Midfoot Fractures
Travis A. Motley
Brian B. Carpenter
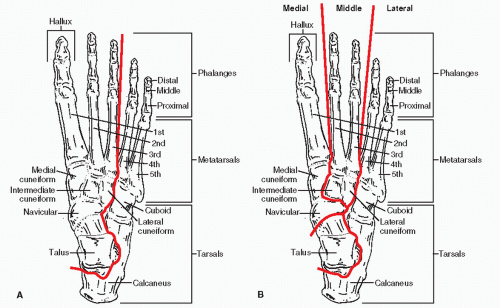
The navicular, cuboid, and cuneiform bones make up the midfoot. The midfoot has been described in several ways for understanding injury patterns and for relation to reduction and fixation techniques. Early and Hansen (1) describe midfoot bones to comprise portions of both the medial and lateral longitudinal columns of the foot. The medial longitudinal column includes the talus, navicular (keystone), three cuneiforms, and corresponding metatarsals. The lateral longitudinal column includes the calcaneus, cuboid, and corresponding metatarsals. Another version (2) uses a three-column description with the medial column of the navicular, medial cuneiform, and first metatarsal; middle column of the second and third metatarsals and cuneiforms; and the lateral column of the calcaneus, cuboid, and fourth and fifth metatarsals (Fig. 105.1). In all descriptions, the stability of the foot is dependent upon the alignment and strength of all columns: each supports the other and injury to one column likely involves injury to and requires stabilization of the other columns (3). Considering the interdependence of the longitudinal columns, it is extremely difficult to sustain an isolated injury at any level in any of the longitudinal column models without disruption of the bony and/or ligamentous anatomy of other columns.
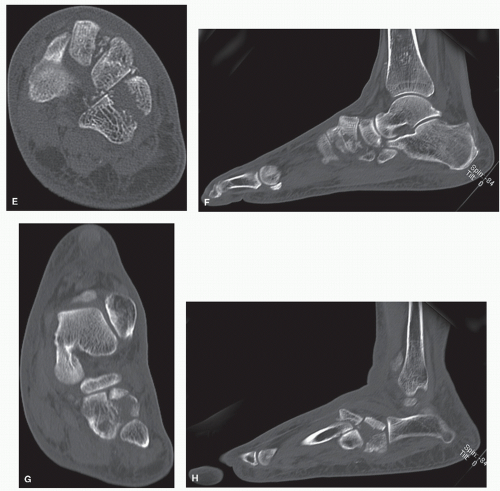
Acute midfoot injuries are quite rare and can have unusual patterns. Injuries to the individual midfoot bones usually occur in a complex with other injuries, both bony and ligamentous. Injuries occurring in multiple bones and ligaments of the midfoot, such as Chopart joint injuries, are rare as well when compared with all foot and ankle trauma. These are injuries that may or may not be initially evaluated, especially in the polytrauma patient. Midfoot injuries can be subtle on plain films because spontaneous reductions occur. These relatively benign findings on plain films necessitate the practitioner to further evaluate the foot with subsequent magnetic resonance imaging (MRI) or computerized tomography (CT) imaging, which will usually show more significant injury patterns (Fig. 105.2).
Initial evaluation of suspected midfoot injuries includes neurovascular, dermatologic, and musculoskeletal exam. Neurovascular evaluation includes consideration of compartment syndrome. Dermatologic exam includes notation of lacerations for open injuries as well as tented skin or fracture blisters. Musculoskeletal exam includes evaluation for any gross deformities, muscle strength testing, and isolated midfoot range of motion/instability testing.
Radiographic examination includes plain radiographs of anteroposterior, lateral, and oblique projections. Since midfoot injuries can often be missed on plain films, CT imaging is indispensable. However, since midfoot injuries, especially those with insidious onset of pain, can include stress fractures and soft tissue injuries, MRI may be necessary. Nuclear medicine can also be utilized for suspected stress injuries, but the overall value of this study is less compared with CT or MRI.
In general, initial treatment of midfoot injuries should include attempted reduction of gross deformities by closed manipulation. Closed reduction techniques are often very difficult and can be complicated by intervening soft tissue structures. The practitioner must always be aware of surrounding neurovascular structures in the anatomic neighborhood prior to attempted closed reduction as these structures may become more traumatized or entrapped with reduction. Initial treatment also includes stabilization through a bulky splint to decrease edema. Constant attention to the soft tissue envelope will allow a quicker surgical reduction and less postoperative incisional problems.
Neglected or delayed diagnosis of the midfoot results in poorer patient outcomes. Complex midfoot injuries are generally high-energy injuries that carry significant long-term sequelae, whereas patients sustaining isolated midfoot injuries have less long-term impairment (4). Nonacute isolated injuries to the midfoot are sparsely reported in the literature. There is more data in the literature for complex midfoot injuries. A common theme in the literature is that the practitioner must have a high index of suspicion for midfoot injuries, especially in those patients with insidious onset of pain. If pain is located in the midfoot region and initial radiographic findings are normal, it is imperative to continue with other radiographic evaluation, and a midfoot injury must be ruled out.
Throughout this chapter, articles are summarized to substantiate certain points. However, most midfoot injuries are not isolated and are part of a complex of injuries such as Chopart or Lisfranc patterns (Fig. 105.3). When discussing independent injury to bones of the midfoot, the reader should know that the literature is relatively sparse. Navicular injuries are the exception and have been described in several large published studies. The bottom line is that the reader should consider these isolated individual midfoot bone injuries to be the exception, not the rule.
NAVICULAR INJURIES
The navicular is the most commonly reported bone injured in the midfoot. The navicular is a comma-shaped bone that is the keystone of the medial longitudinal column. It is widest medially at the tuberosity and tapers laterally. Articular cartilage covers the concave proximal surface for articulation with the talus, the convex distal surface for articulation with the cuneiforms, and the lateral tail for occasional articulation with the cuboid. All cuneiforms share a single synovial joint with the navicular. Vascular supply of the navicular includes branches of the dorsalis pedis artery dorsally, branches of the medial plantar artery plantarly, and from an anastomosis between the dorsalis pedis and the medial plantar arteries to the tuberosity medially. This pattern creates a watershed area in the central portion of the bone (5) (Fig. 105.4).
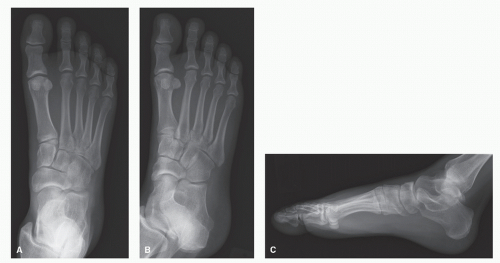 Figure 105.2 A-C: AP, oblique, and lateral views demonstrate subtle findings of fractures of the third and fourth metatarsal bases. (Continues on next page) |
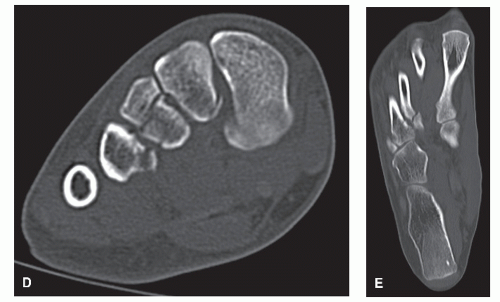 Figure 105.2 (Continued) D,E: Frontal and transverse plane CT scans demonstrate further injury across the Lisfranc joint complex. |
 Figure 105.3 A-C: Plain radiographs showing disruption across the midtarsus. D-H: CT imaging shows significant injury patterns to the metatarsals, cuneiforms, and cuboid. |
Navicular stress (incomplete) fractures were once thought to be quite rare, but the increase in index of suspicion has also increased the diagnosis (6). Numerous predisposing factors have been implicated in the development of navicular stress fractures: pes cavus, short first metatarsal, metatarsus adductus, limited subtalar or ankle motion, and medial narrowing of the talonavicular joint. No study has demonstrated a statistical significance to any of these theories (6).
Pain is usually described as worse during and after physical activity. Activities that exacerbate this pain are those associated with pushing off such as jumping and starting from a stationary position. Active patients may relate a change in training modalities or shoes. Pain can be generalized at the beginning of the injury, but as time progresses, it is often localized to the dorsum of the navicular bone (6). Pain can be aggravated with pressure over the dorsal central navicular by single-leg heel raise
or by single-leg hopping (7). If a patient, especially an athlete, complains of pain with insidious onset in the navicular region, a stress fracture must be ruled out, even with normal radiographs (6). A prior study demonstrated that plain radiographs may be normal acutely and no changes may be evident for three to 6 weeks after initial navicular injury (8). In comparison of stress fractures among athletes, navicular stress fractures accounted for 14% to 15% of all pedal stress fractures (9,10).
or by single-leg hopping (7). If a patient, especially an athlete, complains of pain with insidious onset in the navicular region, a stress fracture must be ruled out, even with normal radiographs (6). A prior study demonstrated that plain radiographs may be normal acutely and no changes may be evident for three to 6 weeks after initial navicular injury (8). In comparison of stress fractures among athletes, navicular stress fractures accounted for 14% to 15% of all pedal stress fractures (9,10).
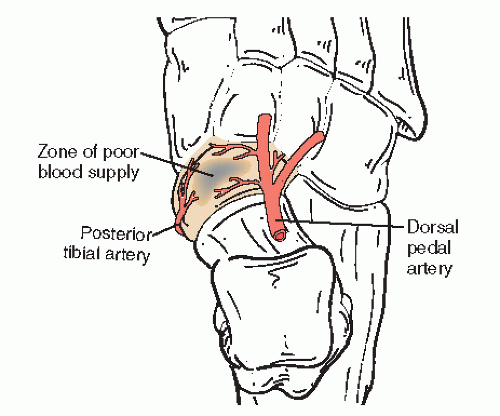 Figure 105.4 Schematic of the blood supply of the navicular with watershed area in the central third. |
Classification systems for navicular stress fractures exist for plain weight-bearing radiographs based on lucency and callus formation (11) and CT imaging based on the cortices involved (12). Plain radiograph classification is typically less reliable as these injuries may be subtle and missed. CT classification is more widely used and provides information in developing a treatment plan. The Saxena et al (12) CT classification is based on a retrospective review of 22 navicular stress fractures with an average follow-up of 36.5 months. Type I (incomplete) injury involves the dorsal cortex only. In a type II (incomplete) pattern, the fracture runs from the dorsal cortex into the navicular body. In type III (complete), the fracture line is through both dorsal and plantar cortices (Fig. 105.5). The following are the recommended treatments based on this classification: type I, conservative treatment or open reduction internal fixation (ORIF) in athletes; type II, conservative treatment or ORIF in active/athletic patients; and type III, most often ORIF. Average return to activity time for both nonoperative treatment and ORIF of type I was 3.0 months; type II, 3.6 months; and type III, 6.8 months. Those patients that underwent ORIF demonstrated a statistically significant quicker return to activity than those with conservative treatment. Recommendations were for early ORIF of navicular stress fractures involving more than the dorsal cortex to allow a quicker return to activity. Furthermore, Saxena et al (12) evaluated an adjunct of pulsed electromagnetic field (PEMF) bone stimulators in some patients and noted that patients utilizing PEMF healed slower than those without PEMF.
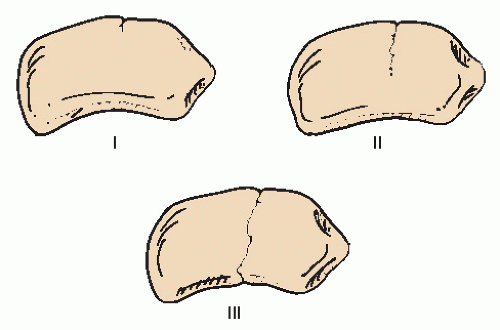 Figure 105.5 Navicular classification of type I, II, and III described by Saxena (12). |
Navicular stress fractures should be treated as complete fractures. If the fracture has minimal bone involvement, conservative treatment is favorable. If the fracture is more extensive or has been determined to be nonunited, treatment favors surgical intervention. Conservative treatment is a minimum of 6 weeks non-weight-bearing in cast or boot immobilization. Previous studies show good results with both conservative and surgical treatment of navicular stress fractures, although all authors did not distinguish between different types of injuries. Keeping that in mind, some have demonstrated that conservative care, including activity modification, is a viable option in treatment of navicular stress fractures. In a retrospective review of 21 navicular stress fractures, patients treated with initial nonweight-bearing cast immobilization for 6 to 8 weeks resulted in 100% success rate with an average return to activity at 3.8 months (13). In a series of 86 navicular stress fractures that were confirmed with CT and initially treated for 6 weeks in nonweight-bearing cast, 86% returned to full activity in 5.6 months. When patients were casted for 2 to 5 weeks, 69% returned to full activity. Activity restriction without casting resulted in 50% returning to full activity. Without activity restriction, only 20% returned to full activity (14). Other series note some patients require up to 8 months to return to full activity when treated with conservative therapy alone (15).
After surgical intervention or initial conservative treatment, subsequent physical exam including direct pressure over the proximal dorsal navicular will determine if a continued course of non-weight-bearing and immobilization is necessary. If pain has resolved, weight-bearing can resume with physical therapy and return to activity as tolerated. If pain persists, protected weight-bearing and repeat radiographic exam is indicated. Plain radiographs can show subtle signs of healing but serial MRI or CT imaging are more sensitive and specific to follow marrow edema and trabecular patterns.
Some authors claim that dislocation of the navicular without associated fracture is an anatomical impossibility (16). Others describe a mechanism that is usually a plantarflexion/compressive injury that can crush the navicular and may displace the fractured bone from proximal and/or distal articulations (17). This displacement occurs with a longitudinally directed force compressing the navicular, in addition to an abduction/plantarflexion injury (18). In a series of six navicular dislocations without fracture of the body of the navicular, all patients were found to have considerable disruption of soft tissue and bony structures of the midfoot (3). All patients had some form of lateral injury with either fracture subluxation of the calcaneocuboid joint or frank midtarsal dislocation. They (3) presumed that with an abduction/pronation injury, the midfoot initially breaks at the naviculocuneiform joint in the medial column; the force also causes a break at a similar point laterally at either the calcaneocuboid joint or lateral tarsometatarsal joint to produce an occult or frank midtarsal dislocation. The forefoot
displaces either superolaterally or inferolaterally, depending on the deforming forces, and the subsequent relocation of the forefoot then pushes the navicular from the talonavicular joint. Depending on the direction of the forces, as well as the residual soft tissue attachments to the bone, the navicular can be dislocated to various positions medially. If the deforming force leads to forced plantarflexion, dorsal displacement of the fractured navicular will occur (19) (Fig. 105.6). To produce a complete dislocation of the navicular without fracture, a midtarsal dislocation or subluxation (complete or transitory) must occur (3).
displaces either superolaterally or inferolaterally, depending on the deforming forces, and the subsequent relocation of the forefoot then pushes the navicular from the talonavicular joint. Depending on the direction of the forces, as well as the residual soft tissue attachments to the bone, the navicular can be dislocated to various positions medially. If the deforming force leads to forced plantarflexion, dorsal displacement of the fractured navicular will occur (19) (Fig. 105.6). To produce a complete dislocation of the navicular without fracture, a midtarsal dislocation or subluxation (complete or transitory) must occur (3).
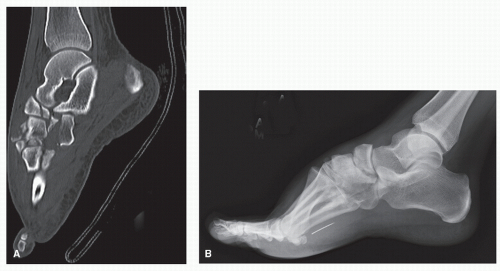 Figure 105.6 When the deforming injury force leads to forced plantarflexion, dorsal displacement of the navicular may occur.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|