Lumbar Nerve Root Lesions
T12, L1, L2, L3
Clinical Description
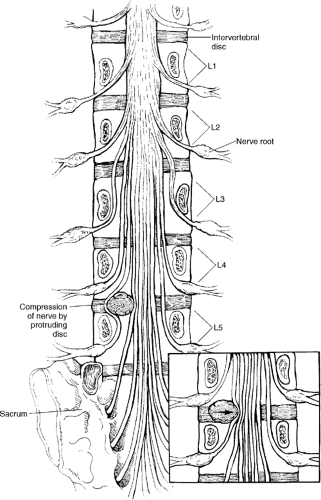
Nerve roots in the lumbar spine exit the spinal column through laterally placed intervertebral foramina. The nerve roots in the lower thoracic and lumbar spine gradually exit their intervertebral foramen at its upper aspect. This causes the nerve root in these areas to be affected by
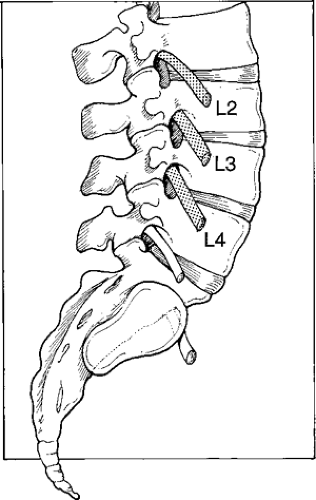
the intervertebral disc above the exiting nerve root (Fig. 11-1). The lower thoracic area and upper lumbar area (T12–L2) are transitions to this anatomic consideration and in this area may be affected either by the intervertebral disc at the same interval or the disc at the level above the exiting nerve root. This situation may depend on the laterality of the disc defect. The L3 to L5 nerve roots exit the intervertebral foramen at the upper end of the foramen 80% of the time, and they are usually affected by the intervertebral disc above the exiting nerve root. Because of its anatomic position, the S1 nerve root is usually affected by the L5–S1 intervertebral disc. If a lumbar nerve root lesion is suspected, you must evaluate three clinical aspects of the neurological examination: sensory dysfunction, motor dysfunction, and reflex dysfunction.
the intervertebral disc above the exiting nerve root (Fig. 11-1). The lower thoracic area and upper lumbar area (T12–L2) are transitions to this anatomic consideration and in this area may be affected either by the intervertebral disc at the same interval or the disc at the level above the exiting nerve root. This situation may depend on the laterality of the disc defect. The L3 to L5 nerve roots exit the intervertebral foramen at the upper end of the foramen 80% of the time, and they are usually affected by the intervertebral disc above the exiting nerve root. Because of its anatomic position, the S1 nerve root is usually affected by the L5–S1 intervertebral disc. If a lumbar nerve root lesion is suspected, you must evaluate three clinical aspects of the neurological examination: sensory dysfunction, motor dysfunction, and reflex dysfunction.
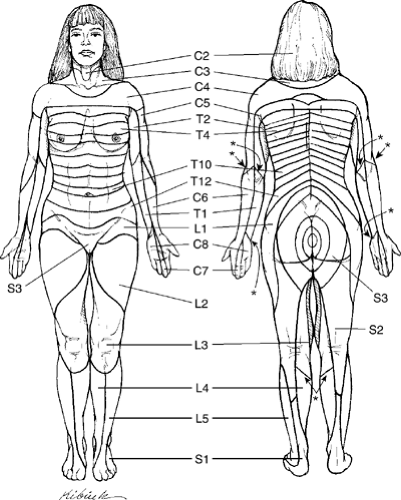
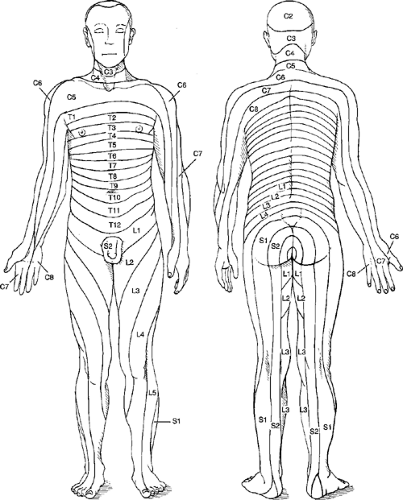
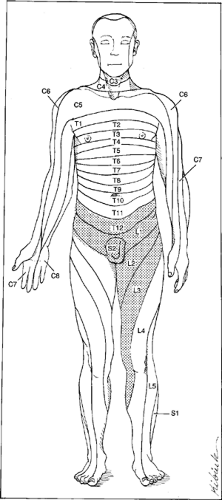
The sensory deficit evaluation addresses the segmental cutaneous innervation of the skin. It is tested with a sterile or disposable Neurotip or pinwheel in specific dermatomal patterns. Two dermatomal maps are provided here. Figure 11-2 indicates the body areas of intact sensation when roots above and below an isolated root are interrupted, sensation loss when one or more continuous roots are interrupted, or the pattern of herpetic rash and hypersensitivity in isolated root involvement. Figure 11-3 presents the hyposensitivity to pin scratch in various root lesions and is consistent with electrical skin resistance studies showing axial dermatomes extending to the distal extremities. This pattern is useful in evaluating paresthesias and hyperesthesias secondary to root irritation. This is the pattern that will be delineated to evaluate sensory root dysfunction. Since a fair amount of segmental overlap exists, a single unilateral lesion may affect more than one dermatomal level. Motor function is tested by evaluating the muscle strength of specific muscles innervated by a particular nerve root or roots using the muscle grading chart adopted by the American Academy of Orthopaedic Surgeons (Box 11-1). The reflex arc is tested by evaluating the superficial stretch reflex associated with the particular nerve root. These reflexes are graded by the Wexler scale (Box 11-2).
Box 11-1 Muscle Grading Chart
| 5 | Complete range of motion against gravity with full resistance |
| 4 | Complete range of motion against gravity with some resistance |
| 3 | Complete range of motion against gravity |
| 2 | Complete range of motion with gravity eliminated |
| 1 | Evidence of slight contractility; no joint motion |
| 0 | No evidence of contractility |
The clinical presentation of nerve root lesions depends on two important factors: the location and the severity of the injury or pathology. These two factors determine the lesion’s clinical presentation. The possibilities range from no clinical signs or slight clinical manifestation, such as slight loss of sensation and pain, to total denervation with complete loss of function (motor, sensory, and reflex) in the structures innervated by the involved nerve root. Each nerve root has its own sensory distribution, muscle test or tests, and a stretch reflex, which will be grouped to facilitate identification of the suspected level.
The clinical evaluation is not made solely on one aspect of the neurological package but is determined by the combination of history, inspection, palpation, the three individual tests (motor, reflex, and sensory), and appropriate diagnostic imaging and/or functional neurological testing, such as electromyography. Furthermore, the injury or pathology may not necessarily affect a nerve root; it may affect the lumbar plexus, a trunk of that plexus, or a named nerve. Depending on the severity and location of the injury or pathology, various combinations of neurological dysfunction may be revealed.
T12, L1, L2, L3
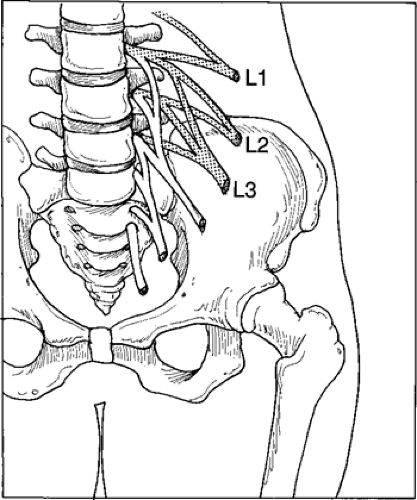
The T12, L1, L2, and L3 nerve roots exit the spinal canal at their respective levels. The T12 and L1 nerve roots can be affected by the intervertebral disc at their respective levels or levels above them, depending on the size and laterality of the disc defect (Fig. 11-4).
Iliopsoas: T12, L1, L2, L3 Nerve Root Innervation
Procedure
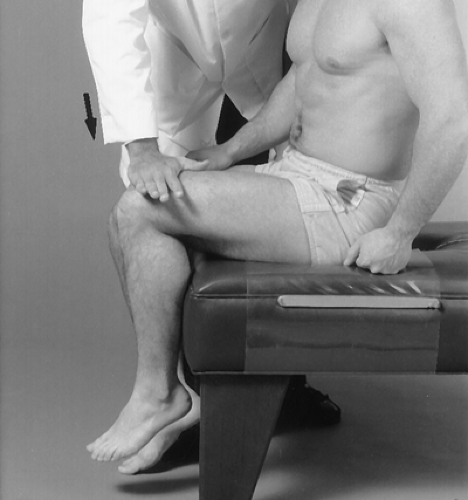
With the patient sitting at the edge of the examination table, instruct the patient to raise the thigh off the table. Place your hand on the patient’s knee and instruct the patient to continue to raise the thigh against your resistance (Fig. 11-5). Perform the test on the opposite thigh. Grade according to the muscle grading chart and evaluate bilaterally.
Reflex
There is no reflex test.
Procedure
With a pin, stroke the dermatomal area corresponding to each nerve root (Fig. 11-6) and evaluate bilaterally.
L2, L3, L4
The L2, L3, and L4 nerve roots can be affected by the intervertebral disc at their respective levels or levels above them, depending on the size and laterality of the disc defect (Fig. 11-7).
Quadriceps Muscle: L3, L4 Femoral Nerve Innervation
Procedure
With the patient sitting at the edge of the examination table, instruct the patient to extend the knee. Place one hand on the patient’s thigh for stabilization and place the other hand on his or her leg. Exert pressure on the leg while instructing the patient to resist flexion (Fig. 11-8). Grade according to the muscle grading chart and evaluate bilaterally.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree