Modified Bristow, Latarjet, and Allograft Capsular Reconstruction
G. Russell Huffman MD, MPH
James E. Tibone MD
The goal of any surgical technique treating glenohumeral instability is to afford a stable shoulder while preserving glenohumeral range of motion. The surgical approach to the patient’s instability is directed by the anatomy of the instability and by the functional demands placed upon the shoulder. For cases of traumatic anterior shoulder instability, either open or arthroscopic Bankart repairs remain the surgical procedure of choice. Failure rates for arthroscopic procedures approach the success obtained with open Bankart repairs with failure rates averaging 3% to 5%.1,2 The success of an “anatomic” instability repair, however, diminishes with the chronicity of glenohumeral instability and with the development of deficient anatomic restraints to instability.
There are several instances in which anterior capsulolabral reconstructions fail to address the anatomy of instability. The Bankart reconstruction fails to provide sufficient long-term shoulder stability in cases of: (a) severe glenoid bone loss; (b) engaging Hill-Sachs lesions; and (c) glenohumeral capsule attenuation from prior thermal treatment, failed instability surgery, connective tissue disorders, and chronic recurrent instability. This chapter discusses options to treat complex shoulder instability in cases of glenoid and humeral bone loss and in cases of capsular insufficiency.
Patient Evaluation
All patients should undergo a thorough history specifically addressing the onset and events surrounding their initial dislocation episode, the chronicity and number of instability events, positions that cause apprehension, current level of activity, and any prior stabilization procedures. It is extremely helpful to obtain copies of operative reports and intraoperative arthroscopy photos to better understand the status of the shoulder.
The physical examination focuses on ascertaining the direction of instability: anterior, inferior, posterior, or multidirectional. Additionally, associated pathology including superior labrum, anterior to posterior (SLAP) lesions, rotator cuff tears, scapulothoracic dysfunction, and neurological findings should be evaluated particularly after prior surgical treatment. The load and shift test is the preferred method for quantifying the degree of anterior instability as well as determining the competence and presence of the anterior band of the inferior glenohumeral ligament. In the anesthetized patient, obtaining a locked dislocation after the load and shift indicates a large bony lesion that may preclude Bankart repair. When treating patients with capsular attenuation, a careful assessment of restraints to anterior, posterior, and inferior translation is important. The posterior load and shift test and an assessment for inferior instability with observation of a sulcus sign in adduction and neutral rotation as well as in adduction and external rotation will indicate competency of the coracohumeral ligament, superior glenohumeral ligament, and rotator interval. If the sulcus sign is positive only in neutral rotation, then the interval is competent. If the sulcus remains positive after external rotation, the interval is loose and provides insufficient restraint to inferior instability. Generalized ligamentous laxity should also be assessed in each patient and comparison with the contralateral shoulder is essential in making the correct diagnosis.
Glenoid bone loss has been reported with an incidence as high as 80% and humeral impaction fractures in 70% of cases of chronic, recurrent anterior glenohumeral instability.3 Many of the bony glenoid lesions involve less than 20% of the glenoid width and may be treated with more standard approaches to instability surgery than discussed in this chapter.4 In most instances, glenoid and humeral bone loss are evident with standard radiographs. A true glenohumeral
anteroposterior (AP) projection and an internal rotation AP will reveal significant Hill-Sachs lesions. An apical oblique view is also useful in visualizing Hill-Sachs lesions.5 Although the axillary lateral radiograph is an important part of the initial trauma evaluation of a patient with shoulder instability, this view fails to adequately identify or to quantify sufficiently the degree of glenoid bone loss.6 The West-Point lateral7 or the glenoid profile lateral as described by Bernegeau et al.6 more accurately defines anterior inferior glenoid bone loss in all cases of traumatic instability. With the appropriate use of AP and the glenoid profile view, identification of bony defects is possible without the use of additional imaging modalities. However, when quantifying glenoid bone loss, computed tomography (CT) is the most precise imaging modality. In cases of revision instability surgery in which the amount of glenoid loss is uncertain, a CT scan may be useful. Additionally, in cases of combined glenoid and humeral bone loss, use of preoperative CT may allow the surgeon to appropriately plan for both anterior stabilization procedures as well as for addressing humeral bone loss. Magnetic resonance imaging (MRI) is not necessary in the routine assessment of instability patients. However, an MRI allows assessment of capsular integrity after thermal capsulorrhaphy and is useful in the preoperative assessment of the rotator cuff in patients over 40 with a history of traumatic instability.
anteroposterior (AP) projection and an internal rotation AP will reveal significant Hill-Sachs lesions. An apical oblique view is also useful in visualizing Hill-Sachs lesions.5 Although the axillary lateral radiograph is an important part of the initial trauma evaluation of a patient with shoulder instability, this view fails to adequately identify or to quantify sufficiently the degree of glenoid bone loss.6 The West-Point lateral7 or the glenoid profile lateral as described by Bernegeau et al.6 more accurately defines anterior inferior glenoid bone loss in all cases of traumatic instability. With the appropriate use of AP and the glenoid profile view, identification of bony defects is possible without the use of additional imaging modalities. However, when quantifying glenoid bone loss, computed tomography (CT) is the most precise imaging modality. In cases of revision instability surgery in which the amount of glenoid loss is uncertain, a CT scan may be useful. Additionally, in cases of combined glenoid and humeral bone loss, use of preoperative CT may allow the surgeon to appropriately plan for both anterior stabilization procedures as well as for addressing humeral bone loss. Magnetic resonance imaging (MRI) is not necessary in the routine assessment of instability patients. However, an MRI allows assessment of capsular integrity after thermal capsulorrhaphy and is useful in the preoperative assessment of the rotator cuff in patients over 40 with a history of traumatic instability.
All patients should undergo examination under anesthesia, including anterior and posterior load and shift, as well as assessment of inferior instability. The routine use of arthroscopic examination allows precise measurement of glenoid bone loss8 and an additional assessment of the appropriateness of arthroscopic stabilization techniques. The failure rate of arthroscopic stabilization when glenoid bone loss exceeds one fifth the glenoid width is 60%.8 Additionally, dynamic assessment of engaging Hill-Sachs lesions may be confirmed arthroscopically. In cases of capsular attrition from failed thermal capsulorrhaphy or failed instability procedures in patients with generalized ligamentous laxity, proceeding directly to open surgical treatment is appropriate.
Modified Bristow Technique
History of the Technique
In 1958 Helfet9 first described a technique of suturing the tip of the coracoid to the glenohumeral capsule and to the periosteum of the anterior glenoid in cases of recurrent anterior glenohumeral instability. Mead and Sweeney10 modified the procedure in 1964 to include rigid fixation of the bone block to the anterior glenoid rim with a screw. The transferred short head of the biceps and coracobrachialis provide a dynamic restraint to inferior and anterior instability, particularly in positions of glenohumeral abduction and external rotation. Additional restraint is provided by passing the bone block and conjoined tendon between the inferior one third and superior two thirds of the subscapularis, which prevents the subscapularis from ascending above the inferior aspect of the humeral head during abduction and shoulder external rotation. There is debate over the effectiveness of the bony process in providing an osseous restraint to dislocation.
Indications and Contraindications
Indications for the modified Bristow procedure include treatment of anterior instability in patients with bony glenoid defects exceeding 20% of the inferior glenoid diameter, patients with failed prior stabilization procedures and bony glenoid or humeral head deficits, and patients participating in contact sports with failed prior stabilization procedures. The procedure allows for preservation of external rotation. Coracoid transfer procedures should not be viewed as the initial stabilization procedure in patients with traumatic anterior instability in the absence of substantial glenoid defects or engaging humeral defects. In these instances, either an arthroscopic or open Bankart procedure should be utilized depending upon the technical abilities of the surgeon and the activity level of the patient. Contraindications to performing the Bristow include subscapularis tears and glenoid defects exceeding one third of the anterior glenoid.
Surgical Technique
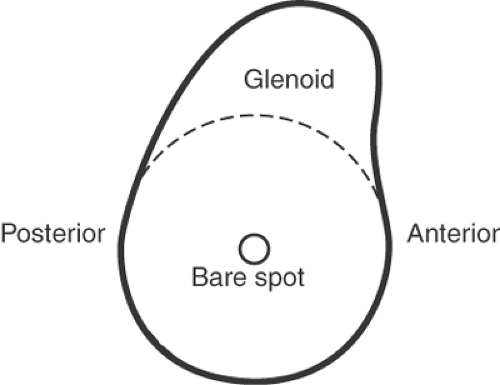
General anesthesia is used for this procedure. Supplemental regional blocks allow for lowered narcotic use and for the procedure to be performed in an outpatient setting when qualified anesthesia personnel are available. In cases in which the amount of anterior glenoid bone loss is questionable or additional diagnoses are suspected, the patient is placed in the lateral decubitus position and undergoes arthroscopic evaluation. The amount of bone loss is determined by identifying the bare spot in the center of the glenoid. A probe with markings is then used to measure the distance from the posterior aspect of the glenoid to the bare spot. This distance should be the same as the distance from the bare spot to the anterior aspect of the glenoid. The amount of anterior glenoid bone loss can then be measured (Fig. 18-1). In addition,
Burkhart et al.8 have described the inverted pear shape of the glenoid as an indication of glenoid bone loss. The normal shape of the glenoid is that of a pear, with the body of the glenoid being wider inferiorly and the superior portion being narrower. With glenoid bone loss, the pear shape is reversed or inverted. After arthroscopic findings confirm an indication for the Bristow procedure, the patient is repositioned supine, prepped with Betadine solution, and draped with an arm board positioned lateral to the operative shoulder. A small amount of reverse Trendelenburg is useful, however, the beach chair position is not necessary.
Burkhart et al.8 have described the inverted pear shape of the glenoid as an indication of glenoid bone loss. The normal shape of the glenoid is that of a pear, with the body of the glenoid being wider inferiorly and the superior portion being narrower. With glenoid bone loss, the pear shape is reversed or inverted. After arthroscopic findings confirm an indication for the Bristow procedure, the patient is repositioned supine, prepped with Betadine solution, and draped with an arm board positioned lateral to the operative shoulder. A small amount of reverse Trendelenburg is useful, however, the beach chair position is not necessary.
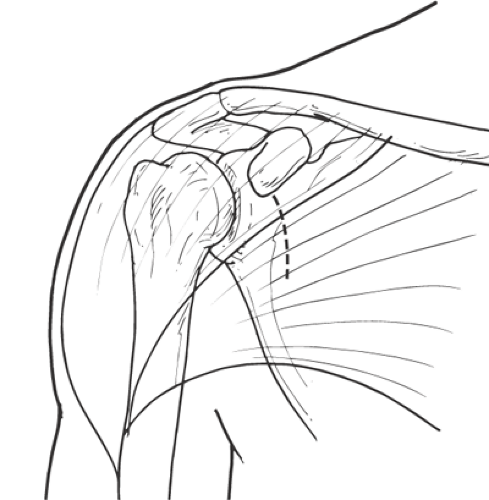
The incision is drawn from the tip of the coracoid to the axilla, in line with the axillary skin fold for cosmesis (Fig. 18-2). Prior to incision the skin and subcutaneous tissues are injected with a solution containing 1% Lidocaine and epinephrine. The incision is carried sharply through the skin and subcutaneous tissues to the level of the deltopectoral fascia. The cephalic vein is mobilized laterally with the deltoid. Next, the dissection is carried bluntly with the surgeon’s fingers through the deltopectoral interval superiorly to the coracoid tip to the base of the surgical incision. Deep hand-held retractors are used to improve exposure deep to the deltopectoral interval.
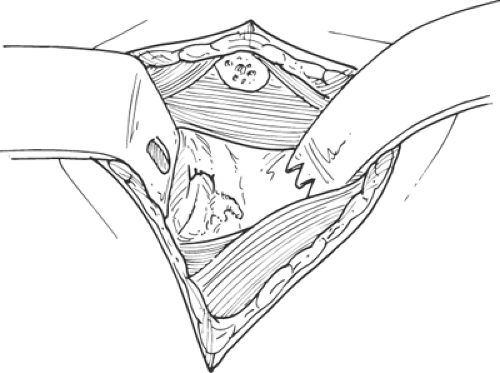
The conjoined tendon and the tip of the coracoid process are identified. The tip of the coracoid process is then exposed with electrocautery. At least a 1.5-cm block of bone should be exposed when measured from the anterior coracoid tip toward the base of the coracoid process. The anterior portion of the tendinous attachment of the pectoralis minor is released with an elevator or with electrocautery. The posterior attachment of the pectoralis minor insertion is preserved at the base of the coracoid process. A sharp 0.75-inch osteotome is then placed at least 1.5 cm posterior to the medial tip of the coracoid process (Fig. 18-3). The coracoid tip is cut from medial to lateral to avoid injury to the brachial plexus and musculocutaneous nerve medial to the coracoid. Bone wax is applied to the exposed cancellous portion of the remaining coracoid. Predrilling of the process prior to osteotomy is not necessary and may lead to eccentric drill hole placement or fracture during osteotomy.
