Meniscus
Julie A. Dodds Md
Steven P. Arnoczky DVM, Dipl ACUS
Once described as functionless remains of leg muscle, the menisci are now realized to be integral components in the complex biomechanics of the knee joint.
The menisci are extensions of the tibia, serving to deepen the articular surfaces of the tibial plateau to better accommodate the condyles of the femur.
The functions of the menisci include load bearing, shock absorption, joint stability, lubrication, and proprioception. Loss of the meniscus significantly alters these functions and predisposes the joint to degenerative changes.
The vascular supply of the meniscus is the essential element in determining its potential for repair. This blood supply must have the ability to support the inflammatory response characteristics of wound repair. The peripheral meniscal blood supply is capable of producing a reparative response similar to that in other connective tissue.
When examining injured menisci for potential repair, lesions are often classified by the location of the tear relative to the blood supply of the meniscus and the “vascular appearance” of the peripheral and central surfaces of the tear.
Because no perfect substitute has been created to eliminate the problems seen after meniscal removal, the goal remains meniscal preservation through repair.
The menisci of the knee are C-shaped wedges of fibrocartilage interposed between the condyles of the femur and tibia. Once described as functionless remains of leg muscle (1), the menisci are now realized to be integral components in the complex biomechanics of the knee joint (2,3,4,5,6,7,8,9,10). Knowledge of the form, function, and biology of these unique structures is an important prerequisite to applying the various clinical procedures available to treat, preserve, and replace the menisci of the knee joint. It is the purpose of this chapter to review the basic science aspects of the menisci in order to provide a sound, fundamental basis for the care and treatment of meniscal injuries.
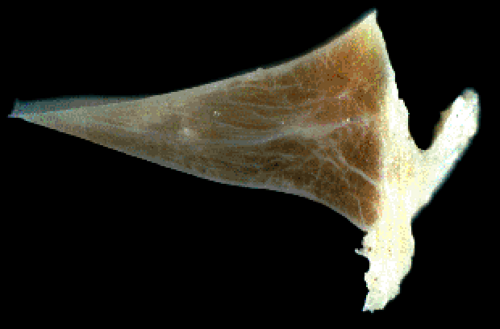
The menisci of the knee joint are actually extensions of the tibia, which serve to deepen the articular surfaces of the tibial plateau to better accommodate the condyles of the femur. The peripheral border of each meniscus is thick and convex and attached to the joint capsule, while the inner border tapers to a thin, free edge (11). The proximal surfaces of the menisci are concave and in contact with the condyles of the femur; their distal surfaces are flat and rest on the tibial plateau (Fig 2-1).
The medial meniscus is somewhat semicircular in form. It is approximately 3.5 cm in length and considerably wider posteriorly than it is anteriorly. The anterior horn of the medial meniscus is attached to the tibial plateau in the area of the anterior intercondylar fossa, anterior to the anterior cruciate ligament (ACL) (Fig 2-2). The posterior fibers of the anterior horn merge with the transverse ligament, which connects the anterior horns of the medial and lateral menisci (11). The posterior horn of the medial meniscus is firmly attached to the posterior intercondylar fossa of the tibia between the attachment of the lateral meniscus and the posterior cruciate ligament (PCL). The periphery of the medial meniscus is attached to the joint capsule throughout its length. The tibial portion of the capsular attachment is referred to as the
coronary ligament. At its midpoint, the medial meniscus is more firmly attached to the femur and tibia through a condensation in the joint capsule known as the deep medial collateral ligament (MCL) (11).
coronary ligament. At its midpoint, the medial meniscus is more firmly attached to the femur and tibia through a condensation in the joint capsule known as the deep medial collateral ligament (MCL) (11).
 Fig 2-2. Human tibial plateau showing the relative size and attachments of the medial and lateral menisci. |
The lateral meniscus is more circular in shape and covers a larger percentage of the articular surface of the tibial plateau than the medial meniscus. The anterior and posterior horns are approximately the same width (Fig 2-2). The anterior horn of the lateral meniscus is attached to the tibia anterior to the intercondylar eminence and posterior to the attachment of the ACL, with which it partially blends (11). The posterior horn of the lateral meniscus is attached posterior to the intercondylar eminence of the tibia, anterior to the posterior horn of the medial meniscus. In addition to this posterior attachment to the tibia, two ligaments may run from the posterior horn of the lateral meniscus to the medial femoral condyle, passing either in front of or behind the origin of the PCL (11). These attachments are known as the anterior meniscofemoral ligament (ligament of Humphrey) and the posterior meniscofemoral ligament (ligament of Wrisberg). Although there is no attachment of the lateral meniscus to the lateral collateral ligament, there is a loose peripheral attachment to the joint capsule (11). Posteriorly, the meniscocapsular continuity is interrupted by the popliteal hiatus, a 1.3 (+/- 0.1) cm opening, which allows passage of the popliteus tendon through the knee joint (12). Occasionally, fascicles attach the popliteus tendon to the meniscus (13).
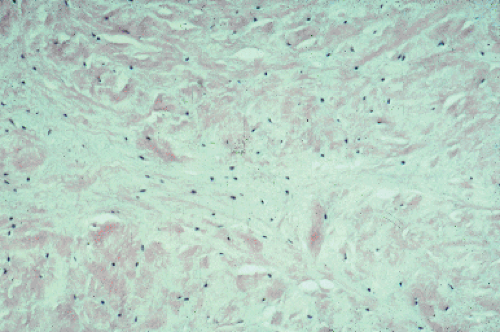
Histologically, the meniscus is a fibrocartilaginous tissue composed primarily of an interlacing network of collagen fibers interposed with cells (3). The cells of the meniscus are responsible for synthesizing and maintaining the extracellular matrix. There is still some debate as to whether the cells of the meniscus are fibroblasts, chondrocytes, or a mixture of both and whether the tissue should be classified as fibrous tissue or fibrocartilage (14). The cells have been termed fibrochondrocytes because of their chondrocytelike appearance and their ability to synthesize a fibrocartilage matrix (Fig 2-3). Two basic types of fibrochondrocytes have been described within the meniscus: a fusiform cell found in the superficial zone of the meniscus and an ovoid or polygonal cell found throughout the remainder of the tissue (14). Although the fusiform cells resemble fibroblasts, they are situated in well-formed lacunae and resemble the chondrocytes found in the superficial (tangential) zone of articular cartilage (14). Both cell types contain abundant endoplasmic reticulum (ER) and Golgi
complexes. Mitochondria are only occasionally visualized, suggesting that, as in articular chondrocytes, the major pathway for energy production for the fibrochondrocytes in their avascular surroundings is probably anaerobic glycolysis (15,16).
complexes. Mitochondria are only occasionally visualized, suggesting that, as in articular chondrocytes, the major pathway for energy production for the fibrochondrocytes in their avascular surroundings is probably anaerobic glycolysis (15,16).
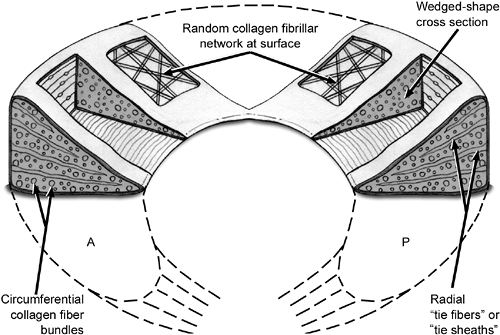
The extracellular matrix of the meniscus is composed primarily of collagen (60% to 70% of the dry weight) (14,15,16,17,18). It is mainly Type I collagen (90%), although Types II, III, V, and VI have been identified within the meniscus (15,16,17,18). The circumferential orientation of these collagen fibers appears to be most directly related to the function of the meniscus. In a classic study describing the orientation of the collagen fibers within the menisci, it was noted that although the principal orientation of the collagen fibers is circumferential, a few small, radially disposed fibers appear on both the femoral and tibial surfaces of the menisci as well as within the substance of the tissue (Figs 2-4, 2-5) (19). It is theorized that these radial fibers act as “ties” to provide structural rigidity and help resist longitudinal splitting of the menisci resulting from undue compression. Subsequent light and electron microscopic examinations of the menisci have revealed three different collagen framework layers: a superficial layer composed of a network of fine fibrils woven into a mesh-like matrix, a surface layer just beneath the superficial layer composed in part of irregularly aligned collagen bundles, and a middle layer in which the collagen fibers are larger and courser and are oriented in a parallel, circumferential direction (20,21) (Fig 2-6). It is this middle layer that allows the meniscus to resist tensile forces and function as a transmitter of load across the knee joint.
 Fig 2-6. Photomicrograph of a longitudinal section of a meniscus under polarized light, demonstrating the orientation of the coarse, deep, circumferentially oriented collagen fibers. |
In addition to collagen, the extracellular matrix of the meniscus also consists of proteoglycans, matrix glycoproteins, and elastin (3,14,15,16,17). The proteoglycan content of the adult meniscus is approximately 10% of the amount found in hyaline cartilage, although this has been shown to vary with age and location within the tissue. A study in the porcine meniscus has shown a higher (two to four times) content of hexosamine and uronic acid in the inner third of the meniscus as compared to the outer two thirds (1,14). These substances have also been known to be more prevalent in the anterior horn as compared to the posterior horn in both the medial and lateral meniscus (1,8). The glycosaminoglycan (GAG) profile of the adult human meniscus has been reported to consist of chondroitin 6-sulfate (40%), chondroitin 4-sulfate (10% to 20%), dermatan sulfate (20% to 30%), and keratan sulfate (15%) (3,14,15,16).
Matrix glycoproteins, such as the link proteins that stabilize the proteoglycan-hyaluronic acid aggregates, and a 116-k Dalton protein of unknown consequence, have also been identified within the extracellular matrix (3,14,15,16). In addition, adhesive glycoproteins, such as Type VI collagen, fibronectin, and thrombospondin, have been isolated from the meniscus (15,16). These macromolecules have the property to bind to other matrix macromolecules and/or cell surfaces and may play a role in the supramolecular organization of the extracellular molecules of the meniscus (15,16).
While the term “shock absorber” has often been used to describe the meniscus, the menisci actually serve many functions in the human knee. Additional functions are theorized to be load bearing, lubrication, and proprioception. The meniscal function of load bearing may be clinically inferred by the degenerative changes that accompany meniscectomy. Fairbank (22) described radiographic changes following meniscectomy, which included narrowing of the joint space, flattening of the femoral condyle, and the formation of osteophytes. These changes were attributed to the loss of the weight bearing function of the meniscus. Biomechanical studies have demonstrated that at least 50% of the compressive load of the knee joint is transmitted through the meniscus in extension, and approximately 85% of the load is transmitted in 90 degrees of flexion (23). In the totally meniscectomized knee, the contact area is reduced approximately 50% (23,24). This significantly increases the load per unit area and results in articular damage and degeneration. Partial meniscectomy has also been shown to significantly increase contact pressures (25). In an experimental study, resection of as little as 15% to 34% of the meniscus increased tibiofemoral contact pressures by more than 350% (26). Thus, even partial meniscectomy can affect the ability of the meniscus to function in load transmission across the knee (5,6,25,27,28,29,30,31,32).
Another proposed function of the meniscus is that of shock absorption. By examining the compressive load-deformation response of the normal and meniscectomized knee, it has been suggested that the viscoelastic menisci may function to attenuate the intermittent shock waves generated by impulse loading of the knee during gait (26,33). Studies have shown that the normal knee has a shock-absorbing capacity about 20% higher than knees that have undergone meniscectomy (33). As the inability of a joint system to absorb shock has been implicated in the development of osteoarthritis (34), the shock absorption mechanism would appear to play a role in maintaining the health of the knee joint.
In addition to the role of the meniscus in load transmission and shock absorption, the menisci are thought to contribute to knee joint stability (9,35,36,37). Although medial meniscectomy alone does not significantly increase anterior-posterior joint stability, several studies have shown that medial meniscectomy in association with ACL insufficiency significantly increases the anterior laxity of the knee (9,35,36,37). However, lateral meniscectomy, alone or in association with ACL insufficiency, has not been shown to increase knee joint laxity (9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree