Mini-Open Achilles Tendon Repair: Perspective 1
Mathieu Assal
Marc Merian-Genast
Mark E. Easley
DEFINITION
Achilles tendon ruptures usually occur 3 to 4 cm above the calcaneal tuberosity.
Although most injuries are “complete“ ruptures, “partial“ injuries have been described.
ANATOMY
The Achilles tendon is about 9 cm long and 0.9 cm in diameter.
The proximal part is composed of the gastrocnemius and soleus tendons.
The distal portion inserts onto the posterior aspect of the tuberosity of the calcaneus.
The Achilles tendon is surrounded by the paratenon, a delicate envelope that contributes to tendon vascularization.
There is an area of poor vascularity located between 2.5 and 5 cm above the calcaneal tuberosity.
PATHOGENESIS
Rupture of the Achilles tendon is a common injury among high-level athletes, recreational sports enthusiasts, or even sedentary individuals.
Rupture of the Achilles tendon usually occurs during forceful dorsiflexion of the ankle.
Patients often describe hearing or feeling a “pop“ in the back of their ankle.
Intratendinous degeneration can be found histologically.
Association with cortisone and fluoroquinolone use has been demonstrated.
This is typically a lesion of middle age, with peak incidence during the third and fourth decades.
NATURAL HISTORY
There is a great deal of controversy concerning the treatment of an acute rupture of the Achilles tendon.
Conservative treatment is found to have a higher rate of tendon rerupture and loss of strength because the tendon heals in an elongated position.
The major factor motivating surgeons to use a nonoperative approach appears to be avoiding the wound complications that occur with an operative repair.
An increasing number of reports in the literature have tended to favor operative treatment of an acute rupture of the Achilles tendon.
The exact type of operative procedure and the postoperative regimen remain controversial. Mini-invasive techniques are associated with a lower complication rate.
If soft tissue complications are avoided, excellent functional results and full return to previous activity can be expected.
PHYSICAL FINDINGS
Physical examination reveals moderate swelling about the posterior aspect of the ankle.
Patients are usually able to walk, although with moderate pain.
With the patient prone, spontaneous excess dorsiflexion of the involved ankle is noted.
In most cases, a tender defect (“soft spot“) can be palpated in the Achilles tendon between 2.5 and 5 cm proximal to its insertion into the calcaneal tuberosity.
The Thompson squeeze test is positive.
Patients have difficulty walking on their toes or rising up on their heels.
IMAGING AND DIAGNOSTIC STUDIES
History and physical examination are sufficient to confirm the diagnosis.
Because these injuries occur in a traumatic setting, plain radiographs of the ankle are strongly advised.
There have been many reports of associated ankle fractures (medial malleolus).
Calcaneal (tuberosity) avulsion will appear on the lateral view.
Ultrasound and magnetic resonance imaging (MRI) are not required for the diagnosis of Achilles tendon rupture but may be of value when the diagnosis is questionable.
DIFFERENTIAL DIAGNOSIS
Ankle sprain
Ankle fracture
Tennis leg (gastrocnemius tear)
Acute paratenonitis
Calcaneal (tuberosity) avulsion
Plantaris tendon rupture
NONOPERATIVE MANAGEMENT
Nonoperative treatment of acute Achilles tendon ruptures involves prolonged immobilization.
Prolonged immobilization is associated with musculoskeletal changes (atrophy), increased time necessary for rehabilitation, and delayed return to work and preinjury activities.
In randomized studies, the rerupture rate has been found to be much higher in the nonoperative group.
However, nonoperative treatment avoids surgical complications.
Nonoperative treatment should be considered in elderly patients with limited functional expectations, patients with significant tobacco or alcohol addictions, patients receiving chronic cortisone treatment, patients with vascular disease, and patients with severe comorbidities such as renal failure.
Indications and Contraindications
The indication for this technique is an acute (<3 weeks)
Achilles tendon rupture, occurring 2 to 7 cm above the tuberosity of the calcaneus.
Over 90% of ruptures of the Achilles tendon occur in the area 2 to 8 cm above the calcaneal tuberosity.
We believe that ruptures occurring more than 8 cm above the tuberosity (muscular ruptures) can be treated nonoperatively and ruptures occurring less than 2 cm from the tuberosity necessitate fixation directly to bone.
Contraindications include chronic rupture greater than 3 weeks in duration, previous local surgery, steroid use, open ruptures and lacerations greater than 6 hours in duration, complex open ruptures with soft tissue defects, and ruptures not occurring between 2 and 8 cm above the tuberosity of the calcaneus.
SURGICAL MANAGEMENT
Preoperative Planning
Plain films should be reviewed for fracture, avulsion, and calcific tendinopathy.
All imaging studies are reviewed.
An examination under anesthesia should be performed before positioning the patient to reconfirm the side of injury.
Positioning
The patient is placed prone on the operating table.
A tourniquet is applied around the upper thigh.
Both legs are included in preparation and draping to compare Achilles tendon tension and spontaneous plantarflexion intraoperatively.
Plastic draping is not used (the technique involves percutaneous steps).
Patients receive antibiotic prophylaxis.
Instrumentation
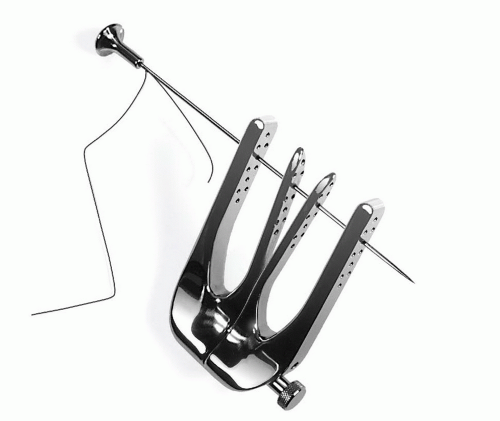
The Achillon (Integra LifeScience, Plainsboro, NJ) was designed by Matthieu Assal and is made of either a rigid polymer or stainless steel (FIG 1).
It is designed to guide the passage of the sutures.
It is composed of a pair of internal branches connected to a pair of external branches, with each branch having a line of apertures at the same level to allow easy and accurate passage of the sutures through all four branches.
The two internal branches are at an 8-degree angle to each other, following the V-shaped anatomic form of the tendon.
A micrometric screw allows for varying the opening of the branches according to tendon morphology.
A straight needle loaded with a suture is passed through the device, soft tissues and tendon. A cap for the needle facilitates applying pressure to the end of the needle.
TECHNIQUES
▪ Open Repair Illustrated
Exposure
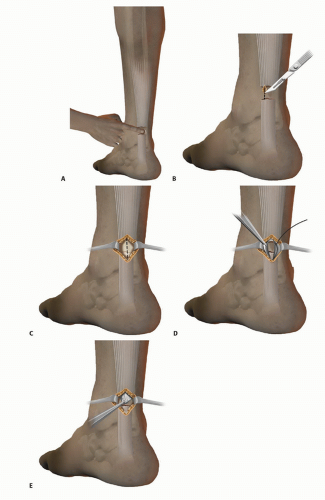
Palpate the site of injury, represented by the gap or soft spot (TECH FIG 1A).
The incision is paratendinous and medial (TECH FIG 1B), beginning at the soft spot and extending about 2.0 cm proximally.
Gently retract the skin and subcutaneous tissue with hooks and identify the paratenon (TECH FIG 1C).
Carefully open the sheath and tag each edge with a stay suture (TECH FIG 1D).
Identify both stumps of the ruptured tendon (TECH FIG 1E) and carefully note the exact site of rupture.
Introducing the Achillon
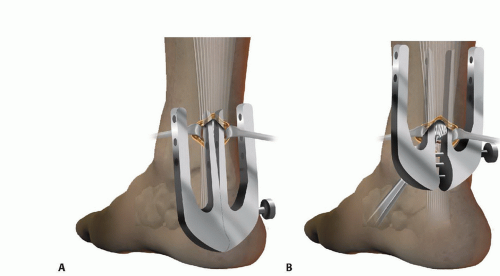
Introduce the Achillon in the closed position under the paratenon in a proximal direction, holding the tendon stump with a small clamp under the instrument (TECH FIG 2A).
The tendon stump is located between the two internal branches (TECH FIG 2B).
As the instrument is introduced, progressively widen it, holding the tendon stump firmly with the clamp.
Confirm the position of the guide by external palpation; you should feel the tendon between the central (internal) branches of the instrument.
Suturing
Pass three sutures from lateral to medial, usually beginning with the most proximal hole of the instrument (TECH FIG 3A,B).
Hold the end of each suture with a small clamp to keep them separate from each other.
Slowly withdraw the instrument while progressively closing the branches (TECH FIG 3C).
This maneuver results in the sutures sliding from an extracutaneous position to a peritendinous position, and thus the tendon itself is the only tissue held by the sutures (TECH FIG 3D).
Apply traction to the three suture pairs to ensure they are firmly anchored in the tendon and individually clamp them to prevent any confusion.
TECH FIG 2 • A,B. Introduction of the instrument proximally under the paratenon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access