Type
Ulnar nerve neuropathy
I-A
None
I-B
Mild
II
Moderate or severe
In throwing athletes, assessing the integrity of the ulnar ligament is imperative. When applying valgus force to the elbow slightly flexed with the forearm in pronation and wrist in flexion, opening of the joint and pain appear in patients with ligament insufficiency.
Medial epicondylitis presents with cervical radiculopathy in slightly more than half the patients. Weakening of the flexor carpi radialis and pronator teres and imbalance of the flexor and extensor muscles from the C6 and C7 radiculopathy allow for easy onset of medial epicondylitis. Patients with medial epicondylitis should be examined for C6 and C7 radiculopathy to ensure proper treatment. Physicians dealing with golfers, pitchers, or other patients with medial epicondylitis should be aware of the association between these two diagnoses to optimize care [8].
Quality anteroposterior, oblique, oblique axial in flexion, posteroanterior axial, and cubital tunnel radiographic views should be assessed for the presence of calcification or a bony exostosis at the medial epicondyle [9]. When instability is suspected, elbow stress radiographs can be of help in identifying ulnar ligament tears.
Musculoskeletal ultrasonography allows for an inexpensive dynamic evaluation of commonly injured structures [10]. Medial epicondylitis is ultrasonographically diagnosed when a focal hypoechoic (degeneration) or anechoic (tear) region with increased vascularity in color Doppler imaging is present at the medial epicondylar muscles with or without calcification [11].
Magnetic resonance (MR) imaging is the preferred imaging modality for chronic elbow pain [12, 13]. MR imaging findings of patients with clinically diagnosed medial epicondylitis include thickening and increased T1 and T2 signal intensity of the common flexor tendon and soft tissue edema around the tendon [14]. The use of MR arthrography at some imaging centers has been reported to have great sensitivity in identifying UCL tears [15].
When ulnar nerve injury or cervical radiculopathy are suspected, the use of electromyographic studies is necessary.
27.4 Treatment Strategy
27.4.1 Non-operative Treatment
Once the diagnosis is established in acute or subacute cases, a period of conservative management is mandatory as a high percentage of patients are known to heal spontaneously without significant intervention. Stahl et al. [3] compared prospectively the effect of local injection of lidocaine and methylprednisolone versus saline solution, associated with physical therapy and nonsteroidal anti-inflammatory drugs (NSAIDS) to treat medial epicondylitis and showed that after 3 and 12 months, patients reported significant improvement in both groups without significant differences. Furthermore, non-operative treatment has been shown to be effective in up to 90 % of cases [3].
There are many options regarding conservative management, but first line should include a short 2–4 week course of NSAIDS associated with rest. NSAIDS are useful in dealing with the concomitant synovitis, and refraining from the injuring activity is the key in avoiding further damage. A detailed review of the specific sport technique and equipment might help as subtle modifications in these can reduce the stress to the CFPO and rapidly improve symptoms.
Full immobilization of the elbow is rarely necessary and reserved for patients with acute symptoms and significant pain and disability, but counterforce bracing during sport practice may be helpful, although it is less effective than in lateral epicondylitis cases.
Different physical therapy modalities might be of use: a combination of ice and flexibility and strengthening training is effective in many tendinosis. The short-term analgesic effect of manipulation techniques may allow more vigorous stretching and strengthening exercises resulting in a better and faster recovery [16]. Forearm Kinesio Taping may enhance absolute force sense and improve pain condition for athletes suffering from medial epicondylitis as baseball players [17].
Instrumental electrophysical modalities – ultrasound, extracorporeal shock wave therapy (ESWT), transcutaneous electrical nerve stimulation (TENS), laser therapy, iontophoresis, phonophoresis, and others – can provide benefit, mainly with ultrasound and laser [18, 19].
Local corticosteroid injections seem to be effective in the short term but not in the long term [3, 19]. Their usefulness is thus controversial. Subcutaneous deposition of the injection must be avoided to prevent complications like hypopigmentation and fat atrophy.
Other types of injections and acupuncture: Suresh et al. [20] suggested that a combination of dry needling and autologous blood injection under ultrasound guidance might be an effective treatment for refractory medial epicondylitis, but all these types of techniques continue to be controversial.
Platelet-rich plasma (PRP): reviewing current literature regarding the biology of PRP and the efficacy of using PRP to augment healing of tendon, ligament, and muscle injuries, as well as early osteoarthritis, the most compelling evidence to support the efficacy of PRP is for its application to tendon damage associated with lateral and medial epicondylitis. PRP therapies have shown to be safe, but a number of questions remain unanswered, including the optimal concentration of platelets, what cell types should be present, the ideal frequency of application, or the optimal rehabilitation regimen for tissue repair and return to full function [21].
27.4.2 Surgical Treatment
It is indicated if conservative treatment fails, after a not well defined period. Patient compliance with activity modification and therapy exercises is mandatory before deciding to perform a surgical procedure. Typically a period of at least 6 months of conservative treatment is required to define failure, but in athletes about 2–4 months of ineffective conservative treatment might be enough to proceed to surgery. This can be accelerated if structural injury (such as tearing or detachment of the CFPO) is identified or if associated progressive ulnar nerve damage is detected [6].
The patients should know that operative treatment usually improves patient function significantly with increase in grip strength and improvement of clinical scores like DASH or Mayo postoperatively [22, 23]. But, 1 year after surgery, 5–30 % of patients will still experience moderate to severe tenderness at the medial epicondyle [24]. No major complications are usually observed.
Little has been published regarding operative techniques for medial epicondylitis. It is generally agreed that the same surgical principles used on the lateral side apply to the medial side: exposing the affected tendon, excising the pathologic portion, repairing the resultant defect, and sometimes reattaching any elevated tendon origin back to the epicondyle [6].
General or regional anesthesia is used. The patient is placed supine with the affected arm in a hand table, and a tourniquet is applied. A 6 cm incision is made centered just anterior to the medial epicondyle. Subcutaneous tissue is dissected. In this point, the medial antebrachial cutaneous nerve is placed at risk of injury. The CFPO is identified. Ulnar nerve and ulnar collateral ligament must be protected, but it is not necessary to expose them if they are not affected. The pronator teres and flexor carpi radialis interval is incised. The degenerated tissue is excised. Creating a bleeding surface in the medial epicondyle by removing fibrous tissue and performing multiple small drill holes might be effective. The remaining tendon is reattached to its origin if possible. At the end, the interval, the subcutaneous tissue, and the skin are closed after placing a drain. A posterior plaster splint is placed with the elbow at 90° and forearm and wrist in neutral position [7]. Vangsness and Jobe [4] reported good to excellent results in more than 95 % of patients with this technique, 86 % of the patients referred no limitation in elbow use a mean of 4 years after the surgical procedure.
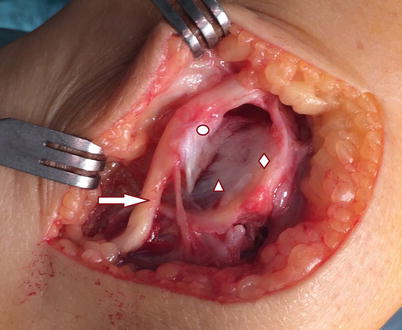
The FETOR technique (fascial elevation and tendon origin resection) which facilitates the complete visualization and resection of the CFPO with limited soft tissue dissection is an effective and safe method described for the treatment of chronic recalcitrant medial epicondylitis [24]. It also minimizes the risk of incomplete removal of the degenerated tendon and allows a rapid rehabilitation. The most important step in this technique is elevating the intact fascia before CPFO resection and a carefully closing of the fascia at the end (Figs. 27.1 and 27.2). Kwon et al. [24] have recently presented the two-year results of this technique, with good or excellent results in 90 % of cases.