Authors and year |
Material |
Findings |
|---|
Betts, 1940 |
19 cases |
The first to make a histologic examination; found increased fibrous tissue elements |
Cottrell, 1940 |
— |
Found progressive thickening of the walls of the endoneural vessels and the perineurium with aging in normal nerves |
McElvenny, 1943 |
12 specimens, 11 patients |
Neurofibromas or angioneurofibromas; Renaut’s bodies |
Baker and Kuhn, 1944 |
14 specimens, 11 patients |
Resembled amputation neuroma: reactive hyperplasia |
King, 1946 |
5 cases |
“Sclerosing neuroma” |
Bickel and Dockerty, 1947 |
18 cases |
Interstitial edema and irregular demyelination |
Nissen, 1948 |
27 cases |
Local vascular degeneration: an ischemic lesion |
Winkler, Felner, and Kimmelstiel, 1948 |
20 cases |
Essentially a degenerative process |
Ringertz and Unander-Scharin, 1950 |
18 specimens, 21 controls |
Endoneural edema and demyelination are the characteristic features of Morton’s neuroma |
Scotti, 1957 |
17 cases |
“Endarteritis-fibrosis complex’ |
Viladot and Moragas, 1966 |
7 cases |
Similar degenerative changes; no sign of inflammation or thrombotic injury |
Meachin and Abberton, 1971 |
23 specimens, 19 patients, 23 controls |
Nonspecific degenerative reactive changes |
Reed and Bliss, 1973 |
118 cases |
“Regressive and productive intermetatarsal elastofibrositis;” elastin tissue proliferation in the fibroadipose tissue surrounding Morton’s neuroma |
May, 1976 |
31 specimens |
“Traumatic neuritis” with proliferation of connective tissue elements: neurofibroma |
Lassmann, 1976 |
105 patients |
Thickened perineurium, thickened walls of endoneural vessels, endoneural edema and sclerosis, axonal degeneration without wallerian degeneration |
Tate and Rusin, 1978 |
50 specimens |
Marked fibrosis and collagenous infiltration; demyelination; axonal degeneration |
Goldman, 1979, 1980 |
133 cases |
Demyelination diagnostic of intermetatarsal neuroma; observed distal wallerian degeneration as evidence of axonal degeneration and shift to left in axon diameter population; pathologic process not sparing any components of the peripheral nerve; detailed degenerative activity plus some axon regeneration; Renaut’s bodies |
Lassmann, 1979 |
133 cases |
Endoneural vascular fibrosis |
Mann and Reynolds, 1983 |
65 specimens, 11 recurrent neuromas |
Similar degenerative changes; classic pathologic findings of neuromas a traumatic neuroma in recurrent lesions |
Graham and Graham, 1984 |
24 neuromas |
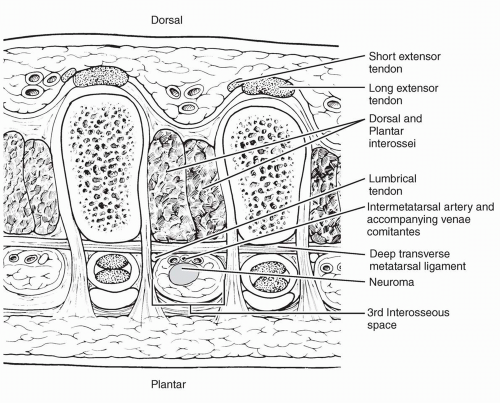
Venous congestion, entrapment changes, nerve enlargement distal to the transverse metatarsal ligament |
Guiloff, Scadding, and Klenerman, 1984 |
16 patients |
Similar degenerative changes: Renaut’s bodies common |
Shereff and Grande, 1991 |
10 specimens |
Edema of the endoneurium, fibrosis beneath the perineurium, axonal degeneration and necrosis characteristic of nerve impingement |
Bourke, Owen and Machet, 1994 |
15 patients |
“Except for possible demyelination, the so-called typical histologic changes of fibrosis and swelling are similar to that seen as presumed degenerative disease in elderly patients” |