Medial and Lateral Meniscus Transplantation: Arthroscopic-Assisted Techniques and Clinical Outcomes
Frank R. Noyes
Sue D. Barber-Westin
The meniscus provides important functions in the human knee, including load bearing, shock absorption, stability, and joint nutrition, that are vital for the integrity of the articular cartilage. While many meniscus tears can be successfully repaired, including complex tears that extend into the central avascular region (23), not all are salvageable, especially if considerable tissue damage has occurred. Transplantation of human menisci is hypothesized to restore partial load-bearing meniscus function, decrease patient symptoms, and provide chondroprotective effects (7,15,27). However, the procedure remains in an evolving state, as investigations of tissue-processing, secondary sterilization, and long-term function continue to evaluate its effectiveness. The optimal candidate is a young patient who has had a total meniscectomy and has pain and mild articular cartilage deterioration in the involved tibiofemoral compartment. There are few treatment options for these individuals and the goal of meniscal transplantation in the short term is to decrease pain, increase knee function, allow pain-free activities of daily living, and delay the onset of tibiofemoral arthrosis.
INDICATIONS/CONTRAINDICATIONS
The indications for a meniscus allograft are:
Prior meniscectomy
Age of 50 years or less
Pain in the meniscectomized tibiofemoral compartment
No radiographic evidence of advanced joint deterioration (≥2 mm of tibiofemoral joint space demonstrated on 45-degree weight-bearing posteroanterior radiographs [22] and no or only minimal bone exposed on tibiofemoral surfaces)
Normal axial alignment and a stable joint are required, as untreated abnormal limb alignment and anterior cruciate ligament (ACL) deficiency have correlated with a high rate of meniscus allograft failure in several studies. Axial correction is recommended in knees in which the weight-bearing line is less than 45% (varus) or greater than 55% (valgus), representing a 2- to 3-degree change from normal alignment. An osteochondral autograft transfer or autologous chondrocyte implantation may be required in knees with full-thickness articular cartilage defects in the meniscectomized tibiofemoral compartment, which may be done either during or before the meniscus transplant procedure. These cartilage procedures expand the indications for meniscus transplantation in knees with femoral articular cartilage defects.
Contraindications for a meniscus allograft are:
Advanced knee joint arthrosis with flattening of the femoral condyle, concavity of the tibial plateau, and osteophytes that prevent anatomic seating of the meniscus allograft (14)
Varus or valgus axial malalignment
Knee joint instability
Knee arthrofibrosis
Muscular atrophy
Prior joint infection
Symptomatic patellofemoral articular cartilage deterioration
Obesity (>30 body mass index)
We do not recommend a prophylactic meniscus transplantation after total meniscectomy in asymptomatic patients who do not have articular cartilage deterioration, as long-term predictable success rates are not available. In addition, the operative procedure does carry a slight risk for complications that could make the patient’s condition worse. There are sophisticated magnetic resonance imaging (MRI) techniques that are useful in determining the integrity of the articular cartilage and detect early deterioration prior to the onset of symptoms (20). A relative indication of meniscus transplantation is early (mild) arthritic deterioration in the involved tibiofemoral compartment in an asymptomatic patient.
PREOPERATIVE PLANNING
A thorough history is taken that includes assessment of prior operative records and current symptoms and functional limitations. The validated Cincinnati Knee Rating System (3) is used to rate pain, swelling, and giving-way of the knee as well as limitations with daily, athletic, and occupational activities. A comprehensive evaluation of the knee is conducted, which documents range of knee motion, joint effusion, tibiofemoral joint pain on palpation and during joint motion, and tibiofemoral joint crepitus. We also evaluate the patellofemoral joint, all knee ligaments, and gait abnormalities (17).
Diagnostic imaging includes bilateral anteroposterior radiographs in full extension, a 45-degree weight-bearing posteroanterior radiograph (22), and an axial view of the patellofemoral joint. The anteroposterior and lateral radiographs are taken with a magnification marker to obtain width and length measurements for the meniscus transplant (18). Axial lower limb alignment is measured using full standing hip-knee-ankle weight-bearing radiographs in knees that demonstrate varus or valgus alignment. MRI using fast-spin-echo techniques (19,20) are used in select cases to evaluate the condition of the articular cartilage and subchondral bone.
Selection of Meniscus Implant
A variety of sterilization techniques have been described for meniscus allografts, including none (fresh-frozen), irradiated, and cryopreserved, and no scientific data exist to select one type of graft processing method over another. Some authors advocate secondary sterilization using low-dose irradiation (1-2 Mrads) for purposes of bacterial sterilization (6). We recommend that allografts be obtained from tissue banks that have been accredited by the American Association of Tissue Banking and inspected by the Food and Drug Administration, where serological testing meets or exceeds the standards of these organizations (26). Importantly, donor selection criteria may vary between tissue banks, and the surgeon should understand the specific criteria used by the bank chosen to supply the transplant. Surgeons should also be aware that even though allograft tissues are generally processed aseptically, this may not prevent contamination and does not guarantee a sterile graft. We use prophylactic antibiotics intravenously before surgery and carefully monitor patients postoperatively for any signs of infection. The implications of different processing techniques on graft sterility is beyond the scope of this chapter, but have been discussed in detail by others (4,7,26).
We advise the surgeon to request that the tissue bank provide a photograph of the transplant that has been selected for the patient before surgery. A metric ruler should be placed adjacent to the transplant in the photograph to ensure that the allograft is of adequate size and width. Medial menisci may have a hypoplastic anterior horn that is narrow, inserting distal to the medial tibial surface (type III)(5); these menisci are not acceptable for implantation. The middle one third of a medial or lateral meniscus may be 8 to 10 mm in width and only suitable for small patients. The lateral meniscus may have reduced anteroposterior length, less than that calculated on the sagittal radiograph, and therefore not suitable for implantation.
SURGICAL TECHNIQUE
Transplant Preparation
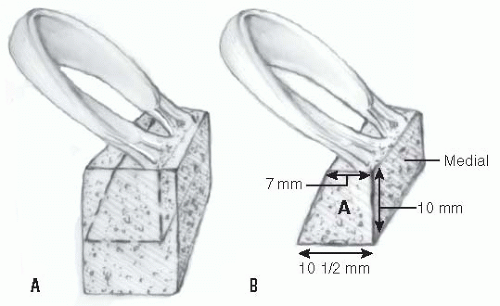
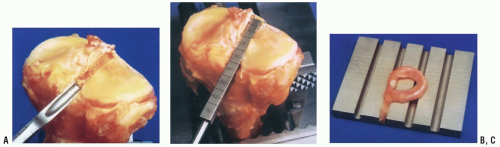
The meniscus is thawed, inspected, and prepared before administration of patient anesthesia because it is difficult to detect implant defects through the plastic packaging, and the meniscus must be thoroughly evaluated. For a lateral meniscus allograft, implant preparation is accomplished first to determine the depth and width required for the tibial slot for the central bone bridge technique. The central bone portion of the lateral meniscus transplant incorporates the anterior and posterior meniscal attachments and usually measures 8 mm wide in smaller patients and 9 mm in larger patients. The length of the bone attachment is usually 35 mm, but this can be altered as required. The posterior 8 to 10 mm of tibia bone that protrudes beyond the posterior horn attachment is removed to later produce a buttress against the bone slot in the host knee. Commercially available (Stryker Endoscopy Co., Kalamazoo, MI, and Cryolife Inc., Kennesaw, GA) sizing blocks and channel cutters are helpful for appropriate sizing. There is also a dove-tail technique that the surgeon may elect, which has the advantage of providing added stability to the fixation at the tibial bone portion of the transplant (Fig. 11-1). This procedure entails cutting a trapezoidal bone block which includes a narrow, 7-mm bone bridge that preserves the ACL tibial attachment site.
Medial meniscus transplants are not prepared until it is determined if the central bone bridge technique (which is preferred) or the two-tunnel technique (separate anterior and posterior bone attachments and tunnels) will be performed, as we will describe in a following section.
It should be noted that the normal ACL tibia attachment site, or a planned ACL tibial graft tunnel, may compromise lateral or medial meniscus transplant tibial fixation in smaller patients who do not have sufficient width of the central tibial region to accommodate both the transplant and ACL tibial attachment or tunnel. Since it is not possible in these knees to use the central slot technique when an ACL reconstruction is to be performed concurrently, the two-tunnel procedure is selected for a medial meniscus transplant. More commonly, the two operations are staged by performing the ACL reconstruction first and the meniscus transplant procedure several months later.
Lateral Meniscus Transplantation
The patient is placed in a supine position on the operating room table with a tourniquet applied with a leg holder, and the table adjusted to allow 90 degrees of knee flexion. The opposite lower extremity
is placed in a thigh-high elastic stocking and is padded to maintain mild hip flexion to decrease tension on the femoral nerve. After examination under anesthesia, diagnostic arthroscopy is done to confirm the preoperative diagnosis and assess articular cartilage changes. A meniscus bed of 3 mm is retained when possible, except at the popliteal tendon region. In knees that require a cruciate ligment reconstruction, an arthroscopically assisted approach is used (11). The femoral and tibial tunnels are drilled, and the ligament graft is passed through the tunnels with femoral fixation done first, followed by the meniscal transplantation, and then tibial cruciate graft fixation. Performing ligament graft fixation at the tibia as the final step allows for maximum separation of the tibiofemoral joint during meniscal transplantation. This also prevents potential ligament fixation problems during the operation.
is placed in a thigh-high elastic stocking and is padded to maintain mild hip flexion to decrease tension on the femoral nerve. After examination under anesthesia, diagnostic arthroscopy is done to confirm the preoperative diagnosis and assess articular cartilage changes. A meniscus bed of 3 mm is retained when possible, except at the popliteal tendon region. In knees that require a cruciate ligment reconstruction, an arthroscopically assisted approach is used (11). The femoral and tibial tunnels are drilled, and the ligament graft is passed through the tunnels with femoral fixation done first, followed by the meniscal transplantation, and then tibial cruciate graft fixation. Performing ligament graft fixation at the tibia as the final step allows for maximum separation of the tibiofemoral joint during meniscal transplantation. This also prevents potential ligament fixation problems during the operation.
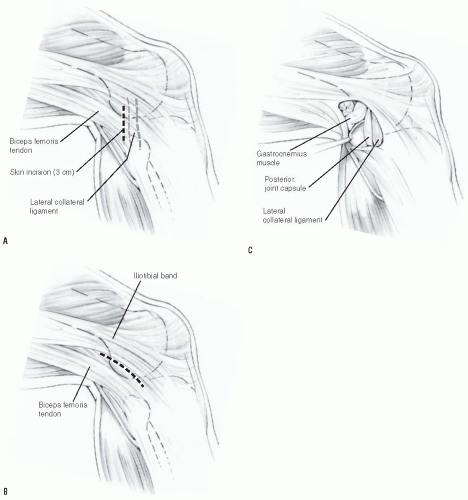
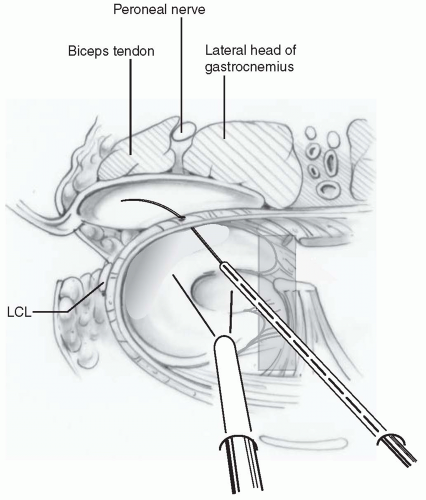
The tourniquet is inflated only for the two operative approaches. A limited 3-cm lateral arthrotomy is made just adjacent to the patellar tendon. Although arthroscopic techniques are available to prepare the tibial slot, we believe the limited arthrotomy provides superior visualization and avoids incising into the patellar tendon, which must be displaced medially to properly place the tibial slot. A common mistake involves placing the central tibial slot lateral to the normal attachment of the anterior horn of the lateral meniscus. A second 3-cm posterolateral incision is made just behind the lateral collateral ligament (Fig. 11-2) (10,24). The interval between the short head of the biceps muscle and the iliotibial band is identified and incised. The lateral head of the gastrocnemius is gently dissected with Metzenbaum scissors off the posterior capsule at the joint line just above the fibular head. Care is taken at this point, as dissection that extends too far proximal to the joint line at the posterolateral aspect would enter the joint capsule. If this occurs, a capsular repair is required to maintain joint integrity during the inside-out meniscal repair procedure. The inferior lateral geniculate artery, also in close proximity, is identified and preserved. The space between the posterolateral capsule and the lateral head of the gastrocnemius is further developed bluntly. An appropriately sized popliteal retractor (Stryker Co., Kalamazoo, MI) is placed directly behind the lateral meniscus bed and anterior to the lateral gastrocnemius muscle.
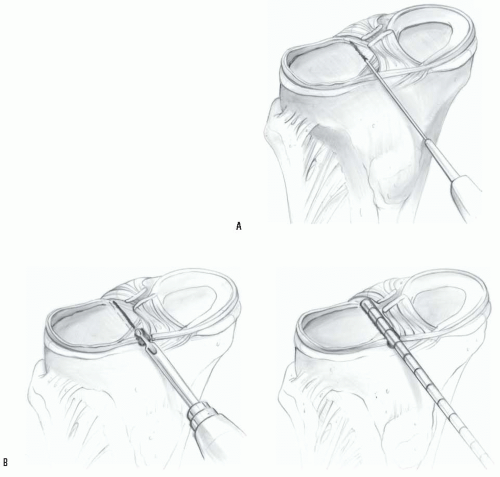
The width of the transplant is determined, and a template made out of aluminum foil of the same width and length is cut and inserted into the lateral compartment to determine the proper placement of the bone slot. This sizing step is important to ensure there is no lateral overhang of the meniscal body produced by not placing the bone far enough medially. A rectangular bone slot is prepared at the anterior and posterior meniscus tibial attachment sites to match the dimensions of the prepared transplant. The sequence of steps to prepare the lateral tibial slot is shown in Figure 11-3. The tibial
bone slot is 1 to 2 mm wider than the transplant to facilitate implantation. The anterior and posterior horns of the implant are placed into their normal attachment locations, adjacent to the ACL.
bone slot is 1 to 2 mm wider than the transplant to facilitate implantation. The anterior and posterior horns of the implant are placed into their normal attachment locations, adjacent to the ACL.
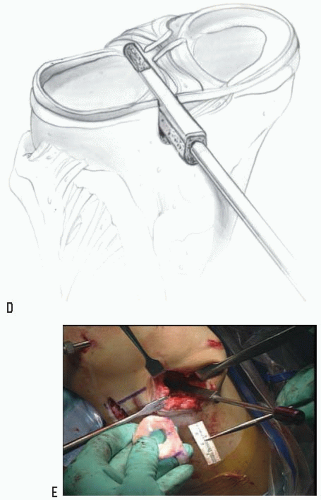
An alternative technique uses a starter chisel and finishing chisels to fashion the tibial slot to its final depth and width (Fig. 11-4A). A tibial slot sizing guide is used to check the length and depth (Fig. 11-4B). The allograft sizing block (Fig. 11-4C) confirms that the allograft bone bridge is of the correct width and depth.
The implant is inserted into the slot (Fig. 11-3E), and the bone portion of the graft is seated against the posterior bone buttress to achieve correct anterior-to-posterior placement of the attachment sites. A vertical suture in the posterior meniscus body is passed posteriorly to provide tension and facilitate implant placement and is later tied. The knee is flexed, extended, and rotated to confirm correct placement of the transplant has been obtained. Sutures are placed into the anterior one third of the meniscus, attaching it to the prepared meniscus rim under direct visualization.
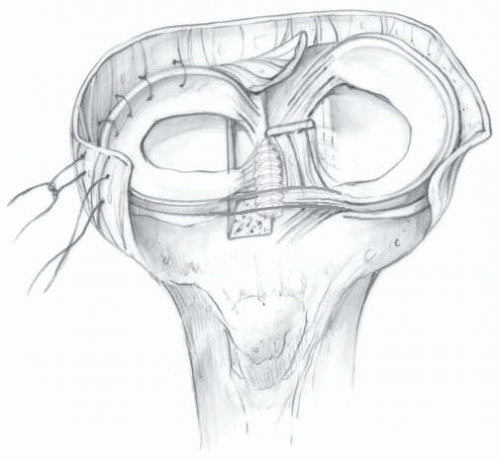
Two fixation methods are available for the central bone attachment. Two 2-0 nonabsorbable sutures (Ticron, Davis and Beck Co., Wayne, NJ, or Ethibond, Ethicon Inc., Somerville, NJ) may be placed over the central bone bridge, brought through a drill hole, and tied to a tibial post. We prefer to place an interference screw (7 × 25 mm, comprised of an absorbable composite material) adjacent medially to the bone bridge (8). A tap is inserted over the guidewire to create a path for the interference screw with the bone bridge held in place manually. The arthrotomy is closed, and the inside-out meniscal repair is completed with multiple vertical divergent sutures, which are placed first superiorly to reduce the meniscus (Fig. 11-5), and then inferiorly in the outer one third of the implant. Sutures are not placed in the middle and inner thirds of the meniscus to avoid weakening the implant due to its limited healing capability in these regions (Fig. 11-6).
Medial Meniscus Transplantation
The patient is placed in a supine position on the operating room table with a tourniquet applied with a leg holder, and the table adjusted to allow 90 degrees of knee flexion. The opposite lower extremity
is placed in a thigh-high elastic stocking and is padded to maintain mild hip flexion (to decrease tension on the femoral nerve). After examination with the patient under anesthesia, diagnostic arthroscopy is done to confirm the preoperative diagnosis and assess articular cartilage changes.
is placed in a thigh-high elastic stocking and is padded to maintain mild hip flexion (to decrease tension on the femoral nerve). After examination with the patient under anesthesia, diagnostic arthroscopy is done to confirm the preoperative diagnosis and assess articular cartilage changes.
The tourniquet is inflated only for the anteromedial and posteromedial surgical approaches. A 4-cm skin anteromedial incision is made adjacent to the tibial tubercle and patellar tendon. A second 3-cm vertical posteromedial incision is made, similar to that described for inside-out meniscus repairs (10) (Fig. 11-7




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree