Fig. 24.1
A size-matched fresh-frozen donor hemi-plateau with meniscus is obtained from a tissue bank in order to fashion a free meniscus graft. (With kind permission from Ref. [107])

Fig. 24.2
Bone plugs measuring 8 mm diameter by 10 mm long are fashioned to recreate the anterior and posterior meniscal root attachment sites to the tibia. (With kind permission from Ref. [107])
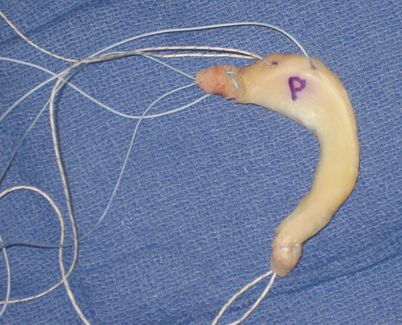
Fig. 24.3
Completed bone-plug meniscal allograft with number 2 permanent sutures passed up central vertical holes in the bone plugs, passed transversely across the root, and back down through the bone plug. Two additional number 2 sutures are placed in the meniscus in the posterior horn and mid-body of the meniscus. (With kind permission from Ref. [107])
After diagnostic arthroscopy, the notch is prepared for cruciate reconstruction. In cases of cruciate intact knees, space is cleared to facilitate posterior bone-plug passage through the notch. For medial meniscal transplants, a small amount of the PCL PM bundle is debrided along with the extreme lateral aspect of the medial femoral condyle (MFC) and the medial eminence (Fig. 24.4). Lateral meniscal transplants require minimal debridement of the ACL PL bundle along with the medial aspect of the LFC and lateral eminence. Once a 9-mm smooth dilator can be easily passed (Fig. 24.5), the preparation is adequate.
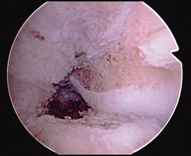
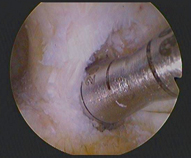
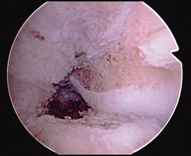
Fig. 24.4
For medial meniscus transplants, a small amount of the PCL posteromedial bundle is debrided along with the extreme lateral aspect of the medial femoral condyle and the medial tibial eminence to facilitate bone-plug passage. PCL posterior cruciate ligament. (With kind permission from Ref. [107])
Fig. 24.5
For lateral meniscus transplants, a minimal recession of the ACL posterolateral bundle and debridement of the medial aspect of the lateral femoral condyle and lateral tibial eminence is performed to facilitate bone-plug passage. Successful passage of a 9-mm tunnel dilator confirms that adequate space exists to pass the posterior bone plug. ACL anterior cruciate ligament. (With kind permission from Ref. [107])
Next, the meniscal remnant is removed. This is performed using a combination of a radiofrequency probe, meniscal scissors, and an arthroscopic biter to cut along the periphery of the meniscus. The goal is to leave a 1–2-mm rim of meniscal tissue while preserving the chondral surfaces (Fig. 24.6). The insertion of the posterior-horn footprint is cleared of soft tissue and marked with the radiofrequency device (Fig. 24.7). An 8-mm posterior-horn bone tunnel or socket is created. While a traditional tunnel can be used, a reverse-drilled socket is preferable to minimize tunnel convergence which may be a concern in a multiple-ligament-injured knee requiring several tunnels. The authors prefer to use an 8-mm FlipCutter (Arthrex, Naples, FL) through a tibial ACL aiming guide to create an 8 x 10 mm socket at the posterior-horn attachment site (Fig. 24.8). A passing suture is placed through this hole out to the anterior portal.

Fig. 24.6
A 1- to 2-mm residual rim of native meniscus is preserved in order to allow secure fixation of the donor meniscus with meniscocapsular suture passage. Extreme care is taken to protect the chondral surfaces during this preparation. (With kind permission from Ref. [107])
Fig. 24.7
The posterior-horn insertion site is cleared of all soft tissue and marked with a radiofrequency device. (With kind permission from Ref. [107])

Fig. 24.8
An 8-mm diameter FlipCutter (Arthrex, Naples, FL) is used to create an 8-mm diameter by 10-mm deep socket in the anatomic posterior-horn footprint using a tibial ACL aiming guide. A passing suture will be placed through this hole and socket for passage of the posterior-horn bone plug. (With kind permission from Ref. [107])
A standard medial or lateral approach for the inside-out meniscal repair technique is then performed. The medial or lateral gastrocnemius fascia is elevated and a retractor is placed to protect the vessel. A second suture is placed 1 cm from the posterior root socket using a suture-shuttling device. This suture is passed through the capsule and out the medial or lateral incision and serves as the shuttling suture for the posterior-horn suture in the meniscus (Fig. 24.9). A third passing suture, the mid-body suture, is placed 1 cm from the last one in a similar fashion. Suture management at this point forward is critical to minimize suture entanglement which interferes with graft passage. The authors prefer to keep the sutures in an ordered fashion with the mid-body suture clamped high on the drape, the posterior-horn suture clamped in the middle, and the posterior root suture clamped low. Again, suture organization is paramount for successful graft passage. At this point, the knee is prepared for meniscus transplantation.


Fig. 24.9
A 90° suture lasso (Arthrex, Naples, FL) is used to place a posterior-horn-passing stitch and a mid-body-passing stitch through the capsule and out the medial or lateral posterior skin incision. After graft passage, the two sutures in the posterior horn and mid-body will be tied to each other over the posterior capsule. (With kind permission from Ref. [107])
With the camera in the anterior portal opposite the compartment being transplanted, an enlarged ipsilateral portal is created to allow the small finger to freely enter into the joint. Prior to graft passage, a ring grasper is used to “run” the passing sutures from outside to inside the joint to confirm that all three sutures exit the enlarged portal without any soft tissue bridges. The graft is then passed into the knee (Fig. 24.10) by first securing the posterior bone plug into its posterior socket. Next, the posterior horn is passed under the femoral condyle by pulling on the posterior-horn and mid-body sutures (Fig. 24.11). Passage of the posterior horn can be assisted by varus or valgus stress to open the transplanted compartment and by a blunt outflow trocar to gently direct the meniscus underneath the condyle. The posterior root bone plug is secured by tying its sutures through a button on the anterior cortex. The posterior-horn and mid-body sutures are tied together over the capsule. At this point, an inside-out meniscal repair is performed working from posterior to anterior (Fig. 24.12). The anterior root bone plug is assessed for where it lays in relation to the anterior tibia. An 8 x 10 mm socket is made through the enlarged portal at this position. A guide pin is drilled from the anterior tibial cortex into this socket, and a bent suture passer is used to pass the anterior bone-plug sutures out the tibial cortex. The bone plug is pulled into its socket and the sutures are tied together through a button on the anterior cortex.
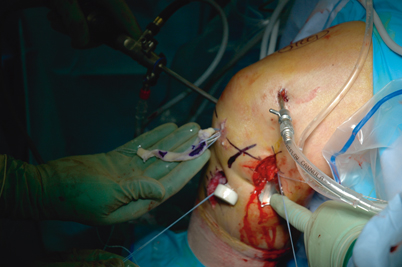

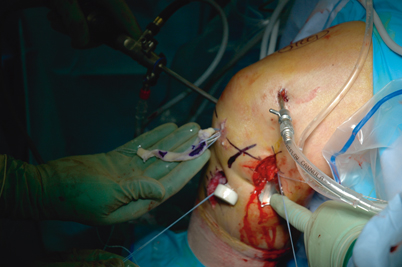
Fig. 24.10
The graft is passed into the knee through the enlarged portal and facilitated by first securing the posterior bone plug into its socket. (With kind permission from Ref. [107])

Fig. 24.11
Sequential traction of the posterior-horn and mid-body sutures is used to pass the meniscus beneath the femoral condyle. This may be assisted with appropriate varus or valgus load on the knee and a blunt outflow trocar. (With kind permission from Ref. [107])
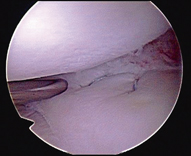
Fig. 24.12
Zone-specific cannulas are used to perform a standard inside-out meniscal repair from posterior to anterior. (With kind permission from Ref. [107])
When performing concomitant PCL reconstruction , the authors prefer to pass the meniscus graft and secure the posterior bone plug, followed by the mid-body repair. Before we secure the anterior bone plug, we typically pass and fix the PCL on the femoral side. After completing our meniscal transplantation, we then secure the PCL on the tibia using the tensioning boot as covered in other chapters.
Rehabilitation after Meniscal Allograft
Rehabilitation after MAT should allow for healing of the meniscus without exceeding the load-to-failure of the meniscocapsular sutures or meniscal-root fixation. Basic science studies have investigated meniscal motion and loading patterns associated with muscle activation through various knee flexion angles. Meniscal motion is significant during knee flexion and extension [62]. Specifically, flexion greater than 90° results in significant meniscal motion and displacement of the posterior horn from the capsule [25, 63]. In contrast, extension reduces the meniscus to the capsule, and there is minimal motion with less than 60° of flexion [62]. Active and passive knee flexion greater than 60°–90° may stress the meniscocapsular and meniscal root fixation during early healing due to the attachments of the semimembranosus to the medial meniscus and the popliteus to the lateral meniscus [64]. However, case series have shown favorable outcomes with early range of motion protocols [65, 66]. Clinical trials comparing different rehabilitation protocols to determine the clinical effect of these biomechanical studies and case series are unavailable. In the absence of high-level evidence for specific rehabilitation protocols, postoperative restrictions are often determined by concomitant cartilage, ligament, or limb realignment procedures [65].
The authors follow a three-phase rehabilitation protocol (Table 24.1). The first phase is a protective phase and extends 6 weeks from surgery. The patient is kept partial weight bearing and wears a brace at all times locked in full extension. The patient passively ranges the knee from full extension to 90° of flexion. The second phase generally extends from weeks 7 through 12 after surgery. This phase focuses on returning full range of motion and achieving a normal gait pattern. The brace is continued but unlocked to allow full range of motion. The patient progresses to full weight-bearing during weeks 7 and 8 and crutches are discontinued when a normal gait pattern is achieved. The third phase goes between 4 and 6 months postoperatively and it is aimed at a return to activity. The brace is discontinued and the focus is on regaining leg strength and a walk to run program. The patient is advised to avoid contact and collision sports for 9 months after surgery at which point they can return to full activities.
Table 24.1
Sample postoperative protocol for isolated meniscal allograft transplantation (Source: With kind permission from Ref. [107])
Phase I: generally 0–6 weeks post-op | |
Phase I goals | ROM: full knee extension, 90° knee flexion |
Precautions | Wear brace at all times |
No bending knee with load applied (i.e., squat, leg press, etc.) | |
Crutches | Begin with touch weight-bearing: progress gradually only when wearing brace locked at 0° |
Weeks 1–2: partial weight-bearing @ 0–25 % body weight | |
Weeks 3–4: partial weight-bearing @ 25–50 % body weight | |
Weeks 5–6: partial weight-bearing @ 50–75 % body weight | |
Brace | Locked at 0° extension for 6 weeks |
Rehabilitation | Begin patellar mobilizations and scar massage after suture removal |
Calf pumping with tubing | |
~ Weeks 1–2 | Heel slides—assisted as needed: within the limits of 0–90° |
Static quad sets, SLRs (in brace) | |
Supine passive extension with towel under heel , Gentle HS stretching | |
~ Weeks 3–4 | Short arc quads—may add light weights as tolerated |
Seated bilateral calf raises—progress to standing bilateral calf raises | |
~ Weeks 5–6 | Hamstring curls—light weight in a painless ROM |
Beginning-level pool exercises: only gait training and deep water jogging | |
Phase II: generally 7–12 weeks post-op | |
Phase II goals | Normal gait and stair ambulation, full knee ROM |
Precautions | Continue to wear brace at all times (except while sleeping), no jogging |
Crutches | Progress gradually to full weight-bearing during weeks 7–8 post-op |
Brace | Open to full ROM |
Rehabilitation | |
7–8 weeks | Stationary bike, gait training, progressive strengthening |
9–10 weeks | Standing balance exercises, progressive strengthening |
11–12 weeks | Along with stationary bike, gradually add elliptical for conditioning |
Phase III: generally 4–6 months post-op | |
Phase III goals | Jog at own pace and distance, ≥ 90 % quadriceps and hamstring strength, ≥ 90 % hop for distance compared to the uninvolved side |
Precautions | No participation in contact/collision sports or military schools |
Brace | None required |
Rehabilitation | |
13–16 weeks | Progressive functional training, strengthening, and balance training |
17–26 weeks | Progressive jogging program |
Miscellaneous | No return to contact/collision sports or military schools until 9 months |
After 6 months post-op: exercises in phase III are continued, gradually increasing intensity and duration as tolerated with the goal of full return to activity @ ~ 9 months post-op | |
Meniscal allografts have a limited life span with deteriorating outcomes over time despite revascularization of the tissue [67, 68]. As a result, the authors do not recommend a return to high-demand activities that involve cutting, pivoting, jumping, or carrying heavy loads. While greater than 60 % of meniscal allograft patients return to some level of sporting activities, the goal of MAT should be a painless knee during activities of daily living [15, 69].
Outcomes
MAT is successful in reducing pain, decreasing effusions, and improving knee function. These clinical improvements are likely due to the improved load transmission characteristics of the meniscal allograft compared to the meniscectomized knee [70]. However, despite improvements in biomechanical function, there is little evidence that MAT slows the progression of cartilage degeneration. Therefore, the goals of this procedure should be to reduce pain, decrease swelling, and improve knee function in the short term while performing activities of daily living.
Despite a high incidence of meniscal injuries after PCL -based knee injuries, very few studies have reported outcomes on MATs with PCL-based knee reconstructions [71]. The literature on PCL-based knee injuries treated with reconstruction and meniscal allograft are limited to individual case reports [50, 60].
The natural history of the meniscectomized knee is consistent cartilage degradation and development of osteoarthritis [1]. Compared to a stable meniscectomized knee, a knee that sustains trauma resulting in PCL injury presumably has cartilage damage and altered mechanics that may hasten the development of arthritis. The goals of MAT in this setting is to provide the meniscectomized knee with tissue that reproduces the improved contact mechanics, reduced peak contact pressures, stabilizing, and chondroprotective effects of the meniscus intact knee.
Prevention of Osteoarthritis
Multiple animal and cadaveric models have evaluated the chondroprotective effects of meniscal allograft transplants. Pressure-sensitive film has been used to evaluate tibiofemoral contact pressures after meniscectomy compared to allograft transplantation in cadaveric models. In lateral meniscal allograft transplants, peak local contact pressures decrease 55–65 % compared to meniscectomy, but contact pressures remain higher than the intact state [70]. After medial meniscal transplantation, maximum and mean contact pressures are reduced 75 % and this contact pressure reduction is closely related to the accuracy of size-matched graft tissue [56]. Peak pressures are restored to near normal after lateral allograft transplantation and bone-plug fixation was found to be superior compared to suture fixation alone [72]. These cadaveric models suggest a chondroprotective effect of MAT through reduction in contact pressures.
A sheep model was utilized by Szomor et al. to evaluate in vivo chondroprotective effects of meniscal transplantation [73]. The area of damaged articular cartilage was reduced by 50 % with meniscal allograft or autograft compared to meniscectomized animals 4 months after surgery. Similarly, Kelly et al. used a sheep model to compare meniscectomized animals with lateral MAT [74]. The cartilage was evaluated at 2, 4, and 12 months with gross inspection, magnetic resonance imaging, T2 mapping, biomechanical testing, and histologic analysis. Significant chondroprotective effects of meniscal allograft transplant were found compared to meniscectomy, but there was still more cartilage damage in the meniscus transplant group compared to the meniscal intact control group. The authors concluded that meniscal allografts provide significant, but incomplete, protection from cartilage degradation in short-term follow-up after meniscectomy.
Rijk et al. utilized a rabbit model to compare radiographic and cartilage cellular activity changes 1 year after meniscectomy or meniscal allograft transplant [75]. No differences in these parameters were found between the meniscectomized animals and the meniscal allograft transplanted animals with the conclusion that transplantation does not prevent degenerative changes with longer follow-up in this rabbit knee model [75, 76].
The chondroprotective effects of meniscal allografts in human subjects have been described only in case series. Ha et al. noted no progression in arthrosis grade in 77.8 % of knees evaluated with magnetic resonance imaging or 64 % of second-look arthroscopies evaluated at relatively short-term follow-up of 31 months [77]. Verdonk et al. reported that 41 % of knees with fresh-meniscal allograft transplants had no further decrease in tibiofemoral joint space width at a minimum of 10 years postoperatively [78]. The authors concluded that the operation had a potentially chondroprotective effect based on the absence of additional joint space narrowing. While this study is compelling by its longer-term follow-up, a randomized trial or prospective comparison to a meniscectomy control group is necessary to define the clinically relevant chondroprotective effects of meniscal allografts compared to meniscectomy.
Healing of Meniscal Allograft
Animal studies have reported healing of meniscal allografts with host cellular repopulation in peripheral meniscal tissue. Fibrovascular scar tissue has been shown in a dog model to be the mechanism of healing to the capsular tissues for cryopreserved menisci [79]. A normal cellular distribution was found, but the allograft cells had a decrease in the number of metabolically active cells. Fresh and cryopreserved menisci showed peripheral healing and revascularization in a goat model, but biochemical changes were noted in the extracellular matrix at 6 months after transplantation [80].
During healing, a transplanted meniscus is revascularized and repopulated with host cells. DNA-probe analysis in a goat model revealed that cells from the meniscus did not survive transplantation, and host cellular DNA was identified completely by 4 weeks [81]. DNA analysis of meniscal allograft tissue retrieved 1 year after transplantation confirmed host repopulation in a patient [46]. Cells derived from the synovial membrane with characteristics similar to synovial cells and fibroblasts repopulate the meniscus in meniscal allograft biopsies 16 months after implantation [82]. The authors in this study also noted cells indicative of an immune response directed at the meniscal allograft, but it did not affect the clinical outcome.
Clinical Outcomes
The clinical evidence for the success of MAT is derived from case series. Comparisons between studies are difficult due to a lack of uniformity on surgical technique, sterilization and preservation methods, outcome measures reported, and patient selection. Furthermore, important characteristics that may affect outcome are not uniformly described including method of size matching, concomitant chondral and ligamentous injury, and limb alignment. With these limitations of clinical outcome comparisons after meniscal transplantation noted, a recent systematic review reported patient satisfaction ranges from 62.5 to 100 % and early failure rates range from 7 to 35 % [15, 83–85]. The early failure rate averaged 10 % when excluding older patients with preexisting osteoarthritis [15].
Milachowski first reported MAT in 1989 and reported an 86 % success rate with 22 meniscal allografts at 14 months after surgery [3]. Noyes et al. reported on 96 fresh-frozen, gamma-irradiated meniscal allografts and noted a 58 % failure rate which has been largely attributed to the gamma-irradiation [38]. Lyophilized meniscus transplants have also had inferior outcomes similar to a meniscectomy control group [68].
Recent series with improved sterilization and preservation methods have shown improved outcomes. A prospective case series of 40 meniscal allografts with anterior and posterior bone-plug fixation had an 86 % success rate and International Knee Documentation Committee (IKDC) scores in the normal or near normal range at 2 years [84]. Cryopreservation was the most common type of graft preparation. Another case series of 40 patients treated with frozen, nonirradiated meniscal allografts implanted with a bone-plug technique, IKDC and Modified Cincinnati scores improved significantly after surgery with reductions in pain, decreased effusions, and improved function [86].
Long-Term Follow-Up
While early results of allograft transplantation have been successful with objective and patient-reported outcome measures, long-term results remain the most important. Van der Wal evaluated 63 cryopreserved meniscal allografts with soft tissue fixation alone at 13.8 years after surgery [67]. A 29 % failure rate and deterioration in patient outcomes over time was noted. Lysholm scores of 79 at 3 years after surgery significantly declined to 61 at final follow-up. There was no difference in Lysholm scores between allograft survivors and those that failed requiring a knee arthroplasty. Wirth et al. reported a decline in Lysholm scores from 84 at 3 years to 75 at 14 years follow-up [68]. A 55 % failure rate at 11.8 years in a recent case series of 22 cryopreserved meniscal allografts was noted. The authors noted improvements in pain and function with only fair results at longer-term follow-up [87]. In contrast to this, a series of 50 cryopreserved meniscal allografts implanted with soft-tissue-only fixation had a 10 % failure rate [88].
Medial Versus Lateral
Outcomes of medial versus lateral MAT have been different in several series [78, 87, 89, 90]. In one study, lateral meniscal allografts had a 76.5 % survival rate at 10 years while medial allografts had a 50.6 % survival rate at 9 years [89]. In contrast, another series had a 25 % medial allograft failure rate compared to a 50 % lateral failure rate at 11.8 years after surgery [87]. Several authors found no significant differences in outcomes between medial and lateral meniscal allografts [66, 91, 92]. The disparity in outcomes may potentially be attributed to differences in ligamentous stability or mechanical alignment. A recent systematic review of MAT found no difference in outcomes between medial and lateral allograft transplants [93].
Preexisting Osteoarthritis
Preexisting knee osteoarthritis portends a worse prognosis after MAT. An 80 % failure rate was noted in knees with advanced arthrosis compared to 6 % in patients with normal articular cartilage or mild arthrosis in an early study of MAT [38, 94]. Improved postoperative Lysholm and Tegner scores in patients with Outerbridge scores of less than 2 have been noted, while patients with Outerbridge scores greater than 3 in any area did not improve with surgery [66]. Evaluation of 29 meniscal allografts using magnetic resonance imaging revealed allograft degeneration was associated with moderate and severe chondral wear and the authors recommended preoperative assessment to identify patients at risk for failure [95].
Defining the optimal time to offer MAT remains difficult. Total meniscectomy results in long-term degradation of articular cartilage [1]. While only limited data are available to support MAT to prevent or slow progression of osteoarthritis, it is currently the only surgical option for young patients with a symptomatic meniscus-deficient knee. Prophylactic meniscal allografts before the onset of symptoms in an attempt to prevent degenerative changes have been reported [96]. Without clinical studies proving chondroprotective benefits, meniscal allografts are not currently recommended for asymptomatic meniscus-deficient patients. Waiting for a patient to develop cartilage degeneration and symptoms may reduce graft survival and symptomatic relief. Given this difficult clinical situation, we recommend yearly follow-up for young patients with meniscus-deficient knees with weight-bearing radiographs to monitor progression of symptoms and joint space narrowing. Future surrogate markers of cartilage degradation (i.e., imaging or biomarkers) may enable earlier detection to help define the appropriate indications for MAT. Little evidence exists supporting the routine use of MRI or bone scanning in such patients and the cost over time obtaining such studies may be prohibitive.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








