Chapter 24 Medial and Posteromedial Ligament Injuries
Diagnosis, Operative Techniques, and Clinical Outcomes
INDICATIONS
Medial ligament injuries are among the most frequently treated problems of the knee joint, with the majority not requiring operative intervention. Whereas isolated superficial medial collateral ligament (SMCL) ruptures are common, concomitant damage to the anterior cruciate ligament (ACL) also occurs in many cases, especially in young and active patients.6,11,14,28,33
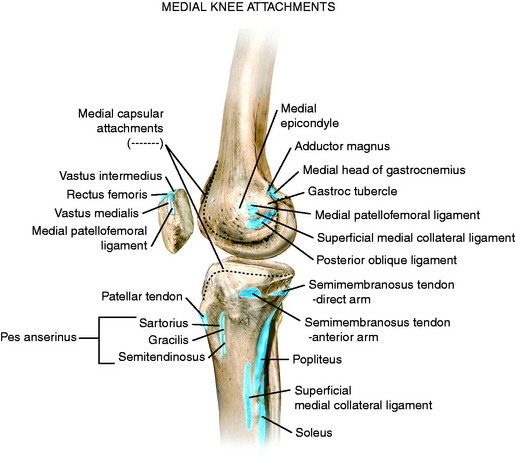
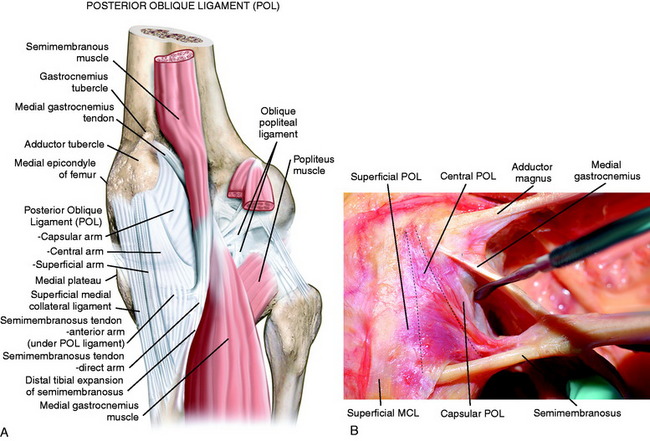
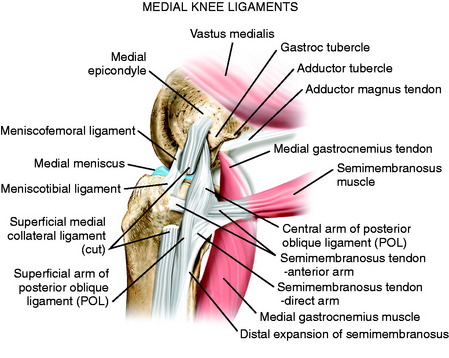
The medial structures identified for purposes of surgical treatment consist of the SMCL, deep medial collateral ligament (DMCL, including meniscus attachments), and the PMC, which includes the structures referred to as the POL and semimembranosus attachments.22,44 The key to the diagnosis and treatment of medial ligament injuries relies on a comprehensive understanding of the intricate anatomy on the medial side of the knee. This is presented in detail in Chapter 1, Medial and Anterior Knee Anatomy. In Figure 24-1, the osseous attachments of the medial structures are shown. Figure 24-2 shows the medial and posteromedial ligament structures, which are discussed in detail. Figure 24-3 shows the relationship of the semimembranosus muscle attachments to the posteromedial structures and POL. These include the bifurcation of the semimembranosus tendon into a direct and anterior area just distal to the joint line and a minor attachment of the direct arm to the medial coronary ligament along the posterior horn of the medial meniscus. The semimembranosus tendon sheath makes up a distal tibial expansion that includes a medial and lateral division. A major attachment of the semimembranosus forms the oblique popliteal ligament, which is a broad fascial band that courses laterally attaching to the fabella, posterolateral capsule, and plantaris (see Chapter 1, Medial and Anterior Knee Anatomy, Figs. 1–4 to 1–10).
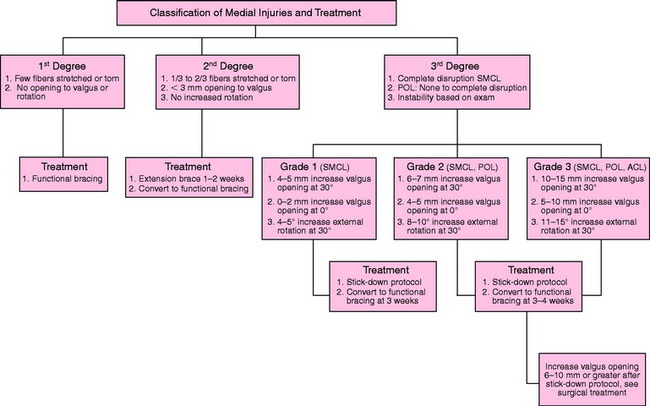
It is important to understand and classify the soft tissue injury of all the medial structures. The majority of acute medial ligament injuries that involve damage to the SMCL alone, or SMCL and PMC, are treated conservatively. The nonoperative treatment algorithm is shown in Figure 24-4 and discussed later in more detail. Gross major disruption of all of the medial structures alone or in addition to the ACL or PCL tears involve a group of select knees. The treatment of these gross ligament disruptions is discussed in a later section of this chapter.
In cases of chronic injury to the medial ligaments, it is important to obtain a complete history and objective and functional rating. The authors’ use the Cincinnati Knee Rating System (CKRS) for this analysis (see Chapter 44, The Cincinnati Knee Rating System) to determine patient complaints of giving-way and the levels of activity at which this symptom occurs as an indication for surgical stabilization procedures. In this chapter, instability refers to an increase in abnormal motion limits as detected on the physical examination, and is not used to indicate giving-way events.
CONTRAINDICATIONS
Critical Points CONTRAINDICATIONS
CLINICAL BIOMECHANICS
A considerable amount of discrepancy exists in the literature regarding the use of terminology to describe and classify the medial ligament injuries from an anatomic standpoint and the abnormal motion limits that exist (see Chapter 3, The Scientific Basis for Examination and Classification of Knee Ligament Injuries). The authors agree with Hughston and coworkers19 that the clinician must clearly separate and classify medial ligament tears into first degree (tear involving a few fibers), second degree (partial tear, no instability, ≤3 mm of medial joint opening), and third degree (complete rupture) (TABLE 24-1; see also Fig. 24-4).5,10,11,13,20,21,32,42 This is one of the earliest systems devised and is based on a classification proposed by the American Medical Association.1 The problem has arisen, as amply demonstrated in TABLE 24-1, that this classification system has been modified extensively by different authors and it is often not possible to categorize the injury severity of the knees under treatment. For example, some authors in TABLE 24-1 refer to a second-degree or grade 2 instability as one that has a definite laxity or mild to moderate instability, even though the original definition of a second-degree or grade 2 injury represented only a partial ligament tear without any major increase in medial joint opening. Thus, it is necessary in the review of the literature to perform a subset analysis, which has been done in this chapter, to try to obtain the category or type of injury under treatment and the authors’ treatment recommendations.
TABLE 24-1 Published Classification Systems for Ruptures to the Medial Structures of the Knee
MCL, medial collateral ligament.
Critical Points CLINICAL BIOMECHANICS
For purposes of this chapter, the injury classification based on the clinical examination is shown in Figure 24-4. Note that the medial ligament injuries are based on the first-, second-, and third-degree original classification system proposed; the increases in medial joint opening for the third-degree injury are based on the increase in medial joint opening and external tibial rotation. Some classification systems use a system in which each grade represents a further 5-mm increase in joint opening (grades 1, 2, and 3) over the contralateral normal knee, whereas other systems use the grade to represent the absolute amount of joint opening in the injured knee (grades 1+, 2+, and 3+). This chapter uses the increase in millimeters of medial joint opening between the injured and the contralateral normal knee to diagnose the medial ligament injury, because this is the system used in the published biomechanical and kinematic studies to be presented.
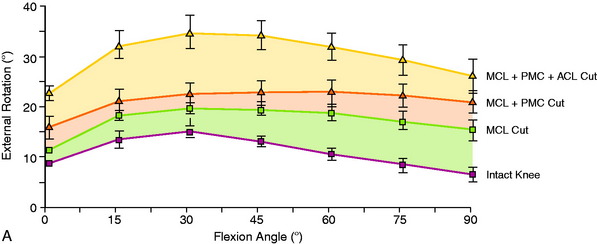
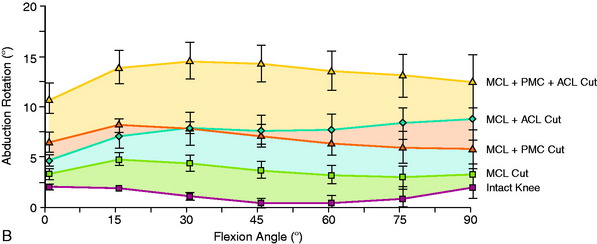
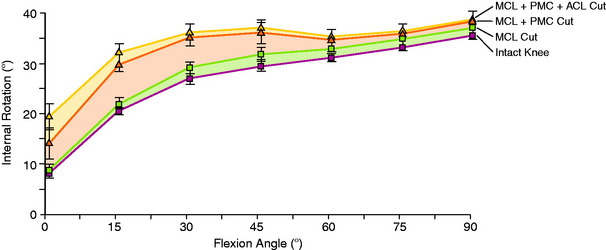
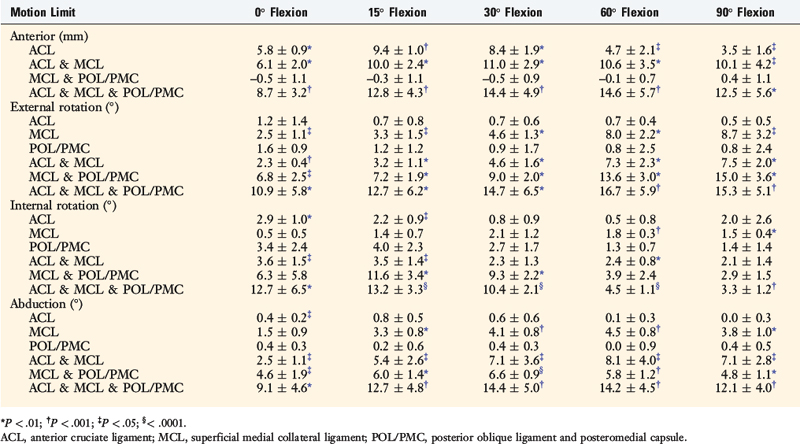
A review of the in vitro cadaveric biomechanical function of the medial ligaments and ACL in resisting medial joint opening, external tibial rotation, and internal tibial rotation is provided in Figure 24-5, summarized in TABLE 24-2, and discussed in more detail in Chapter 3, The Scientific Basis for Examination and Classification of Knee Ligament Injuries. A finding of increased medial joint space at 30° of flexion (third-degree sprain, parallel fibers of the SMCL), but not at 0° of flexion, indicates that the PMC (including the POL) is still functional. Any further increase in medial joint opening at 0° indicates concurrent damage to the PMC. With complete disruption of the SMCL and PMC, the ACL and PCL become a restraint to further medial joint opening. Knees with rupture to both the medial collateral ligament (MCL) and the POL will demonstrate increases in external tibial rotation (average of 9° at 30° of flexion), increases in internal tibial rotation (average of 12° at 30° of flexion), and increases in abduction testing at 0° and 30° of flexion (averages of 6° and 9°, respectively). The results show the importance of performing the dial tibial rotation test (see Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes) to determine the anterior subluxation of the medial tibial plateau with medial ligament injuries. With a combined MCL/POL injury, there will be a noticeable increase in internal and external tibial rotation. The PMC is an important structure for stabilizing the extended knee under valgus loading.35–37 With knee flexion, the PMC slackens and the MCL becomes the dominant restraint. In the extended knee, with posterior drawer and internal rotation, the PMC tightens based on its attachments at the femur (just posterior to the adductor tubercle) and the posteromedial aspect of the tibia. The increase in abduction for a combined MCL/POL injury and MCL/ACL injury at 15° to 45° of flexion is nearly the same (see Fig. 24-5B). The major difference between these injuries is in increased abduction at full extension in the MCL/POL ruptured knee.
TABLE 24-2 Increases in Motion Limits Relative to the Intact Knee That Occurred When the Indicated Structures Were Sectioned
The increase in medial joint opening and external tibial rotation shown in Figure 24-5 provides an indication of an associated ACL tear when these motion limits are distinctly abnormal. In these knees, there is a large increase in anterior tibial translation and the pivot shift test is in the grade III category.
The function of the PMC/POL in resisting internal tibial rotation is shown in Figure 24-6. An increase in the internal rotation limit at low flexion angles is a further diagnostic test for PMC/POL rupture, detected by the dial test.
Sims and Jacobson44 reviewed 93 knees that underwent operative treatment for acute MCL injuries. These authors reported that 93% had associated injury to the POL following the description of Hughston and Eilers.22 The authors emphasized the importance of identification and repair of the POL and tears of the semimembranosus capsular attachment (present in 70% of knees) and associated peripheral detachment of the medial meniscus (present in 30% of knees; Fig. 24-7). The authors postulated that a dynamic function of the semimembranosus attachments exists for knee stability, but this is unproved experimentally. Although some authors describe rupture and surgical repair of the POL alone (anteromedial rotatory instability), the biomechanical data show that the POL is not a primary restraint for medial joint opening or external tibial rotation. Interestingly, an isolated POL injury does produce an increase in internal tibial rotation (see Fig. 24-6), although again, this injury pattern clinically involves a combined PCL/POL disruption.
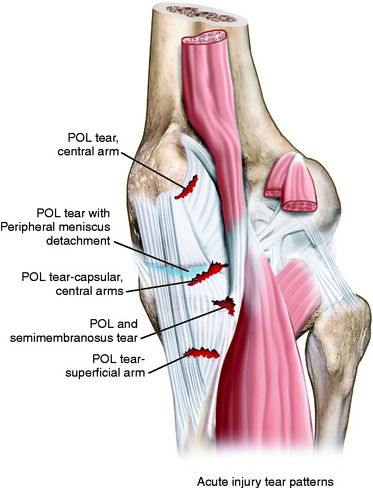
FIGURE 24-7 Three major injury patterns (injury to the POL is common to all): (1) injury to the POL with semimembranosus disruption, (2) injury to the POL with complete peripheral meniscocapsular detachment, and (3) POL injury with semimembranosus injury and peripheral meniscocapsular detachment. Disruption at any level is capable of disabling the dynamic function of the semimembranosus.44
CLINICAL EVALUATION
History and Physical Examination
The comprehensive examination of the knee joint required to detect all abnormalities includes assessment of (1) range of knee flexion and extension, (2) knee joint effusion and swelling, (3) the knee motion limits and subluxations compared with the contralateral knee,31 (4) alignment of the patellofemoral joint, (5) patellofemoral and tibiofemoral crepitus, (6) tenderness along the medial joint line and along the entire course of the SMCL from proximal to distal, (7) overall lower limb alignment, (8) neurovascular status, and (9) gait.
Diagnostic Clinical Tests
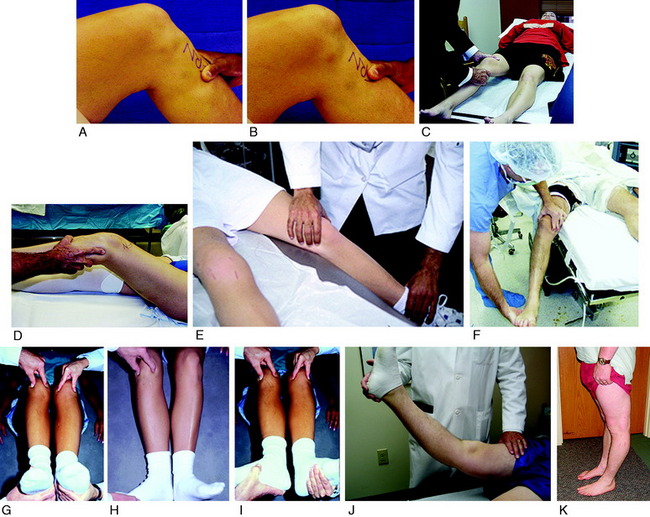
The clinical tests for the assessment of ligament injuries are shown in Figure 24-8. SMCL disruption is determined by manual valgus stress testing at 0° and 30° of knee flexion. The surgeon estimates the amount of joint opening (in millimeters) between the initial closed contact position and the open position of each tibiofemoral compartment (avoiding internal or external tibial rotation). The result is recorded according to the increase in the tibiofemoral compartment of the injured knee compared with that of the opposite normal knee.
Critical Points CLINICAL EVALUATION
The tibiofemoral rotation dial test at 30° and 90° with the patient in the supine position is done to determine whether increases in external tibial rotation occur with anterior subluxation of the medial tibial plateau (and not posterior subluxation of the lateral tibial plateau, indicating a posterolateral ligament injury).32 An increase in internal rotation may occur with MCL/POL disruptions (maximum 15°–45° flexion). Associated lateral and posterolateral disruptions are determined by varus stress testing at 0° and 30° of knee flexion.
Radiographs and Imaging Studies
Posterior stress radiographs are obtained in patients with PCL ruptures, especially those in whom the distinction of a partial versus complete PCL tear is difficult to determine on clinical examination (see Chapter 21, Posterior Cruciate Ligament: Diagnosis, Operative Techniques, and Clinical Outcomes).16 Lateral stress radiographs may be required in knees with lateral ligament injury (see Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes). Full standing radiographs of both lower extremities, from the femoral heads to the ankle joints, are done in knees with varus or valgus lower extremity malalignment (see Chapter 31, Primary, Double, and Triple Varus Knee Syndrome: Diagnosis, Operative Techniques, and Clinical Outcomes). The mechanical axis and weight-bearing line are measured.7 Of concern is to exclude a knee with lower extremity valgus alignment and increased medial soft tissue tensile forces with a valgus thrust, indicating the need for a corrective osteotomy in chronic medial injuries.
MRI is helpful to reveal the location of ligament anatomic disruptions, bone contusions, other ligament ruptures, and meniscus tears (Fig. 24-9). A high rate of concurrent lateral meniscus tears has been reported with MCL ruptures, making MRI an important adjunct for an accurate diagnosis.30,41 Ligament avulsion or osteochondral injuries requiring treatment within the initial 7- to 10-day period after injury may exist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree