Miscellaneous Orthopaedic Tests
Peripheral Arterial Insufficiency
Peripheral arterial insufficiency may involve both the upper and lower extremities. It may be due to obstruction, traumatic occlusion, arthrosclerosis, diabetes, Buerger’s disease, or Raynaud’s phenomenon. The patients who develop arterial insufficiency generally demonstrate one of three clinical patterns: (a) cold, cyanosed, livid and/or painful digits (Raynaud’s phenomenon); (b) digital ischemia; or (c) crampy pain on exercise (claudication). There is usually prolonged venous filling time following elevation of the extremity. The impaired flow or arterial insufficiency may be adequate to serve the metabolic activities of the muscles at rest but does not maintain the circulation necessary to the increased metabolic rates of exercise. Therefore, exercise testing, such as flexing and extending the arms and legs or walking, may reproduce the patient’s symptoms. Diagnosis is based on the combination of physical examination and vascular diagnostic testing, such as angiography, plethysmography, thermography, and vascular ultrasound.
Clinical Signs and Symptoms
Extremity pain
Cold extremities
Decreased pulse amplitude
Pallor or rubor
Hair loss
Shiny skin
Claudication
Gangrene
 |
Procedure
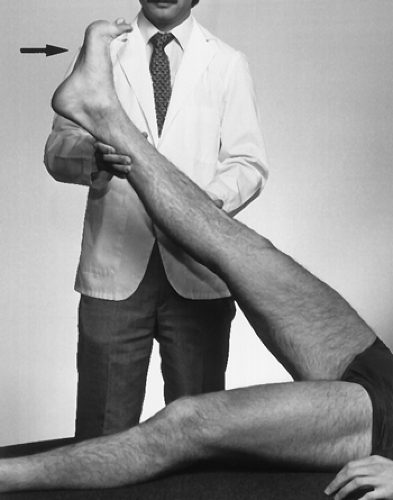
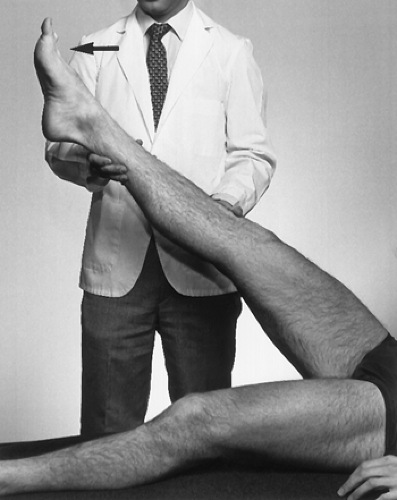
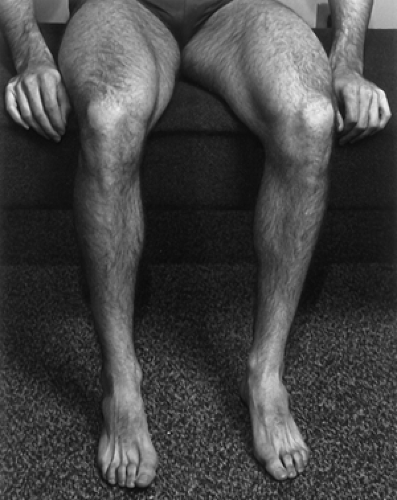
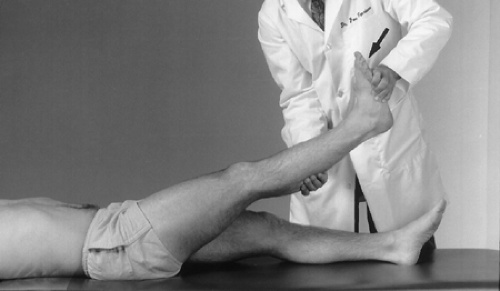
With the patient supine, instruct him or her to elevate one leg at a time. The patient must consecutively dorsiflex and plantar-flex the raised foot for a minimum of 2 minutes (Figs. 16-1 and 16-2). The leg is then lowered and hung off the side of the table with the patient seated (Fig. 16-3).
Rationale
Elevating and flexing the foot diminishes the blood flow in the lower extremity. When the leg is lowered and hung off the table, the lower leg and foot should fill with blood. This turns the foot a pinkish color, and the veins distend. This process takes less than 1 minute. If it takes longer, the test is positive for arterial compromise to the lower extremity.
 |
Procedure
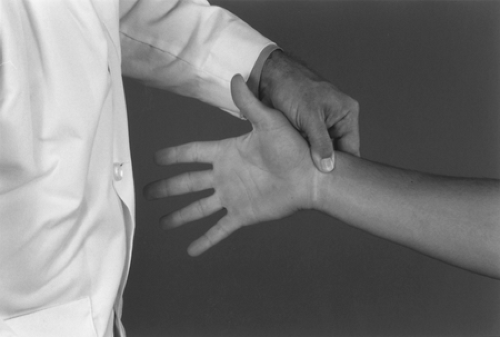
With the patient seated, occlude the radial and ulnar arteries with both thumbs (Fig. 16-4). Then instruct the patient to open and close the fist to express blood from the tissue (Fig.16-5). At that point, instruct the patient to open the hand as you release the pressure to the radial artery (Fig. 16-6). Repeat the test with the pressure released to the ulnar artery (Fig. 16-7).
Rationale
Consecutively opening and closing the fist diminishes the blood flow in the hand, causing blanching. When pressure on one of the arteries is released, the hand should fill with blood, which turns it a pinkish color, and the veins distend. A delay of more than 10 seconds in returning a pinkish color to the hand indicates either ulnar artery insufficiency or radial artery insufficiency. The artery being tested is the one not being manually occluded.
Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a cordlike clot formation that usually arises in the deep veins of the calf muscles. This venous occlusion results in edema and dependent cyanosis. The cause may be iatrogenic or result from a mechanical trauma that injured the endothelium of the veins, hypercoagulability associated with malignant tumor or oral contraceptives, or stasis that occurs with prolonged bed rest. If left untreated, approximately 20% of thrombi may extend into the proximal venous system and pose a serious and even life-threatening risk of a pulmonary embolism: 90% of pulmonary emboli originate in the deep venous system of the legs.
Clinical Signs and Symptoms
Leg pain
Leg swelling
Leg tenderness
Local temperature elevation
Discoloration
Venous distension
Palpable cord (thrombosed vessel)
 |
Rationale
Deep-seated pain at the posterior leg or calf may indicate thrombophlebitis. Dorsiflexing the foot places a dynamic stretch on the gastrocnemius muscle and tension of the deep veins. The addition of squeezing the calf compresses the surrounding tissue against the thrombus, stimulating a nociceptive response.
Somatosensory Amplification Assessment
Somatosensory amplification is usually a misrepresentation of the patient’s symptoms. It is seen in patients with hypochodriasis, patients with extreme anxiety disorder, or feigned for secondary gain. This is a very difficult assessment. Although this condition is most common in the setting of workers compensation and personal injury cases, the secondary gain may not be financial alone. It may occur if individuals desire a less strenuous job at work. They may gain control over fellow workers or family members. The injured party may allow others to do work that the patient would normally do.
The possibility of symptom magnification should be raised when major discrepancies or inconsistencies appear in the patient’s condition. These inconsistencies are most noted in history and physical examination. Some examples of these inconsistencies: (a) dramatized complaints that are vague or global, (b) overemphasized gait or postural abnormalities, (c) resistance to evaluation or rehabilitation, and (d) lack of motivation to develop new skills or lack of treatment compliance.
Once the information has been collected, a determination of symptom magnification may be made. This is difficult because very few symptom magnification cases are totally without pain or fear of being placed in a job perceived as potentially harmful. Second opinions are quite useful if you suspect symptom magnification. Concurrence by more that one physician is prudent in these cases.
Clnical Signs and Symptoms
Discrepancy between patient’s presentation and degree of reported pain
Negative workup for organic problems by multiple physicians
Dramatized complaints that are vague or global
Overemphasized gait or posture
Resistance to evaluation
Resistance to rehabilitation
 |
Procedure 1 (Non-Anatomic Tenderness)
Examiner palpates the area of complaint with light touch (Fig. 16-9).
Rationale
The patient reports disproportionate pain in response to light touch and distribution does not correlate to known anatomic structures.
Procedure 2 (Simulation Sign)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree