Metatarsus Adductus and Allied Disorders
Patrick S. Agnew
NOMENCLATURE
The term metatarsus adductus was described by Ganley and Ganley (1) as being the least cumbersome and most accurate description of the shared component (adduction of the metatarsal bones) present in a group of disorders. Extensive controversy surrounds the subject of metatarsus adductus. This controversy persists because no study has provided complete answers to some basic questions. These questions include the etiology, prognosis, and treatment of this condition.
Even the terminology is debatable (2). Some authors prefer the terminology used in ancient anatomic dissections of a fresh cadaver executed by hanging, in which the foot is in a varus position (3). The more practical approach is to describe the condition in terms of the functional anatomy (i.e., the appearance of the weight-bearing foot). The issue of terminology is further complicated by the existence of several major variations of metatarsus adductus and countless shades of penetrance. The basic list of foot deformities that possess metatarsus adductus as an obvious characteristic includes metatarsus adductus, metatarsus adducto varus, cavoadducto varus, cavometatarsus adductus (also known as serpentine or Z-foot), and talipes equinovarus (4). Talipes equinovarus often includes metatarsus adductus as a component, along with forefoot adductus, and is discussed in Chapter 29.
Metatarsus adductus as an isolated deformity is characterized by a uniplanar, adducted metatarsus. It may be differentiated from other complex deformities such as talipes equinovarus by the absence of rearfoot deformity associated with the metatarsus adductus deformity (Fig. 73.1). However, the apex of the metatarsus adductus deformity may vary from the metatarsal diaphysis to the rear area of the midtarsus. Isolated metatarsus primus adductus may also present similarly, but it lacks the prominence of the styloid process of the fifth metatarsal.
Metatarsus varus includes varying amounts of metatarsus adductus but also demonstrates forefoot varus in the open kinetic chain (5). The rearfoot is normal, at least until weightbearing is initiated, and produces either uncompensated, partially compensated, or compensated forefoot varus (6). In the case of the latter (fully compensated forefoot varus), the rearfoot must pronate.
Cavoadducto varus includes metatarsus adductus and rearfoot varus. This condition is more commonly acquired from neuromuscular disease (7) (Fig. 73.2).
The compensated metatarsus adductus foot occurs when metatarsus adductus is accompanied by varying amounts of rearfoot pronation. In a fully compensated metatarsus adductus deformity, the foot may appear almost normal (Fig. 73.3). Subdivisions of compensated metatarsus adductus have been described by Berg (8), who detailed the apexes of the deformity. Forefoot and midfoot deformity is termed cavometatarsus adductus. Forefoot and hindfoot deformity is termed skewfoot. Complex skewfoot includes extensive deformity throughout the foot.
Other terms used have included parrot foot, pigeon toe, ding foot, C-foot, and hooked foot (5). Standardized terminology is preferred and is necessary to facilitate intercultural and international communication.
INCIDENCE AND ETIOLOGY
The overall incidence of deformities that are primarily characterized as metatarsus adductus has been reported at 1 per 1,000 live births. This is about 10 times more frequent than talipes equinovarus (9). Kite (3) was the first to recognize an apparent modern increase in the incidence. Whether this trend is a result of better recognition or other possible causes is unclear. Other potential causes for the increased incidence include a wider distribution of infant care manuals that encourage belly sleeping (in this position, babies often sleep on the feet and effectively splint the lower legs and feet in a position of medial rotation and adduction), increasing birth weight with better prenatal nutrition, broader intervals between sibling births, and older maternal age at birth. A large-number comparison of the incidence of metatarsus adductus in developed countries versus developing countries may help to clarify whether any of these postulated causes has merit.
Many theories on the origin of metatarsus adductus exist. These may be grossly classified as “packaging” defects or “manufacturing” defects (10). It is also conceivable that either mechanism could produce the same clinical appearance. Although the cause is academically interesting, I am unaware of any evidence demonstrating that the prognosis for resolution of an inherited disorder is any worse than that of an acquired defect.
Evidence of intrauterine pressure, or a “packaging” defect, as a cause includes the prevalence of left-sided over right-sided deformity (11). The left leg is more often positioned against the firmer spine than against the abdomen in utero. Ponseti and Becker (12) also noted a higher incidence in first pregnancies, when presumably the womb is less stretched. Preterm and multiple fetus births also have a higher incidence of metatarsus adductus (13).
Wynne-Davies (9) noted an increased appearance of metatarsus adductus in siblings, a finding possibly indicating a genetic or “manufacturing” defect. However, because an inheritance
pattern is not clear, multigenic inheritance with variable penetrance is a possible mechanism. Abnormalities in the mother’s anatomy could also explain higher sibling involvement. A later work by Wynne-Davies et al (14) failed to demonstrate support for this premise.
pattern is not clear, multigenic inheritance with variable penetrance is a possible mechanism. Abnormalities in the mother’s anatomy could also explain higher sibling involvement. A later work by Wynne-Davies et al (14) failed to demonstrate support for this premise.
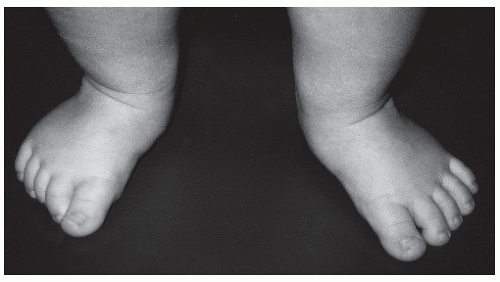
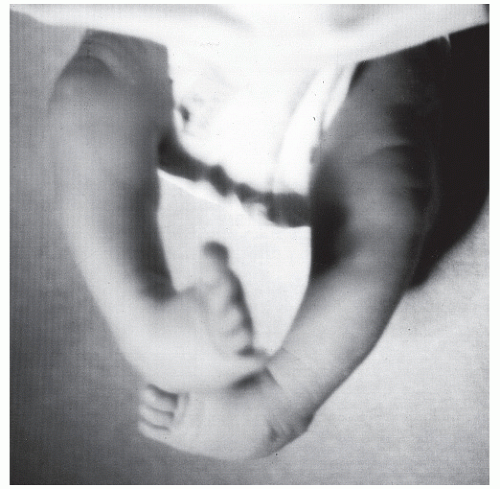 Figure 73.1 Neonate with metatarsus adductus as part of a talipes equinovarus deformity. Note the abnormal rearfoot positioning with rearfoot varus and ankle equinus. |
Absence of the medial cuneiform has been cited as one possible cause of metatarsus varus (15). This cause has not been supported by other studies. However, abnormal growth of the medial cuneiform is a likely cause of persistent metatarsus adductus. This condition has been illustrated in histologic sections (16).
Abnormal muscle positions have also been suggested. Ghali et al (17) reported an exaggerated plantar insertion of the tibialis anterior tendon, although another study was unable to demonstrate this abnormality in cadaveric specimens (18). Browne and Paton (19) suspected contraction of the posterior tibial tendon as a cause of metatarsus adductus. An abnormal insertion of the abductor hallucis has been noted by Sgarlato (20). Thompson and Simons (21) theorized that hyperactivity of the abductor hallucis could produce metatarsus adductus deformity or at least mimic it and resist its correction.
Tax and Albright (22) suspected that an arrest of normal ontologic rotation of the foot resulted in persistent metatarsus adductus. Metatarsus adductus is a normal position of the foot in early fetal development (Fig. 73.4).
Many congenital syndromes include metatarsus adductus as a component. Deformation sequences may also terminate in metatarsus adductus. A higher index of suspicion may lead the foot and ankle physician to suspect a comorbid disease. In infants, the “hard tissue” (bone) is soft cartilage analog, and the “soft tissue” (ligament) is normally strong or hard. The fetus with ligamentous laxity is unable to resist the deforming forces of the primigravida womb, and metatarsus adductus may be induced (23) (Figs. 73.5 and 73.6).
CLINICAL EVALUATION
PRESENTATION
Metatarsus adductus presents as six distinct forms:
Simple metatarsus adductus is characterized by an abnormal forefoot to rearfoot relationship, with the metatarsals abducted on the transverse plane at Lisfranc articulation. Pure adduction occurs on a plane parallel to the ground.
Metatarsus adducto varus is present when the adducted metatarsals have an additional frontal plane varus component. Therefore, the deformity exists on two planes, that is, adduction (transverse) and varus (frontal).
Metatarsus primus adductus exists when only the first metatarsal is adducted and the intermetatarsal angle is greater than 15 degrees.
Complex metatarsus adductus is present when a valgus deformity of the rearfoot coexists. In this instance, the calcaneus, cuboid, and navicular are all rotated laterally beneath the talus. This is referred to as the serpentine foot or Z-foot, in which the navicular is articulating on the lateral side of the talar head. Normally, the talus, navicular, and the first metatarsal form a straight line, but in this foot, a line drawn through the long axis of the talus deviates laterally through the navicular and then deviates medially through the first metatarsal to form a Z. This foot is identified in the neonate with a large increase in the talocalcaneal angle because the navicular shadow cannot be seen on radiograph. Berg further subdivided the complex metatarsus adductus deformity according to pathologic findings in three foot segments: forefoot, midfoot, and hindfoot (8). The first condition, complex metatarsus adductus, is a deformity of the forefoot and midfoot. Its characteristics are (a) an adducted forefoot, (b) lateral translation of the midfoot, and (c) a normal hindfoot. The second category is skewfoot, a deformity of the forefoot and hindfoot, which consists of (a) an adducted forefoot, (b) a normal midfoot, and (c) hindfoot valgus. In the third condition, complex skewfoot, all three components are deformed, resulting in (a) an adducted forefoot, (b) lateral translation of the midfoot, and (c) hindfoot valgus. The key to the lateral translation of the midfoot is that the calcaneal midline intersects the medial one-third of the cuboid. Normally, the cuboid is directly in front of the calcaneus.
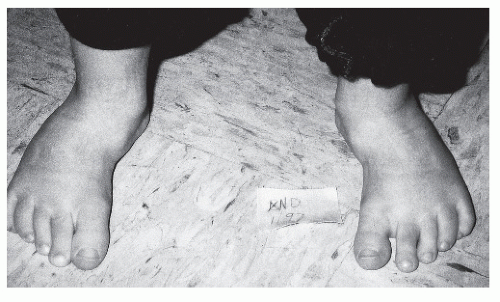
Figure 73.6 Metatarsus adductus and early secondary digital deformities afflict this patient who has Ehlers-Danlos syndrome.
Talipes equinovarus is the classic clubfoot, with adducted metatarsals as one of the three basic components, the other two being rearfoot varus and equinus. Equinus is the key factor that differentiates this condition from metatarsus adductus. Equinus is invariably the more difficult component to correct.
Cavoadducto varus is a deformity in which the metatarsals are adducted and the rearfoot is in varus (7). It differs from the classic clubfoot (no. 5) in that equinus is absent. It differs from metatarsus varus (no. 2) in that the first metatarsal is plantarflexed (frontal plane valgus). This deformity is seldom seen in the infant and usually appears during the early teens, a finding suggesting a possible neurologic cause.
PHYSICAL EXAMINATION
The ARM method of physical examination described by Ganley facilitates immediate appreciation of the metatarsus adductus deformity (24). ARM stands for the components of the pediatric evaluation: attitude, relationship, and movement. The resting “attitude” of the foot in the non-weight-bearing neonate with metatarsus adductus is pointing medially, unless more proximal deformity negates this appearance. Therefore, appreciation of
the “relationship” of the forefoot to the rearfoot in all three cardinal planes is necessary (Fig. 73.7). In all deformities that exhibit metatarsus adductus, the forefoot is adducted toward the body’s midline relative to the rearfoot. Deformity in the hindfoot, leg, knee, thigh, or hip may, however, produce an overall rectus or laterally rotated attitude. “Movement” of the forefoot relative to the rearfoot may be possible in varying amounts. Simply stimulating the primitive reflexes of the lower extremity may spontaneously reduce the deformity in some patients temporarily, whereas firm laterally directed force may not in other patients. Apparent changes may occur rapidly in infancy. Positional abnormalities present at birth may spontaneously resolve as the effect of maternal hormones diminishes. Mild-appearing deformities may become much worse when weight-bearing begins. Thus, even mild flexible deformities must be frequently reexamined, and weight-bearing should at least be simulated at each visit (2,17) (Fig. 73.8).
the “relationship” of the forefoot to the rearfoot in all three cardinal planes is necessary (Fig. 73.7). In all deformities that exhibit metatarsus adductus, the forefoot is adducted toward the body’s midline relative to the rearfoot. Deformity in the hindfoot, leg, knee, thigh, or hip may, however, produce an overall rectus or laterally rotated attitude. “Movement” of the forefoot relative to the rearfoot may be possible in varying amounts. Simply stimulating the primitive reflexes of the lower extremity may spontaneously reduce the deformity in some patients temporarily, whereas firm laterally directed force may not in other patients. Apparent changes may occur rapidly in infancy. Positional abnormalities present at birth may spontaneously resolve as the effect of maternal hormones diminishes. Mild-appearing deformities may become much worse when weight-bearing begins. Thus, even mild flexible deformities must be frequently reexamined, and weight-bearing should at least be simulated at each visit (2,17) (Fig. 73.8).
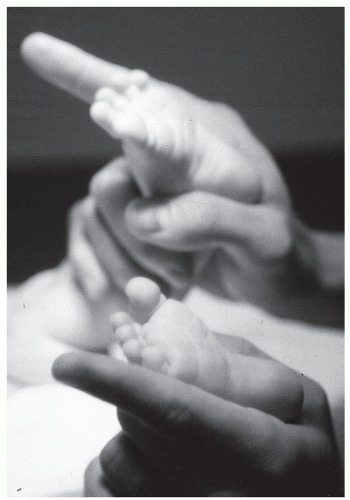 Figure 73.7 Evaluation of the position of an infant’s feet in all three cardinal planes is necessary. Comparison of the lateral border of the foot to a straight edge may highlight deformity. |
Other deformities have been associated with metatarsus adductus (14). Tibial torsion and femoral torsion are frequently observed comorbid conditions with metatarsus adductus (25). Developmental dysplasia of the hip has also been reported as more common with metatarsus adductus; however, this claim has been disputed by Wynn-Davies et al (14). Appropriate physical examination for these conditions should be included in the lower extremity examination of any infant. Suspicious hip movement or sounds should be assessed or referred for appropriate management.
PROGNOSTIC CLASSIFICATION
With the patient supine, the examiner can lift the patient’s foot by the toes. Bestard et al (26) considered the results positive when the deformity persisted in this position. Berg employed a bisection of the plantar heel to estimate the severity of the deformity, but he admitted that his method could not predict outcomes (8).
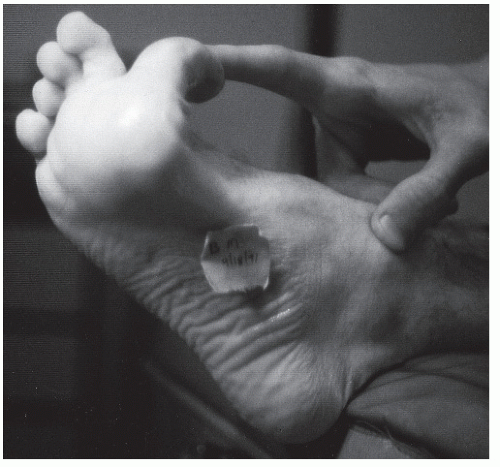
Ganley and Ganley (1) preferred a simple flexibility test, which is reproducible and uncomplicated (Fig. 73.9). If the foot is manually correctable without force, this is considered a mild deformity. If the deformity is only correctable with force, it is classified as moderate. A severe case is not manually reducible. Although this method has been suggested as a good prognostic test for the success of treatment, no published studies have substantiated this claim. In addition, although three levels of severity are described, only two basic treatment protocols are recommended. These are treatment or no treatment. A system that fails to provide treatment guidance is of little use to clinicians.
I am unaware of any system that can correctly predict the outcome of any form of metatarsus adductus. Therefore, I do not rely on any specific tests to predict outcomes.
DIAGNOSTIC IMAGING
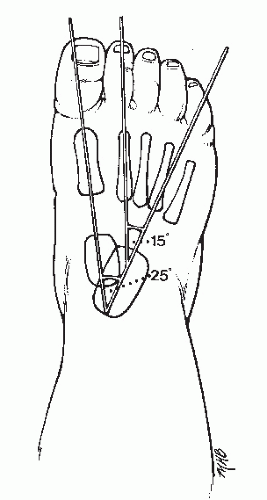
Several roentgenographic methods measuring the amount of metatarsus adductus have been described. Regrettably, most of these methods are useful only in a fully ossified skeleton. This problem was addressed by Ganley and Ganley (1), who used the calcaneus as a reference point. They recognized that the metatarsals are the most obvious component involved and show varying degrees of deformity. The lesser tarsal bones in a neonate, however, are not measurable and are radiographically silent. In many types of metatarsus adductus, the talocalcaneal relationship may be abnormal. These investigators went on to state that it is axiomatic that a variable is best measured against a fixed reference point.
In the clinical examination of the infant, a preferred method is to use the more proximal anatomy as the fixed point against which the distal parts are measured with respect to attitude and
range of motion (24). To be consistent, the examiner should consider a correlative method regarding the radiographic study. The tibia is ideal for recording foot position when it is viewed laterally inasmuch as the foot and leg are on the same plane. However, in the dorsoplantar view of the foot, the leg is at a right angle to the x-ray film, and the tibia becomes less than an ideal reference point. Recognizing this problem, Ganley and Ganley (1) stated that the talus is the foot structure with the most constant and normal relationship with the leg. This is especially true in metatarsus adductus deformity because equinus and dorsiflexion do not enter into the problem. The talus moves on the sagittal plane but is relatively fixed in the other two planes in the ankle mortise. No one has suggested an abnormal talotibial position in metatarsus adductus. Possibly, severe adduction deformity could influence the angle between the talar head and body, but for the most part, the central axis of the talus represents an extension of the leg and is the best starting point to measure metatarsus adductus deformity. Therefore, Ganley and Ganley (1) preferred the talocalcaneal angle of divergence, or Kite angle, as the first recommended measurement to determine the presence of rearfoot abnormality. This angle is normally 20 to 25 degrees. If the talocalcaneal angle is within normal limits, then a rearfoot abnormality can be ruled out, and the talar-first metatarsal angle (i.e., the angle formed by the long axis of the talus and the long axis of the first metatarsal) should determine the degree of metatarsus adductus. Simons showed that in the infant, the talar-first metatarsal angle is normally 0 to -20 degrees (27).
range of motion (24). To be consistent, the examiner should consider a correlative method regarding the radiographic study. The tibia is ideal for recording foot position when it is viewed laterally inasmuch as the foot and leg are on the same plane. However, in the dorsoplantar view of the foot, the leg is at a right angle to the x-ray film, and the tibia becomes less than an ideal reference point. Recognizing this problem, Ganley and Ganley (1) stated that the talus is the foot structure with the most constant and normal relationship with the leg. This is especially true in metatarsus adductus deformity because equinus and dorsiflexion do not enter into the problem. The talus moves on the sagittal plane but is relatively fixed in the other two planes in the ankle mortise. No one has suggested an abnormal talotibial position in metatarsus adductus. Possibly, severe adduction deformity could influence the angle between the talar head and body, but for the most part, the central axis of the talus represents an extension of the leg and is the best starting point to measure metatarsus adductus deformity. Therefore, Ganley and Ganley (1) preferred the talocalcaneal angle of divergence, or Kite angle, as the first recommended measurement to determine the presence of rearfoot abnormality. This angle is normally 20 to 25 degrees. If the talocalcaneal angle is within normal limits, then a rearfoot abnormality can be ruled out, and the talar-first metatarsal angle (i.e., the angle formed by the long axis of the talus and the long axis of the first metatarsal) should determine the degree of metatarsus adductus. Simons showed that in the infant, the talar-first metatarsal angle is normally 0 to -20 degrees (27).
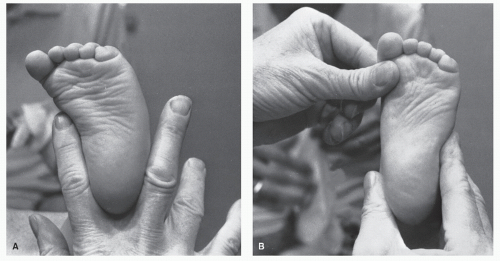 Figure 73.9. Flexibility test. Severity of deformity is tested by attempts at manual correction. In this instance, the foot can be corrected but only with force; thus, the deformity is moderate. |
The calcaneal-second metatarsal angle (i.e., the angle formed between the long axis of the calcaneus and the bisection of the long axis of the second metatarsal) is probably the best method for measuring forefoot adduction (Fig. 73.10). The central axis of the calcaneus is parallel to the lateral border, and because the lateral border of the calcaneus is often easily visualized on a radiograph, the calcaneal-second metatarsal angle is often measured between the lateral border of the calcaneus and the long axis of the second metatarsal. The calcaneal-fifth metatarsal angle is normally 0 degrees (12). The central axis of the calcaneus bisects the fourth metatarsal (28). Ganley and
Ganley (1) found that the normal calcaneal-second metatarsal angle is 15 degrees, ±3 degrees.
Ganley (1) found that the normal calcaneal-second metatarsal angle is 15 degrees, ±3 degrees.
Therefore, dorsoplantar foot radiographs are used to determine the degree of rearfoot abnormality using the talocalcaneal angle. The talar-first metatarsal angle may be useful in this regard, although it is valid only if simple metatarsus adductus exists. A laterally translated cuboid, or an increased calcaneal-cuboid abduction angle, may indicate a midfoot abnormality. The calcaneal-second metatarsal angle (after subtracting 15 degrees) is the most constant determinant of the deformity, according to Ganley and Ganley (1).
Metatarsus adductus does not present any distinguishing characteristics on a lateral radiograph. However, assessment of the forefoot to rearfoot relationships, and the degree of compensation in the rearfoot, can be accomplished. A foot that demonstrates significant subtalar joint pronation has a smaller sinus tarsi and an anteriorly broken cyma line, and the talar bisection falls below the first metatarsal. The calcaneal inclination angle often is also decreased. The lateral talocalcaneal angle is normally between 25 and 45 degrees. In the presence of excess pronation in the rearfoot, this angle may be greater. In the foot with a lack of adequate pronation and showing little rearfoot compensation, the calcaneal inclination angle is increased. One may also see a “bullet-hole” appearance of the sinus tarsi and a posteriorly broken cyma line. The lateral talocalcaneal angle is typically decreased and is less than 25 degrees.
The traditional method used for measuring the deformity has been to compare the lesser tarsus axis with that of the longitudinal axis of the metatarsals (29) (Figs. 73.11 and 73.12). Yu and Dinapoli (30) considered 15 to 20 degrees a mild metatarsus adductus deformity, 21 to 25 degrees a moderate deformity, and greater than 25 degrees a severe deformity (Fig. 73.13). Weissman considered the normal metatarsus adductus angle to be up to 12 to 14 degrees (31). Heatherington and associates considered an angle greater than 14 to 16 degrees to be abnormal (32). The navicular-first metatarsal angle has been used to assess residual forefoot adduction in clubfoot, and this requires that one outline the base of the navicular bone (33). However, this technique is not possible during the first year of life. Engel et al (34) used simple and convenient measurement of the longitudinal axis of the second cuneiform as the alignment of the lesser tarsus (Fig. 73.14). This approach alleviated the often difficult plotting of the medial and lateral points of the lesser tarsus used in the more traditional method. These authors used 571 radiographs to arrive at a normal value of 24 degrees, whereas the value using the traditional method was 21 degrees. This method, however, is also difficult in the infant.
Lepow and others combined the arcs of a circle centered about the base of the first and fifth metatarsals to measure metatarsus adductus (35). The juncture of the arcs forms a central line against which the long axis of the second metatarsal is measured. The problem with this method is that the measurement records the inner relationships of the metatarsals to each other. It is in effect measuring a deformity against itself. It does not relate the more proximal (normal) parts.
Thompson and Simons (21) stated that roentgenograms are not needed to evaluate or track most cases of metatarsus adductus. Accurate measurements may also be difficult to reproduce (36). Radiographs may help to confirm a complex deformity when such is suspected, and this may alter treatment techniques. For example, the manipulation of the calcaneus is entirely different in treating metatarsus cavovarus than it is for simple metatarsus adductus or complex metatarsus adductus. Banks et al (37) showed a significantly increased risk of juvenile hallux abductovalgus when the metatarsus adductus angle was greater than or equal to 14 degrees. This may be another use for roentgenograms in attempting to provide a prognosis.
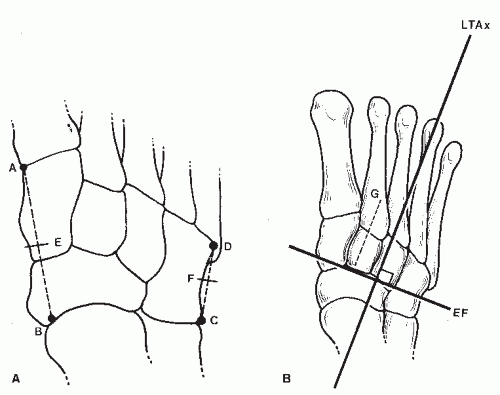 Figure 73.11. A: Diagram demonstrating critical points plotted for determination of longitudinal bisection of lesser tarsus. B: Shows lesser tarsal axis (LTAx), which represents a perpendicular to the bisection of lesser tarsus. Points E and F are midpoints between A and B and C and D, respectively, and line EF is the bisection of the lesser tarsus. Dashed line G represents bisection of the second cuneiform.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|