Anatomic Anterior Cruciate Ligament Double-Bundle Reconstruction
Mario Ferretti
Wei Shen
Hanno Steckel
Freddie H. Fu
INDICATIONS/CONTRAINDICATIONS
Anterior cruciate ligament (ACL) tear is a common injury in orthopaedic sports medicine. Surgical reconstruction is the preferred choice in management to restore knee stability and prevent intra-articular injuries. Current techniques in ACL surgery have been associated with satisfactory long-term results in the majority of patients; however, there remains a considerable subset of patients with unsatisfactory outcomes. Specifically, patients report difficulties relating to rotational instability and return to previous level of activity. The anatomic ACL double-bundle (DB) reconstruction aims to restore the original anatomy and footprints of the ACL by reconstructing the anteromedial (AM) and posterolateral (PL) bundle to achieve a better functional outcome, which is in contrast to single-bundle (SB) reconstruction, which attempts to restore the fibers of the AM bundle. The indications for a reconstruction of a torn ACL applying the anatomic ACL DB reconstruction are like the traditional SB reconstruction and are influenced by several factors. Universally accepted indications for ACL reconstruction are heavy work occupation, high-risk lifestyle, demanding level of sports activity, instability in spite of rehabilitation, and associated injuries like meniscal tears or severe injuries to other ligament structures in the knee. Age is also an important parameter to take into account; however, it is not so much the biologic age, but the status of the knee and the individual lifestyle which have to be considered.
Contraindications for the anatomic ACL DB reconstruction include advanced osteoarthritis of the knee, patients who are unable to comply with the postoperative rehabilitation protocol, and acute intra-articular sepsis. Open physes are not an absolute contraindication for the DB reconstruction, since several authors have described satisfactory results with reconstruction of the ACL using soft tissue grafts passed through the transphysial drill holes. However, extra attention should be paid to patients with large open physes or patients with potential to grow.
PREOPERATIVE PLANNING
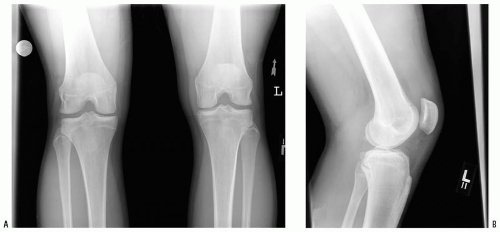
Planning the surgical procedure includes taking the patient’s history as well as a physical examination. For outcome evaluation, clinical parameters such as range of motion (ROM), Lachman grade, anterior drawer grade, pivot-shift grade, objective measurements of knee laxity as obtained with KT-1000 arthrometer, and scores such as the International Knee Documentation Committee Subjective Knee Form (IKDC) and Lysholm are important and are routinely applied. Especially validated outcome instruments like 36-Item Short Form Health Survey (SF-36), Activities of Daily Living (ADLS), Knee Injury and Osteoarthritis Outcome Score (KOOS), and Sports Activities Scales (SAS) are also needed for future evaluation of the DB reconstruction. Imaging of the knee is performed with routine radiographs to determine fractures, osteoarthritis, and the alignment of the lower extremity (Fig. 13-1). Magnetic resonance imaging is always done to assess further intra- and extra-articular injury and to confirm the rupture of the ACL (Fig. 13-2). The time interval from injury to reconstruction is not as important as the condition of the knee at the time of surgery. The knee should have minimal effusion and full range of motion. The patient must be physically and mentally prepared for surgery and free of pain when determining the date of reconstruction.
SURGERY
The patient and the limb to be operated on are identified by the surgeon in the preoperative holding area. In the operating room, the patient is placed in a supine position. Either general or spinal anesthesia is performed according to the preference of the patient and anesthesiologist. Examination under anesthesia is executed with the Lachman test and pivot shift. Special attention is given to the laxity of the knee joint. Under anesthesia, when the pivot shift is grade 1 or graded as a gliding pivot and the side-to-side difference using KT 1000 is less than 5 mm, a possible partial tear of the ACL is considered as a differential diagnosis and further arthroscopic evaluation will elucidate the correct diagnosis. It is important to note that in the case of a complete ACL tear, an anatomic ACL DB reconstruction will be performed. Rarely, when a partial tear of the ACL is diagnosed, an augmentation of the torn bundle, AM or PL bundle, may be a logical approach.
The procedure is performed with the patient in supine position with the nonoperative leg placed in a well-leg holder in the abducted position. The operative leg is exsanguinated by elevation for 3 minutes; a pneumatic tourniquet is applied around the upper thigh and insufflated to 350 or 400 mmHg depending on the patient’s size. Finally, the operative leg is placed in an arthroscopic leg holder, which allows good range of motion (Fig. 13-3), sterile preparation, and draping. The surgery is performed in a stepwise fashion as follows: (a) evaluation under anesthesia, (b) patient set-up, (c) graft preparation, (d) evaluation of the ACL rupture pattern and marking of the footprints of the ACL, (e) positioning and preparation of the tunnels, (f) graft passage and fixation, (g) closure and postoperative assessment of stability, and (h) postoperative management and rehabilitation.
Technique
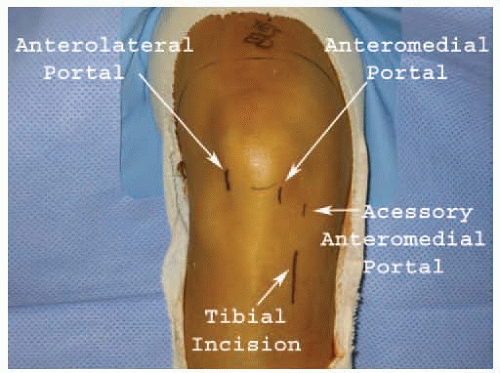
Arthroscopy is performed for diagnosis and treatment of associated injuries. The portals are critical to obtain optimal intra-articular visualization and management of the arthroscopic instruments. We use the standard anterolateral (AL) and anteromedial (AM) portal; an accessory anteromedial portal (AAM) is also used (Fig. 13-4). To establish the AAM portal, the arthroscope is placed into the standard AL or AM portal and an 18-gauge spinal needle is inserted medially and distally to this portal just above the meniscus to reach the center of the femoral footprint of the PL bundle (Fig. 13-5). Once the needle is placed correctly, the AAM portal is performed with a #11 blade. While the arthroscopy is being performed, the grafts are being prepared in a back table by another surgeon. We prefer the use of two separate tibialis anterior or tibialis posterior tendon allografts. These allografts are usually 24 to 30 cm in length, and we fold each tendon graft to obtain 12 to 15 cm double-stranded grafts (Fig. 13-6). First, the tendon allografts are trimmed and the diameters of the double-stranded grafts are adjusted. Usually, the AM tendon graft is trimmed such that the diameter of the double-stranded graft is 8 mm; the PL graft is trimmed such that the diameter of the double-stranded graft is 7 mm. However, the diameters of the graft should be smaller in a small patient. The ends of the grafts are sutured using a baseball stitch fashion with 2-0 Ticron sutures. An EndoButton CL (Smith & Nephew, Andover, MA) is used to loop each graft and obtain a double-stranded graft. The length of the EndoButton loop is chosen according to the measured length of the femoral tunnels.
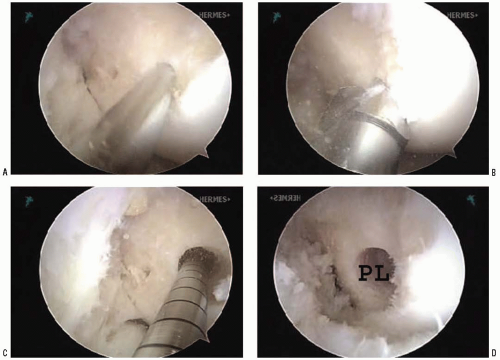
During the arthroscopy, it is important to observe the rupture pattern of the ACL (Fig. 13-7). This step definitively diagnoses the total tear of the ACL and shows us the original footprint of the AM and PL bundles on the lateral wall of the intercondylar notch and on the tibial side (Fig. 13-8). When identified, the footprints of each bundle are marked by a thermal device (Artrocare Corporation, Sunnyvale, CA). A small hole in the center of the femoral AM and PL footprint is created by Steadman awl to facilitate further guidewire placement to create the femoral tunnels (Fig. 13-9). After marked by a thermal device, the remaining tibial footprint fibers are left intact due to their proprioceptive and vascular contributions. It is important to note that in acute cases, the rupture pattern and original anatomy are more easily observed than in chronic cases, in which you may not find the ACL footprints as well. A good understanding of the double-bundle ACL anatomy is essential to identify and mark the correct footprints.
 FIGURE 13-3 A knee holder is used to keep the surgery knee stable during the surgery (A). It also allows a good range of motion, both extension (B) and flexion (C), during the surgery. |
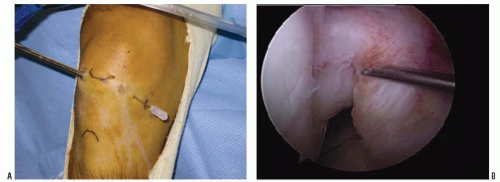 FIGURE 13-5 A spinal needle is inserted to decide the position of the accessory anteromedial portal. A: Outside and (B) inside. |
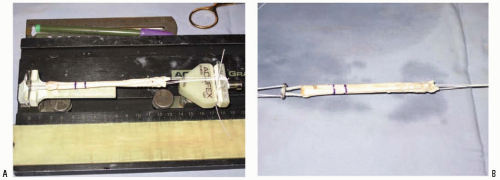 FIGURE 13-6 A,B: The graft is prepared on a back table by an assistant surgeon. The length of the femoral tunnels is measured, and the length of the grafts is adjusted accordingly. |
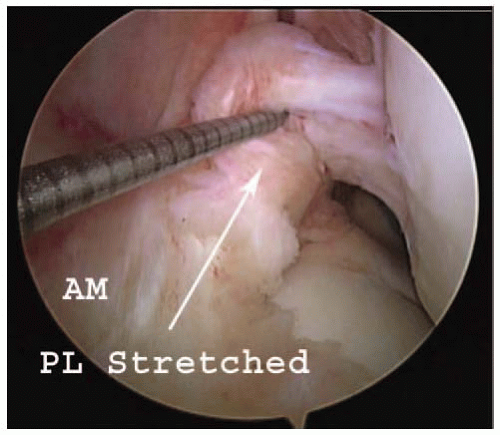 FIGURE 13-7 A thermal device is used to investigate the injury pattern of ACL. One example shows that the AM bundle is intact, whereas the PL bundle is stretched. |
The PL femoral tunnel is the first tunnel to be drilled. The PL femoral tunnel is drilled through the AAM portal, and a 3.2-mm guidewire is inserted through the portal. The tip of the guidewire is placed on the small hole created previously by Steadman awl on the center of the femoral footprint of the PL bundle. Once the tip of the guidewire is malleted in the correct position, the femoral PL tunnel is drilled with an acorn drill that is inserted over the guidewire. The PL femoral tunnel is drilled to a depth of 25 to 30 mm (Fig. 13-10). The far cortex is breached with a 4.5-mm EndoButton drill (Smith & Nephew, Andover, MA) and the depth gauge is used to measure the distance to the far cortex. It is important to note that during the drilling of the PL bundle tunnel, the arthroscopy is placed through the anteromedial portal and the tunnel is drilled through the accessory anteromedial portal (Fig. 13-11). It is also important to note that during the entire procedure to create a PL femoral tunnel the knee is positioned at 110 degrees of flexion, which brings the PL bundle footprint anteriorly.
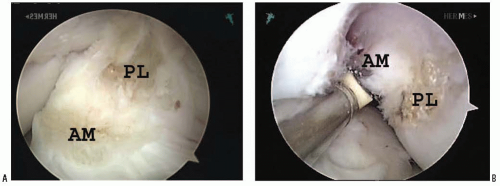 FIGURE 13-8 The insertion sites of AM and PL on both tibial side (A) and femoral side (B) are marked by a thermal device. |
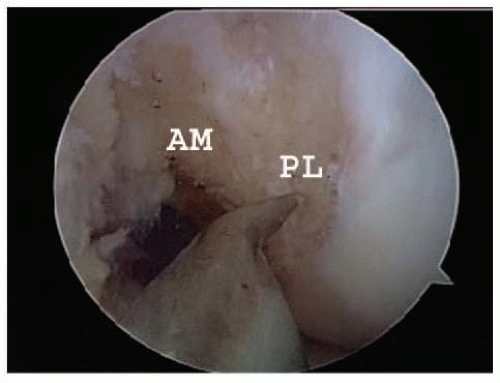 FIGURE 13-9 A Steadman awl is used to mark the desired femoral AM and PL positions for guide pins. It also makes it easier for the guide pins to stick to the chosen spot. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree