (Fig. 28-1). Dissection is carried down to the crural fascia, which is incised longitudinally. Care is taken to protect the neurovascular structures. An interval is developed between the medial head of the gastrocnemius muscle posterior and the capsule of the knee joint anterior. The surgeon’s gloved finger is able to position the neurovascular structures posterior to the finger and the capsule anterior to the finger (Fig. 28-2). In this way, the surgeon can monitor tools such as the over the top PCL instruments and the PCL-ACL drill guide as it is positioned in the posterior aspect of the knee. This also allows for accurate placement of the guide wire in medial lateral and proximal distal directions. The PCL and ACL reconstructions are performed with the knee in approximately 70 to 90 degrees of knee flexion.
Elevating the Capsule.
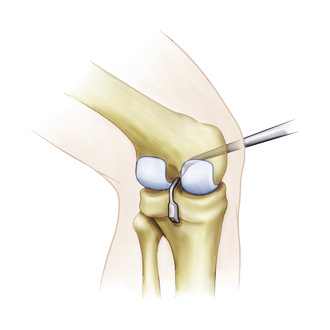
The curved over the top PCL instruments are used to lyse adhesions in the posterior aspect of the knee sequentially and elevate the capsule from the tibial ridge posteriorly. This will allow accurate placement of the drill guide and correct placement of the tibial tunnel (Fig. 28-3).
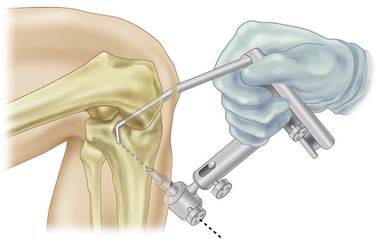
Positioning of the Guide
The arm of the PCL-ACL guide is inserted through the inferior medial patellar portal. The tip of the guide is positioned at the inferior lateral aspect of the PCL anatomic insertion site. This is below the tibial ridge posterior and in the lateral aspect of the PCL anatomic insertion site. The bullet portion of the guide contacts the anteromedial surface of the proximal tibia at a point midway between the posteromedial border of the tibia and the tibial crest anterior, approximately 1cm below the tibial tubercle (Fig. 28-4). This will provide an angle of graft orientation so that the graft will turn two very smooth 45-degree angles on the posterior aspect of the tibia and will not have an acute 90-degree angle turn, which may cause pressure necrosis of the graft. The tip of the guide, in the posterior aspect of the tibia, is confirmed with the surgeon’s finger through the extracapsular extra-articular posteromedial safety incision. Intraoperative anteroposterior (AP) and lateral x-rays may also be used. When the PCL-ACL guide is positioned in the desired area, a blunt spade-tipped guide wire is drilled from anterior to posterior. The arthroscope, in the posterior medial portal, visualizes the tip of the guide wire. The surgeon’s finger confirms the position of the guide wire through the posterior medial safety incision. This is a double safety check.