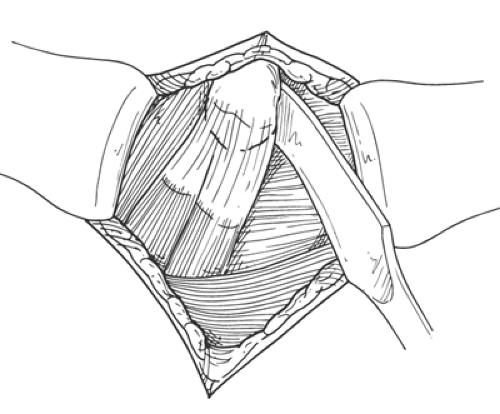 Fig. 18-3. Exposure of coracoid tip during the Bristow procedure with a 0.75-inch osteotome placed medially. At least 1.5 cm of bone should be transferred. |
The subscapularis and underlying anterior capsule are subsequently split in line with the muscle fibers of the subscapularis from its lateral insertion on the humerus to the medial portion of the glenoid neck. The muscle split is between the superior two thirds and the inferior one third of the subscapularis to allow inferior placement of the transferred coracoid tip. Splitting the subscapularis or, at a minimum, leaving the inferior portion of the subscapularis attached to the lesser tuberosity allows for early postoperative external rotation with the arm adducted and diminishes external rotation loss. A three-pronged retractor is then placed medially along the glenoid neck to afford visualization of the glenoid rim and neck as well as the anterior glenohumeral capsule. A second deep retractor is placed along the inferior glenoid rim within the subscapularis to protect the axillary nerve. The capsule is then incised horizontally in line with the subscapularis split with a T-shaped incision created along the glenoid neck to accommodate the transferred coracoid tip. Glenoid exposure is completed with posterior retraction of the humeral head with a small Fukuda humeral head retractor (Fig. 18-4).
The coracoid process is then drilled with a 2.5-mm drill to accommodate a partially threaded malleolar screw (Fig. 18-5). The drill enters the process beginning at the cancellous portion of the process and exits anteriorly, proximal to the conjoined tendon insertion to ensure placement of the screw in the central portion of the process. The coracoid process is transferred to the glenoid rim inside the anterior capsular. The ideal position of
transfer is within 5 mm of the glenoid rim and below the glenoid equator. The glenoid is then drilled from anterior to posterior through the posterior cortex of the glenoid. The screw is then placed through the tip of the coracoid and subsequently through both cortices of the glenoid (Fig. 18-6A,B). Care should be taken during this step not to fracture the coracoid process by overtightening the screw. The typical screw length to penetrate the posterior glenoid neck is 30 to 40 mm. In instances in which a small bone block is transferred, a washer is used to augment screw fixation.
transfer is within 5 mm of the glenoid rim and below the glenoid equator. The glenoid is then drilled from anterior to posterior through the posterior cortex of the glenoid. The screw is then placed through the tip of the coracoid and subsequently through both cortices of the glenoid (Fig. 18-6A,B). Care should be taken during this step not to fracture the coracoid process by overtightening the screw. The typical screw length to penetrate the posterior glenoid neck is 30 to 40 mm. In instances in which a small bone block is transferred, a washer is used to augment screw fixation.
Closure begins with approximation of the subscapularis. One or two interrupted no. 0 Vicryl (or similar weight absorbable suture) are used to close the subscapularis tendon loosely around the transferred coracoid tip. The muscle is not tightly reapproximated in order to prevent undo subscapularis tension. A tight interval closure surrounding the transferred coracoid process will lead to restricted subscapularis excursion and restricted glenohumeral external rotation. The deltopectoral interval typically requires no closure. The deep dermal layer and skin are closed using absorbable sutures in a subcutaneous fashion. Steri-strips and a sterile dressing are applied. A drain typically is not necessary. The patient is placed in a sling prior to awakening from anesthesia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree