Medial Patellofemoral Ligament Reconstruction and Repair
Andrew J. Cosgarea
Brett M. Cascio
INDICATIONS
Over the years, a large number of procedures have been described to treat patellar instability. Recently there has been a great deal of interest in procedures that address the medial patellofemoral ligament (MPFL), the primary soft tissue passive restraint to pathologic lateral patellar displacement (2,4). The MPFL is torn when the patella dislocates (10,15), and a variety of techniques have been described to repair (3,10,15) or reconstruct (5,12,16) the ligament in an attempt to restore its function as a checkrein.
History
The indication for MPFL surgery is patellar instability; therefore, the most important clinical determination to make is whether anterior knee pain is associated with instability. The much more common clinical entity of patellofemoral pain syndrome is nearly universally treated nonoperatively. Among the spectrum of disorders causing anterior knee pain, patellar instability represents a distinct clinical entity that is usually amenable to surgical treatment. Instability represents a continuum ranging from minor incidental subluxation episodes to traumatic dislocation events. Dislocations can occur from an indirect twisting mechanism as the upper body rotates while the foot remains planted on the ground. Less commonly, a direct blow along the medial aspect of the patella during sports activity drives the patella laterally. Medial dislocations are rare in patients who have not undergone previous lateral retinacular release surgery. Sometimes the patella reduces spontaneously, although on occasion a formal reduction maneuver may be necessary. With a first dislocation episode, the patient usually experiences significant pain, and swelling is caused by soft tissue and intra-articular damage. The resulting swelling and muscle weakness may take several weeks to resolve. Patients who sustain multiple episodes tend to experience less dramatic symptoms. Subluxation episodes also tend to be less dramatic. Patients may describe a feeling of instability with or without pain. Instability usually occurs with trunk rotation during physical activity, as the foot remains planted on the ground. The discomfort is usually anterior, and may be bilateral, especially in patients with malalignment or hyperlaxity.
Physical Examination
Careful physical examination can confirm patellar instability. Alignment is evaluated with the patient standing or walking. The knee is then observed for extra-articular swelling or an effusion. The soft tissues are palpated, and the examiner should try to identify an area of tenderness along the course of the MPFL, as this usually identifies the location of the tear. A thorough cruciate and collateral ligament examination is necessary to rule out concomitant pathology. Medial collateral ligament tears often occur at the same time as a patellar dislocation. The quadriceps angle (Q angle) can be measured as a gross assessment of the lateral force vector. Patellar tracking is observed as the knee is extended from a flexed position. The patella has a tendency to slip laterally as the knee approaches the last 20 degrees of extension and the patella is no longer constrained by the lateral trochlear ridge (J sign). Patellar translation is assessed by pushing on the medial side of the patella with the knee in full extension. The amount of translation is quantified in quadrants and compared to the normal contralateral knee. An indistinct endpoint suggests MPFL incompetence. A feeling of apprehension (apprehension sign) supports the diagnosis of instability. Lateral retinacular tightness is assessed by manually elevating the lateral edge of the patella (tilt test).
The standard radiograph series includes anteroposterior, lateral (30 degrees flexion), tunnel, and sunrise (30 to 45 degrees flexion) views. The tunnel view may demonstratel osteochondritis dissecans lesions or loose bodies in the notch. The sunrise view shows the degree of subluxation and tilt. Computed tomography (CT) scan axial images (20 degrees flexion) are occasionally helpful to identify subluxation and tilt. Magnetic resonance imaging (MRI) demonstrates the characteristic bone bruise pattern involving the medial facet of the patella and the proximal lateral femoral condyle in patients who have recently sustained a dislocation.
MPFL reconstruction is indicated in skeletally mature patients with symptomatic recurrent lateral subluxation or dislocation. Patients have usually failed attempts at nonoperative treatment including activity modification, physical therapy, and knee bracing. Some authors recommend MPFL repair for patients following their first patellar dislocation (15). We usually recommend treating an initial dislocation episode nonoperatively, but will repair an acute MPFL tear when surgery is necessary for concomitant intra-articular pathology (large loose body, meniscus tear). MPFL repair techniques may also be used to treat recurrent instability. The MPFL becomes attenuated and functionally incompetent with repeated instability episodes, so it is tightened by cutting, shortening, and reattaching it at the patellar or femoral insertion, or by midsubstance imbrication.
CONTRAINDICATIONS
MPFL repair and reconstruction are contraindicated in patients with medial instability or isolated anterior knee pain. Great care should be taken not to overtighten the MPFL or malposition the graft as this will result in excessive medial patellofemoral joint pressures and is likely to exacerbate patellofemoral pain, particularly in patients with medial patellofemoral chondral damage. The distal femoral growth plate is at risk for injury in skeletally immature patients. The traditional MPFL reconstruction technique can be modified so that the graft is passed around the proximal superficial medial collateral ligament (MCL), or sutured directly to adjacent soft tissue.
Tibial tuberosity osteotomy procedures, such as the Elmslie-Trillat, have a theoretical advantage in patients with greater degrees of malalignment. The Fulkerson anteromedialization osteotomy is preferred in patients with malalignment and degenerative changes involving the inferior pole of the patella or lateral facet (9). MPFL reconstruction or repair can be combined with distal osteotomy if either alone is insufficient to provide adequate stability.
SURGERY
Patient Positioning
The patient is placed supine on a standard operating room table. A vertical post is used to facilitate arthroscopic evaluation and can be removed before starting the open portion of the surgery. A tourniquet is used to facilitate hemostatis and visualization. Surgery is performed on an outpatient basis using general or regional anesthesia. Prophylactic intravenous antibiotics are administered before incision.
Exam under Anesthesia
After induction of satisfactory anesthesia, a comprehensive examination is performed. Patellar stability, translation, and tilt are usually easier to characterize when the patient is anesthetized. With the knee extended, the position of the patella is determined at rest, and with a lateral translation force applied. The amount of translation on the symptomatic side is compared to the normal lateral patellar translation in the contralateral knee (Fig. 2-1). The patella is pushed laterally, and the amount of translation and the consistency of the endpoint are assessed. The examiner everts the lateral edge of the patella to determine whether the lateral retinaculum is tight. If the patient’s symptoms and exam are consistent with excessive lateral retinacular tightness, then consideration should be given to performing a concomitant arthroscopic lateral retinacular release.
Diagnostic Arthroscopy
Arthroscopy is performed first using the standard superolateral, inferomedial, and inferolateral portals. The suprapatellar pouch, the medial and lateral parapatellar gutters, and the posteromedial and posterolateral compartments are carefully assessed for loose bodies. The articular surfaces of the patella and trochlear are thoroughly scrutinized for chondral lesions. The medial facet of the patella and the proximal portion of the lateral femoral condyle are the areas most commonly injured during a traumatic patellar dislocation. Hemorrhage may be noted in the soft tissue adjacent to the medial edge of the patella in patients who have sustained a recent avulsion of the MPFL insertion. Patellar tracking in the trochlear groove is visualized as the knee is ranged. Any large chondral lesions are addressed surgically with debridement, microfracture, or repair techniques as indicated. In some circumstances, large defects should be unloaded using tibial tuberosity anteromedialization. Arthroscopic lateral retinacular release may be performed at this point, although we have not found that to be routinely necessary.
Surface Landmarks
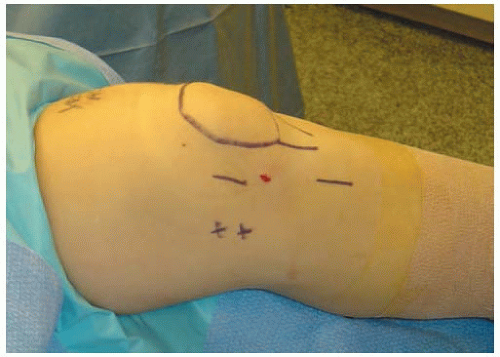
After removing the arthroscopy equipment, a marking pen is used to identify the important bony landmarks (Fig. 2-2). Marks are made over the patella, tibial tuberosity, adductor tubercle, and medial femoral epicondyle. The pes anserine tendon insertion site is palpated, and a 3- to 4-cm oblique mark is made over the sartorial fascia insertion on the proximal medial tibia for the harvest site incision. A second 3- to 4-cm line is drawn directly over the MPFL, halfway between the medial border of the patella and the medial femoral epicondyle. The position is modified if the location of the MPFL tear has been ascertained from the preoperative examination or MRI, and an MPFL repair is planned.
The tourniquet is raised while the knee is in an extended position. A longitudinal incision is made midway between the medial edge of the patella and the medial epicondyle. Sharp and blunt dissection is used to expose the thick medial retinacular layer contiguous with the inferior border of the vastus medialis obliquus muscle. With gentle dissection, the superior and inferior borders of the MPFL are isolated (Fig. 2-3). In patients who have sustained a recent dislocation, it may be possible
to identify the site of the MPFL tear at the medial border of the patella, the medial femoral epicondyle, or in midsubstance.
to identify the site of the MPFL tear at the medial border of the patella, the medial femoral epicondyle, or in midsubstance.
Medial Patellofemoral Ligament Repair
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree