Chapter 28 Meniscus Tears
Diagnosis, Repair Techniques, and Clinical Outcomes
INDICATIONS
The importance of the menisci in the human knee is well understood and documented. The menisci occupy 60% of the contact area between the tibial and the femoral cartilage surfaces and transmit greater than 50% of joint compression forces. After meniscectomy, the tibiofemoral contact area decreases by approximately 50% and the contact forces increase two- to threefold.2,45,66,71,83,139 Meniscectomy frequently leads to irreparable joint damage, including articular cartilage degeneration, flattening of articular surfaces, and subchondral bone sclerosis. Poor long-term clinical results have been reported by many investigators after partial and total meniscectomy.* For instance, Scheller and coworkers122 followed 75 knees that underwent partial lateral meniscectomy 5 to 15 years postoperatively and noted that 78% had Fairbank’s signs of radiographic deterioration. Rockborn and Messner114 noted a 50% rate of radiographic osteoarthritis in 30 patients who underwent meniscectomy a mean of 13 years postoperatively. Roos and associates119 followed 82 knees that underwent medial meniscectomy and 25 knees that underwent lateral meniscectomy a mean of 21 years postoperatively and reported that nearly one half had advanced radiographic osteoarthritis compared with a control group. These authors reported that the relative risk of developing osteoarthritis was 3.6 after partial meniscectomy and 7.1 after total meniscectomy. Problems do exist in many meniscectomy natural history studies such as including both partial and total meniscectomy in the same cohort; not assessing the effects of patient body weight, activity level, and overall lower limb alignment on the functional result; failure to include weight-bearing posteroanterior (PA) radiographs in the assessment; and lack of a carefully defined control group for comparison. Still, preservation of meniscal tissue and function remains paramount for long-term joint function.
Candidates for meniscal repair are active patients younger than 60 years of age. Trauma is one of the most common etiologies of meniscus tears. For example, meniscus tears occur in 40% to 60% of patients with anterior cruciate ligament (ACL) ruptures.76,98 The majority of these tears extend into the middle third avascular region and are amendable to a meticulous inside-out suture repair. Magnetic resonance imaging (MRI) provides important information regarding the type of meniscus tear and potential for repair to preserve function.44 In knees in which repair is deemed possible, it is important to restrict strenuous activities and athletics until surgery to avoid further damage to the joint and meniscus.
Complications and deteriorating results have been reported by others after the use of all-inside meniscus fixation devices72,74,78,87,125,136 which have reduced failure, stiffness, and displacement properties compared with vertical sutures.25,110 The lack of prospective, randomized level I clinical studies precludes definitive recommendations for the various devices currently available.42,78 Therefore, this chapter focuses on suture repair techniques for various types of meniscus tears.
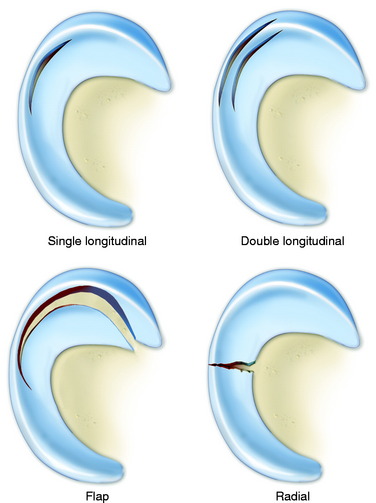
Meniscus tears are classified according to location, type of tear, and integrity and damage to meniscal tissue and the meniscus attachment sites.123 This classification, along with meticulous arthroscopic inspection of the tear site, allows the surgeon to determine whether a tear is reparable. The meniscus body is divided into thirds: inner, middle, and outer. Tears located at the peripheral attachment sites (meniscofemoral and meniscotibial) are referred to as outer third tears. Single longitudinal tears are usually located in the outer third region or at the peripheral attachments (Fig. 28-1). These tears are classified as red-red because both portions have an internal blood supply and are repaired in all cases with high success rates expected.
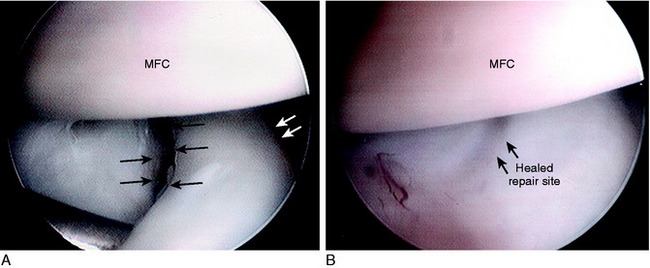
Repairs of complex tears and tears that extend into the middle third region are evaluated on an individual basis. Tear patterns in this region include single longitudinal, double longitudinal, triple longitudinal, horizontal, radial, and flap. The rationale for repair of these tears is that removal results in essentially a total meniscectomy because a substantial amount of meniscal tissue is resected (Fig. 28-2). This is especially concerning in younger patients in their 2nd to 4th decades of life and in all athletically active individuals. These tears are often reparable with reasonable success rates, as described later in this chapter.
CONTRAINDICATIONS
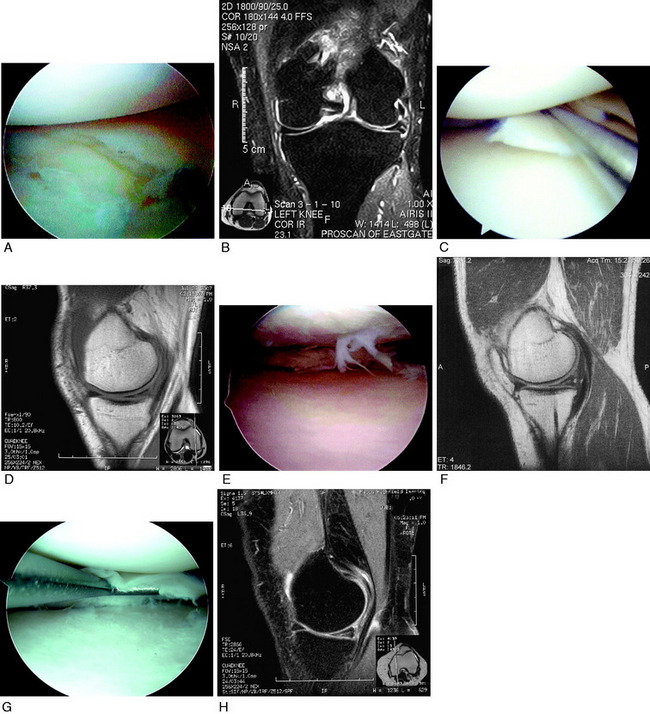
Meniscus tears located in the inner third region are not reparable and require débridement. Chronic degenerative tears usually have tear components in multiple planes and are classified as complex. The surgeon must carefully assess the tear pattern and determine the amount and integrity of meniscal tissue that is present. Many of these tears are not reparable (Fig. 28-3). A large flap tear may be reduced and approximated, and if the tissue has adequate integrity, repair is considered in active patients. Chronic degenerative tears in which poor tissue quality is encountered require débridement. The tissue may be thickened or abnormally firm and altered in shape or length. Horizontal tears frequently involve displacement of the meniscus from the joint such that a repair of the horizontal flaps would not result in restoration of meniscus function.
CLINICAL BIOMECHANICS
Meniscus Function
Critical Points CLINICAL BIOMECHANICS
Under static-loading conditions, the menisci assume a significant load-bearing function in the tibiofemoral articulation.2,26,45 At least 50% of the compressive load of the knee joint is transmitted through the menisci in 0° of extension, and approximately 85% of the load is transmitted at 90° of flexion.2 The presence of the menisci increases the contact area to 2.5 times the size of a meniscectomized joint. The larger contact area provided by the menisci reduces the average contact stress (force/unit area) acting between the joint surfaces. Removal of as little as 15% to 34% of a meniscus increases contact pressures by more than 350%.124
Lee and colleagues75 evaluated the biomechanical effects of serial meniscectomies in the posterior segment of the medial meniscus. Compared with the intact state, the medial contact area decreased from 20% (after removal of 50% of the posterior segment of the medial meniscus) to 54% (total meniscectomy). Medial contact stress increased from 24% (50% meniscectomy) to 134% (total meniscectomy). Medial peak contact stress increased from 43% (50% meniscectomy) to 136% (total meniscectomy). The peripheral portion of the medial meniscus provides a greater contribution to increasing contact area and decreasing contact stresses than the central portion. Peak contact stresses increase proportionally with the amount of meniscus removed.
Medial meniscectomy performed after sectioning of the ACL results in increased anterior translation at 20° of knee flexion compared with that measured in knees with an intact ACL.77 Thus, the loss of the medial meniscus after an ACL rupture is problematic, especially in varus-angulated knees. In knees with posterior cruciate ligament (PCL) ruptures, the increase in posterior tibial translation allows a change in tibiofemoral contact in which the menisci posterior horns have a reduced weight-bearing function. This is sometimes referred to as a “PCL meniscectomy.” The effect is greater for the medial compartment in which the middle and anterior thirds of the medial meniscus have less weight-bearing function than the lateral meniscus.
The menisci remain in constant congruity to the tibial and femoral articular surfaces throughout knee flexion and extension135,146 and are thus believed to contribute to stability to the knee joint.92 The lateral meniscus provides concavity to the lateral tibiofemoral joint owing to the normal posterior convexity of the lateral tibial condyle, allowing the stabilizing effect of joint weight-bearing forces to reduce lateral compartment anterior and posterior translations.82 Total lateral meniscectomy results in a 45% to 50% decrease in total contact area and a 235% to 335% increase in peak local contact pressure.103
Loss of the medial meniscus results in a smaller, more medial displacement of the center of pressure. Load is subsequently transmitted through the articular cartilage and subchondral bone to the underlying cancellous bone through this more central route, thus stress-shielding the proximal aspects of the medial tibial cortex. The deleterious effects of meniscectomy on tibiofemoral compartment articular cartilage have been demonstrated in multiple experimental studies.65,104,132,145 For these reasons, it is paramount to preserve meniscal function, if possible, in knees with varus osseous malalignment.
In addition, the menisci provide shock absorption to the knee joint during walking and are theorized to assist in overall lubrication of the articular surfaces.92,141
Meniscus Suture Repair Biomechanics
Various suture repair techniques and suture materials have been tested experimentally to determine initial fixation strength and performance under cyclical loading.13,106 Suture techniques have also been compared with several meniscus repair devices.* Post and coworkers106 compared the pull-out strength of vertical mattress, horizontal, and knot-end sutures in a porcine model using either 2-0 Ethibond, 0-polydioxanone sutures (PDS), or 1-PDS suture material. The vertical mattress technique with 1-PDS suture had significantly greater (P < .05) mean load-to-failure values than any other combination (146 ± 17 N). This was followed by the vertical mattress technique with 0-PDS suture material (116 ± 28 N). The vertical mattress technique had significantly greater mean load-to-failure values than the horizontal mattress technique, regardless of suture type (P < .0001). There was no difference in the relative strength between horizontal and knot-end suture techniques.
Asik and coworkers13 compared the failure strengths of vertical, vertical mattress, vertical loop, horizontal mattress, and knot-end suture techniques in a bovine model. Each group consisted of four medial menisci, and 1-Prolene suture material was used in all specimens. The vertically oriented sutures showed significantly higher initial fixation strengths (mean, ∼131 N) compared with the knot-end (64 N; P < .001) and horizontal (98 N; P < .001) techniques. In another study, Asik and Sener12 compared the mean load to failure of a variety of meniscus repair devices with that of horizontal and vertically oriented sutures in a bovine model. The strongest repair method was the vertical sutures with 0 PDS (mean, 104.7 N). The mean failure strengths of all of the devices were lower than both suturing techniques (range, 9.8 N for the Arthrex dart to 51.4 N for the T-Fix device).
Miller and associates88 assessed healing rates and chondral injuries of three all-inside devices in a goat model 6 months after implantation. A 15-mm longitudinal tear was created in the peripheral 25% of the posterior-central horn and then repaired with either two Meniscal Fasteners (Mitek, Ethicon, Westwood, MA), two 10-mm BioStingers (Linvatec, Largo, FL), or two 10-mm Clearfix Meniscal Screws (Mitek). A group of goats that had undergone repair with two vertical mattress sutures for a similar lesion was used for control.89 The authors reported that the suture group had a significantly higher rate of healing (93% completely healed, 7% no healing) than all three of the device groups (P < .01), which ranged from 43% to 54% complete healing and from 0% to 25% no healing. In addition, significant chondral injury was observed in the majority of animals in all three device groups.
Several investigations compared the biomechanical properties of meniscus arrows with those of vertical and horizontal sutures.4,12,16,24,37,110,126,143 Vertical sutures are superior to both horizontal sutures and meniscus arrows in mean load-to-failure values.12,42,143 Dervin and colleagues37 reported that the meniscus arrow had approximately one half the failure strength of vertical sutures (30 N and 58 N, respectively; P < .001). Song and Lee126 found that the maximum tensile strength of the meniscus arrows was significantly lower (38 N) than both vertical (114 N) and horizontal (75 N) sutures (P < .05). Walsh and coworkers143 reported that the meniscus arrow and meniscus staple had significantly lower mean force-at-failure values (44.3 N and 17.8 N, respectively) than vertical suture (73.9 N; P < .005).
Rankin and associates110 used a bovine model to compare vertical sutures, horizontal sutures, meniscus arrows, and T-Fix repairs in which three sutures or devices were used for each repair. Vertical sutures were stronger than all other repair methods and showed the smallest average residual displacement (0.21 mm). The force required to generate 2 mm of tear displacement was greatest for the vertical sutures and least for the arrow (143 N and 43.6 N, respectively; P < .0001). The superior strength of vertical sutures is believed to be due to the perpendicular orientation to the circumferential collagen bundles of the meniscus.110
Becker and colleagues21 compared the biomechanical behavior of several biodegradable implants for meniscus repair with that of vertical and horizontal mattress sutures in response to cyclical loading and load-to-failure testing. Seventy lateral menisci were removed from patients aged 52 to 60 years prior to total knee replacement. One suture or device was used for each repair. The pull-out strength of the vertical and horizontal sutures was superior to those of the implants. Superior stiffness during load-to-failure testing and lower displacement under cyclical loading were found for the vertical sutures compared with horizontal sutures and all implants.
Nyland and associates100 evaluated displacement (repair site gapping) of all-inside vertically or horizontally placed FasT-Fix (Smith & Nephew, Endoscopy Division, Andover, MA) devices to horizontally placed RapidLoc devices (Mitek Surgical Products, Westwood, MA) under cyclical loading conditions in human cadavers (mean age, 65 ± 7.7 yr). Two implants placed 5 mm apart were used for each repair. The vertical FasT-Fix group had significantly less displacement after 500 cycles than the other two groups (P < .01) and greater stiffness.
Meniscus Repair Healing
There are few published experimental studies on the strength of a healing meniscus suture repair (without cell-based therapy or growth factors) subjected to tensile loads. Newman and associates94 measured the mechanical behavior of canine joints after repair of peripheral and radial meniscus tears. Contralateral limbs served as controls. The peripheral tears were repaired with four vertically oriented sutures, and the radial tears were repaired with two horizontally oriented sutures. Thirteen weeks later, the peripheral repairs demonstrated no statistically significant differences between the repaired and the control limb in compressive force-displacement behavior, input energy, and ratio of dissipated to input energy. All of the peripheral repairs healed, with no gapping at the repair site. However, the radial repairs showed significant differences in the structural and material properties compared with the control limb. These repairs healed with 3- to 5-mm-wide fibrovascular scars, and 10 of 17 (59%) specimens failed to refill the gap completely to the inner meniscal rim. The authors concluded that the mechanical function was restored after peripheral repairs, but not after radial repairs in this animal model.
In a rabbit model, Roeddecker and colleagues117 studied tissue strength after repair of longitudinal meniscal lesions located in the central third region. A 3-mm lesion was created and then either left alone, repaired using one suture, or repaired with a fibrin sealant. The contralateral limb was used as a control. After 6 weeks, the mean relative strength of the healing tissues were 26% (suture) and 42.5% (fibrin glue) of the control values. These strength values remained similar after 13 weeks.
CLINICAL EVALUATION
The presence of tibiofemoral joint line pain on joint palpation is a primary indicator of a meniscus tear. Other clinical signs include pain on forced flexion, obvious meniscal displacement during joint compression and flexion and extension, lack of full extension, and a positive McMurray test.84 All ligament stability tests are performed and compared with the opposite knee joint. MRI may be obtained using a proton-density–weighted, high-resolution, fast-spin-echo sequence107,108 to determine the status of the articular cartilage and menisci. This evaluation is useful in knees with suspected degenerative tears142 and chronic ACL ruptures and to determine whether a meniscus cyst is present. A recent investigation that examined the ability of MRI to predict reparability of longitudinal full-thickness meniscus lesions reported high sensitivity and specificity rates (overall, 94% and 81%, respectively).95
LaPrade and Konowalchuk73 described a figure-four test that attempts to replicate symptoms in patients with tears of the lateral meniscus popliteomeniscal attachments. The patient is placed supine, the knee flexed to approximately 90°, the foot placed over the contralateral knee, and the hip externally rotated. A varus loading at the knee joint increases tensile loading in the damaged posterolateral soft tissue meniscal attachments. The primary symptom from popliteomeniscal tears is lateral compartment pain with activities, especially turning and twisting with sports. MRI is frequently negative. The authors described an open approach to repair the popliteomeniscal attachments. However, these peripheral tears are amendable to an inside-out repair technique, as is described later.
Radiographs taken during the initial examination include lateral at 30° of knee flexion, weight-bearing PA at 45° of knee flexion, and patellofemoral axial. Axial lower limb alignment is measured using full standing hip-knee-ankle weight-bearing radiographs in knees that demonstrate varus or valgus alignment.38 Knees that have deficiency of the posterolateral structures may require lateral stress radiographs. Posterior stress radiographs may be used in patients with PCL ruptures.
Patients complete questionnaires and are interviewed to rate symptoms, functional limitations, sports and occupational activity levels, and patient perception of the overall knee condition according to the Cincinnati Knee Rating System.19
INTRAOPERATIVE EVALUATION
A thorough arthroscopic examination is conducted, documenting articular cartilage surface abnormalities.99 A probe inserted from the medial infrapatellar portal is used to tension the meniscus to determine the integrity of the peripheral rim and the anterior and posterior attachments. The probe is placed underneath the meniscus to visualize the entire undersurface (see Fig. 28-2). Flap tears that otherwise may not be evident may be discovered during this examination.
A 30° or 70° arthroscope is used in the anteromedial portal to examine the posteromedial meniscal region. The anteromedial portal is purposely placed immediately adjacent to the medial border of the patellar tendon. The arthroscope sheath with a blunt obturator is passed along the lateral aspect of the medial femoral condyle distal to the PCL attachment into the posteromedial compartment. The meniscal-synovial junction, the peripheral edge of the meniscus, the opening of a synovial cyst, and the posterior articular surface of the medial femoral condyle are inspected. A nerve hook is passed from the anteromedial portal and brought over the top of the meniscus into the posteromedial compartment. The peripheral attachment of the posterior horn of the medial meniscus frequently cannot be completely visualized unless this view is obtained.27
Critical Points PREOPERATIVE PLANNING
Critical Points INTRAOPERATIVE EVALUATION
The arthroscopic examination in patients with lateral and posterolateral joint pain may not reveal obvious tears of the posterosuperior meniscus attachments. There may be observable tears in the inferior meniscus tissues about the popliteal hiatus and meniscotibial attachments (Fig. 28-4). There is frequently enlargement of the popliteal hiatus and subtle interstitial tearing of the meniscotibial posterior horn attachments that allow the posterior horn to be abnormally elevated and displaced anteriorly into the lateral compartment. These displacement tests of the posterior horn are performed at 60° to 70° of flexion using a figure-four position because the increased joint gap allows a nerve hook to easily displace the posterior horn and demonstrate the abnormal slackness of the attachments. The authors have frequently encountered athletes who have had a prior negative arthroscopic examination and MRI who have demonstrable posterior horn popliteomeniscal attachment tears that require suture repair.
OPERATIVE TECHNIQUE
Patient Preparation
The patient is placed in the supine position on the operating table so that the affected leg is elevated (Fig. 28-5). The foot of the surgical bed is adjusted to allow 90° of knee flexion. A tourniquet and leg holder are used, but the tourniquet is inflated only for the initial exposure. The leg holder is placed at the middle of the thigh, which allows an assistant to open the tibiofemoral compartment under maximum tension for visualization and meniscus surgery. The extremity is draped free to allow easy positioning during surgery. Standard medial and lateral patellar arthroscopic portals, placed directly adjacent to the patellar tendon, are used for the diagnostic arthroscopy. A common mistake is to place the arthroscopic portals too far medially or laterally over the femoral condyles, where instrument passage damages the femoral articular cartilage. The safe area for instrument passage is with the portal just medial and lateral to the patellar tendon with passage into the femoral notch region.
Critical Points OPERATIVE TECHNIQUE
Exposure for Medial Meniscus Repair
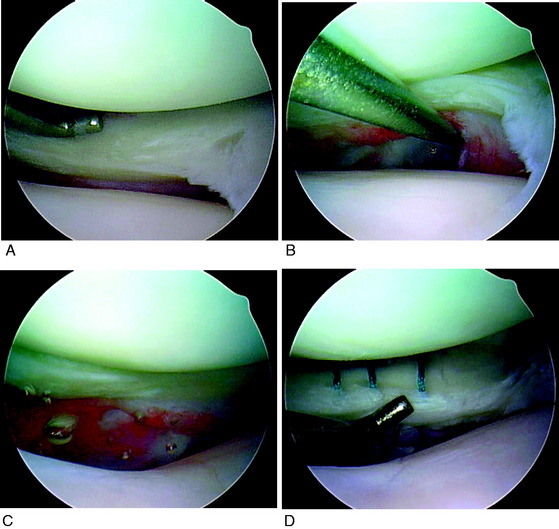
Medial Meniscus Suture Repair Techniques
Multiple 2-0 Braided Polyester Nonabsorbable Sutures Used on 10-Inch Straight Cutting Needle
Exposure for Medial Meniscus Repair
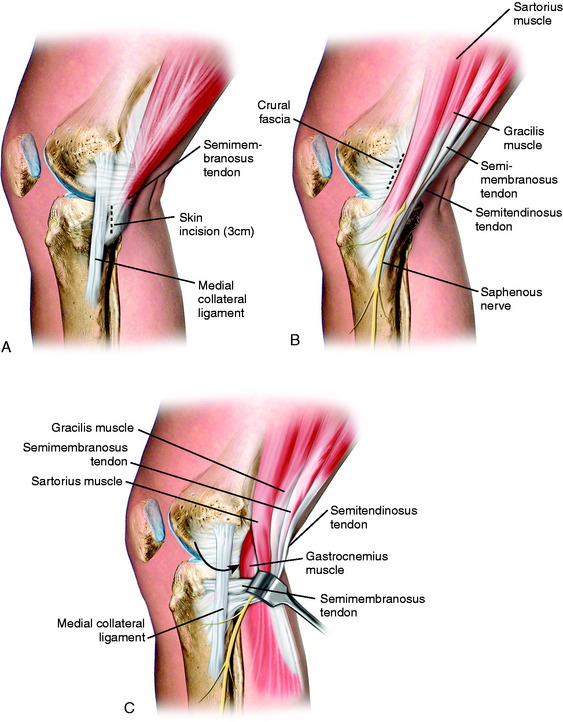
With the surgeon seated, using a headlight, and the sterile prepared foot in the surgeon’s lap, the knee is flexed to 60° and a 3-cm vertical skin incision is made just posterior to the superficial medial collateral ligament (SMCL; Fig. 28-6). The tourniquet is inflated for the surgical exposure. The incision is centered just below the joint line (one third above, two thirds below) to allow retrieval of sutures. Avoid placing the incision too posterior in order to protect the saphenous vein and nerve. The subcutaneous dissection proceeds from the superior aspect of the wound down to the fascia. Care must be taken in the inferior aspect of the wound to avoid damage to the saphenous vein and nerve. Two retractors are used to provide visualization of the next layer of structures, the crural fascia and sartorius.
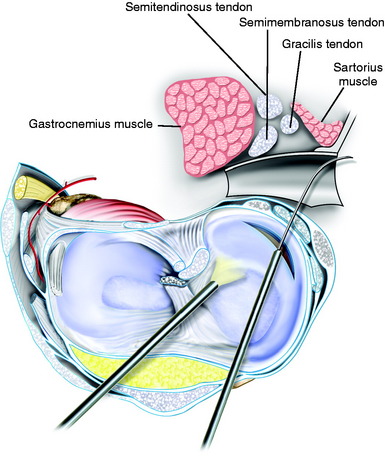
Blunt dissection with an index finger allows development of a plane between the medial gastrocnemius tendon and the posterior capsule. A Henning retractor or spoon is inserted, allowing safe suture placement and needle retrieval (Fig. 28-7). The anesthesiologist is asked to provide muscle relaxation so that the gastrocnemius and semimembranosus muscles can be retracted. If the exposure is inadequate at this point, an alternative approach is to further dissect the semimembranosus tendon, which is elevated proximally to gain exposure just distal to the tendon. This is a less ideal approach because it is necessary to avoid placing sutures through the semimembranosus tendon just above its tibial attachment site.
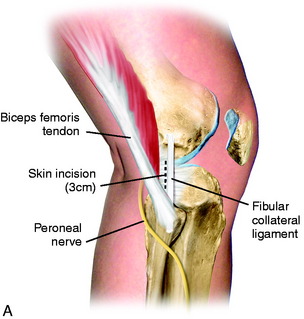
Exposure for Lateral Meniscus Repair
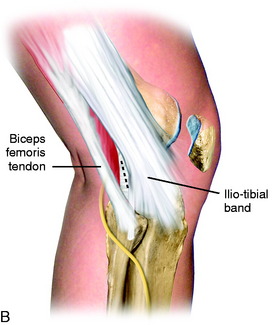
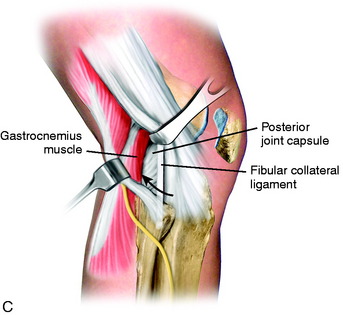
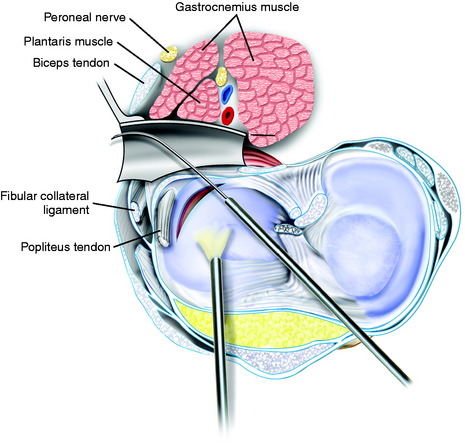
The tourniquet is inflated and the surgeon seated using a headlight with the sterile prepared foot in the surgeon’s lap. The knee is flexed to 60° and a 3-cm skin incision is made just behind the fibular collateral ligament (FCL; Fig. 28-8). The incision is centered just below the joint line (one third above, two thirds below) to allow retrieval of sutures. The interval between the biceps tendon insertion and the iliotibial band is identified and incised, staying superior to the biceps short head muscle fibers. The fascia overlying the posterolateral structures and FCL is gently dissected and peeled from superior to the fibular head. This is performed by applying tension with forceps to the incised fascia and using a thin-blade scissors to peel and strip the fascial tissues to the head of the fibula, protecting the FCL. The retractors are positioned between the biceps tendon and the iliotibial band. The deep layer consists of the posterior capsule and the lateral gastrocnemius tendon. The gastrocnemius tendon has a normal proximal attachment to the posterior capsule, making it necessary to gently dissect the tendon with scissors off the posterior capsule at the joint line. The peroneal nerve inferior to the biceps tendon is palpated and protected, but is not dissected.
The surgeon must be careful to remain posterior to the FCL and other posterolateral structures. The key step is to initially enter the space anterior to the lateral gastrocnemius tendon just above the fibular head. This avoids penetrating and opening the posterior capsule. The space between the posterolateral capsule and the lateral gastrocnemius tendon is further developed bluntly with the index finger. A Henning retractor is used to push the neurovascular bundle medially (Fig. 28-9). The inferior lateral geniculate artery may be visualized in the inferior aspect of the exposure and may be damaged and require electrocoagulation (which is avoided if possible to maintain the vascular supply to the lateral meniscus). The retractor must always be positioned anterior to the gastrocnemius muscle and tendon and directly posterior to the posterior capsule and posterior meniscus bed. The retractor blocks the suture needles from passing too posterior and potentially injuring the common peroneal nerve. During the meniscus suture steps, the surgeon should frequently check the position of the retractor to always ensure that it is anterior to the gastrocnemius muscle. If the retractor is mistakenly placed posterior to the gastrocnemius muscle, the peroneal nerve may be injured.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree