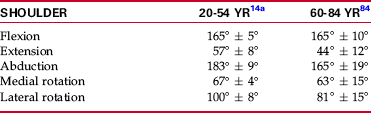
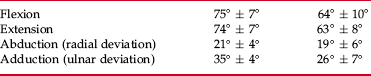
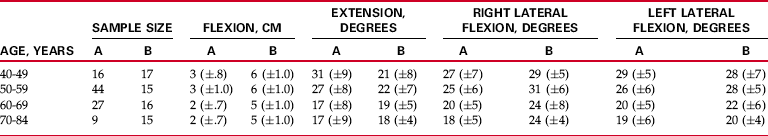
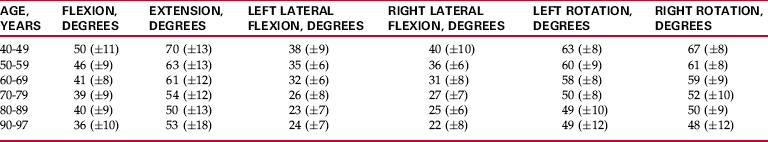
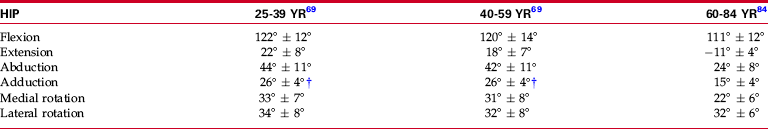
Chapter 2 Chapter 1 introduced the background necessary to measure joint range of motion (ROM) and muscle length using standardized procedures. The purpose of this chapter is to educate the individual who is collecting data on ROM and muscle length regarding the meaning of that information. The clinician must be aware of the strengths and weaknesses of referring to data as “normative.” The reader needs to understand both the changes that occur with age and the differences that exist between men and women, as well as among different cultures. In addition, changes that occur as a result of participation in athletic activities are important to understand. Finally, if measurements are not accurate, then the information gained from collected data is literally worthless. The clinician not only must be aware of the need for accurate measurements, but also must have an understanding of the reliability and validity of the procedures and instruments that are being used. After reading Chapter 2, readers should have a better understanding of the clinical relevance of the data collected in measuring ROM and muscle length to better educate their patients and to guide their intervention. Numerous individuals and groups have provided “norms” for ROM of the joints of the spine and extremities (see Appendix B). However, the validity of most of these “norms” is suspect for one reason or another. Many individuals and groups who have provided “norms” for ROM have done so without substantiating the source of the “normative” data. For example, the long-used and accepted “norms” for ROM provided by the American Academy of Orthopaedic Surgeons (AAOS)4 were published without an explanation of how the data were obtained or any description of the population from which the data came. The newest edition of the AAOS joint motion manual repeats many of the 1965 “norms” and provides other normative data that are derived from studies with small or nonrandomized samples.35 Likewise, the American Medical Association (AMA) does not describe the source for its published “norms” for ROM.5 Instead of providing unsubstantiated normative data for the various movements, Appendix B attempts to provide “norms” for ROM for movements of the extremities and the spine that are based on available published literature. CHANGES IN RANGE OF MOTION WITH AGE Table 2-1 reports ROM of the lower extremity in the elderly population. A significant decrease in the amount of hip motion (abduction, adduction, medial rotation, and lateral rotation) was reported in male and female subjects aged 60 to 84 years as compared with mean values reported for younger adults (see Table 2-1).69,84 Similar results indicating a progressive decrease in hip ROM in 77 male subjects as they aged from 15 to 73 years was reported by Nonaka et al.59 Table 2-1 Changes in Lower Extremity Range of Motion: 25 to 84 Years of Age †From Boone DC, Azen SP: Normal range of motion of joints in male subjects. J Bone Jt Surg 1979;61:756-759. However, these reported decreases in ROM in the hip joints of older adults were not substantiated by Roach and Miles,69 who reported on data from the first National Health and Nutrition Examination Survey (NHANES I). In their analysis of 1313 of the original 1892 subjects (aged 25 to 74 years) on whom hip and knee range-of-motion measurements were taken as part of NHANES I, Roach and Miles69 reported that, generally, differences in mean ROM between younger (aged 25 to 39) and older (aged 60 to 74) age groups were small, ranging from 3 to 5 degrees. The only motion of the hip that did appear to decrease in range with aging, according to Roach and Miles,69 was hip extension, which showed a greater than 20% decline between the youngest (aged 25 to 39 years) and oldest (aged 60 to 74 years) age groups. The apparent discrepancy in reported results between the study by Walker et al84 and the Roach and Miles69 study may have been due to differences in the age groups studied. The sample population in the Walker et al84 study included subjects with ages up to 84 years, whereas no subjects over the age of 74 were included in the data reported by Roach and Miles.69 A more recent study by Nonaka et al59 supported the findings of the Walker et al group.84 Additionally in a study that focused on subjects between the ages of 70 and 92 years, James and Parker41 reported progressive decreases in all lower extremity joint motions with increasing age, with the most pronounced decreases in motion occurring after age 80. The largest changes in ROM occurred with ankle dorsiflexion (knee extended) and hip abduction. Thus one could presume, by analyzing the aforementioned studies, that lower extremity ROM does show a decline with increasing age, but that that decline is probably not significant until the ninth decade. Some motions of the lower extremities have been reported to decline in range at earlier ages. Decreased ROM of the first metatarsophalangeal joint after age 45 has been reported both for flexion and for extension of that joint.18 Loss of extension ROM appears to be both more marked and more significant in terms of potential loss of function.18 Decreases in upper extremity ROM in older adults have been reported (Table 2-2). Walker et al84 reported a significant decrease in the amount of shoulder and wrist extension that occurs in older males only, and a decrease in the amount of forearm supination was observed in older females, compared with mean values reported for all motions by the AAOS.35 Statistically significant decreases with increasing age were reported for wrist flexion, wrist extension, and shoulder rotation ROM in a group of 720 subjects, aged 33 to 70 years.3 These subjects represented a subgroup of a population surveyed in Iceland and Sweden. Decreases in other upper extremity motions (shoulder flexion, abduction, medial rotation, and lateral rotation) were reported by Downey et al28 in a group of 106 subjects aged 61 to 93 years. However, these decreases were based on comparison with means published by the AAOS in 1965, many of which have since changed. Comparison of values obtained by Downey et al28 versus current AAOS means35 reveals decreases only in shoulder abduction and lateral rotation in the group of older subjects. This decrease in shoulder abduction with increased age was supported by a study by Bassey et al,10 who examined 894 subjects over the age of 65 (529 females, 365 males). Results indicated that the mean values for shoulder abduction were significantly lower for subjects over 75 years of age (n = 432) than for the younger group, which ranged in age from 65 to 75 years (n = 462). After examining 40 subjects (20 male, 20 female) in each of the following age groups—0-10, 11-20, 21-30, 31-40, 41-50, 51-60, and 61-70 years, Barnes et al9 reported that shoulder flexion, abduction, extension, and lateral rotation decreased with age. The authors were surprised to find that internal rotation increased with age. Similar to the study by Downey et al,28 the largest decrease in ROM per year occurred in shoulder abduction and lateral rotation. An investigation by van Adrichem and van der Korst82 examined the changes that occur as children age from 6 to 18 years. Using a tape measure, the authors measured lumbar flexion in 248 children and reported that as the child became older and progressed to adulthood, flexion ROM increased. After investigating differences in lumbar ROM in 405 healthy subjects (196 female, 209 males) ranging in age from 16 to 90 years, Troke et al80 reported that lumbar ROM declined in a linear fashion as age increased. Declines in ROM were 40% to 42% for flexion, 76% for extension, and 43% for lateral flexion. However, the author reported no change in lumbar rotation with increasing age. Results presented by Troke et al80 were supported by several studies30,33,49,54,56,77,83 that examined lumbar ROM across the age span by categorizing subjects into 10-year increments and comparing the amount of lumbar motion in each age group. In one of the earliest studies, Loebl49 used an inclinometer to measure lumbar flexion and extension in 176 individuals between the ages of 15 and 84 years and reported that a decrease in ROM was “readily demonstrated.” Similarly, Moll and Wright56 used the tape measure technique to measure flexion, extension, and lateral flexion in 237 subjects (aged 18 to 71 years) and reported that an initial increase in lumbar motion occurred from the age 15-to-24 decade to the age 25-to-34 decade, followed by “a progressive decrease in advancing age.” Sullivan et al77 used double inclinometry to measure flexion and extension in 1126 healthy volunteers and reported that “flexion and extension declined as age increased.” These results were supported by van Herp et al,83 who used a computerized three-dimensional (3D) system to examine lumbar flexion, extension, lateral flexion, and rotation in 100 subjects with ages ranging from 20 to 77 years. The author found a consistent reduction in motion with each decade of life and reported that “a clear trend of reducing motion with age in both male and female is apparent.” Also using a computerized system to measure lumbar flexion, extension, lateral flexion, and rotation, McGregor et al54 examined 203 subjects. Results indicated that age had “an influence on motion with a gradual reduction seen with each decade.” After examining flexion (using a tape measure), extension (using a goniometer), and lateral flexion (using a goniometer) in 172 primarily male subjects (only four subjects were female) between the ages of 20 and 82 years, Fitzgerald et al33 reported that lumbar motion decreased across the age span, with the difference being statistically significant at 20-year intervals. In reporting similar results after measuring flexion (with a tape measure), extension (with a goniometer), and lateral flexion (with a goniometer) in 109 females, Einkauf et al30 described significant differences between the two youngest decades (ages 20 to 29 and ages 30 to 39) and the two oldest decades (ages 60 to 69 and ages 70 to 84). Additionally, Einkauf et al30 reported that extension showed the greatest decrease in motion with increasing age. Table 2-3 provides information on normative data related to lumbar ROM with increased age derived from the research by Fitzgerald et al33 and Einkauf et al.30 Although inconsistencies related to the effects of aging on joint ROM in other joints may exist, agreement is noted in the literature that ROM of the cervical spine decreases in aging adults. Using an inclinometer attached by straps to the head and under the chin, Kuhlman45 compared a group of 20- to 30-year-old subjects (n = 31) with a group of 70- to 90-year-old individuals (n = 42) for cervical flexion, extension, lateral flexion (right and left measured separately), and rotation (right and left measured separately). The authors reported that “the elderly group had significantly less motion than the younger group for all six motions measured.” Furthermore, the authors reported that the loss of motion was greatest for cervical extension and least for cervical flexion.45 A review of the literature revealed several studies that supported the conclusions reported by Kuhlman.45 Five studies used the cervical range of motion (CROM) device to examine the changes in cervical motion that occur with age. Examining combined flexion/extension, combined right/left lateral flexion, and combined right/left rotation in 90 subjects with an age range of 21 to 60 years, Nilsson58 reported that results revealed “significant differences between ROM in different age groups for all directions of movement, in the sense that ROM decreased with increasing age.” After examining change with age in 84 subjects ranging in age from 20 to 69 years, Hole et al40 reported that cervical ROM in all planes decreased significantly, and “an individual can be expected to lose about 3.8 degrees and 6.9 degrees in cervical flexion and extension, respectively, per decade.” Both Peolsson et al62 (101 subjects; aged 25 to 63 years) and Castro et al19 (157 subjects; aged 20 to 89 years) reported that cervical ROM decreased with increasing age. Furthermore, Peolsson et al62 reported similar results to the study by Kuhlman45 in that the decrease in ROM was most pronounced in extension. Also using the CROM to examine cervical flexion, extension, lateral flexion, and rotation in subjects categorized in 10-year increments across eight decades, Youdas et al85 examined 337 individuals ranging in age from 11 to 97 years. The authors concluded that males and females should expect a loss of 3 to 5 degrees for all cervical ranges of motion per 10-year increase in age—similar to the amount of loss of motion reported by Hole et al.40 Table 2-4 provides the only published data on normative ranges of motion related to cervical motion with increased age. Two studies in which similar 3D devices were used to measure cervical ROM also divided subjects into categories of 10-year intervals. Examining 150 subjects for combined flexion/extension, combined right/left lateral flexion, and combined right/left rotation from age 20 to “older than 60 years,” Dvorak et al29 reported that ROM decreased as age increased, “with the most dramatic decrease in ROM occurring between the 30-39th and 40-49th decades.” Similarly, Trott et al81 examined cervical flexion, extension, lateral flexion (right and left measured separately), and rotation (right and left measured separately) in 120 subjects aged 20 to 59 years and reported that “age had a significant effect on all the primary movements.” Grouping subjects ranging in age from 12 to 79 years into seven groups by age using 10-year increments (n = 70), Lind et al48 reported that radiographic examination indicated that “the motion in all three planes (flexion/extension, lateral flexion, and rotation) decreased with age.” This decrease was significant and began in the third decade. Additionally, results reported by Lind et al48 were consistent with a report by Kuhlman45 that “in the sagittal plane, extension motion decreased more than motion in flexion.” An investigation by Mayer et al52 was the only study to report that no age-related differences occurred in the measurement of cervical flexion, extension, lateral flexion (right and left measured separately), and rotation (right and left measured separately) when a double-inclinometer method was used. However, a review of the study’s procedures indicated that the authors compared the youngest 50% of subjects with the oldest 50% of subjects (n = 58). Although the age range of subjects was reported as 17 to 62 years, no data were provided as to the mean age of each group. Therefore, the mean age of each group compared in this study is unknown, and any conclusions of this study are unclear.52 Thurnwald79 evaluated active ROM of the temporomandibular joint (TMJ) in 100 asymptomatic subjects with calipers. In comparing a group of 50 (25 male, 25 female) subjects aged 17 to 25 years versus 50 subjects (equal numbers of males and females) aged 50 to 65 years, the author reported that the older group had a significant decrease in ROM for mandible depression, protraction, right lateral deviation, and left lateral deviation. The author concluded that the TMJ “behaves in a similar manner to other synovial joints with increasing age.” Mezitis et al55 also compared the effects of age on mouth opening in 1100 healthy adults (500 male, 600 female) between the ages of 18 and 70 years. After dividing subjects into age groups by decade between the ages of 20 and 70, the authors reported that the significantly greatest maximal opening was seen in those of younger age, whereas the significantly smallest maximal opening was recorded in those of older age. The amount of ROM present in the joints of males and females appears to differ, but not with respect to all joints. However, in almost all cases cited, the greater ROM is found in the female population. Bell and Hoshizazki12 compared 124 females to 66 males ranging in age from 18 to 88 years for differences in ROM at 17 joint actions at the hip, knee, and ankle and reported that “females have greater range of motion in joint action than their males counterparts throughout life.” In a study of 60 college-age subjects in which the influences of hip position and gender on hip rotation were investigated, females demonstrated a statistically greater range of active hip medial and lateral rotation compared with males.74 Similar differences between the sexes regarding the range of available hip rotation were reported by James and Parker41 in a sample of elderly (ages 70 to 92) males and females. Increased medial, but not lateral, hip rotation in females also has been reported by Walker et al84 in a study of 60 male and female subjects aged 60 to 84 years, and in a study by Svenningsen et al,78 who studied 761 Norwegian subjects ranging in age from 4 years to adulthood (the 20s). Other motions of the hip that have been reported as being increased in females compared with males are hip flexion in adolescents, young adults,78 and elderly females (aged 70 to 92 years)41 and hip abduction in all age groups from 4 years to young adulthood.78 Two studies of older adults41,84 have reported a statistically increased range of knee flexion in female compared with male subjects. However, in one study, the difference did not exceed the inter-rater error for that measurement.84 A greater amount of ankle plantarflexion also appears to be present in women compared with men across all adult age groups.41,57,84 Conversely, there appears to be some indication that ankle dorsiflexion ROM becomes significantly greater in males than in females among persons older than 70 years.57 Some motions of the upper extremity also appear to differ according to sex. Barnes and colleagues9 examined 280 subjects between the ages of 4 and 70 years and found that female subjects had a greater shoulder ROM than men at all ages, with the greatest difference occurring in abduction and medial and lateral rotation.9 In a study of 720 adult subjects from Sweden and Iceland,2 significantly greater ranges of shoulder medial and lateral rotation were reported in females compared with males. These differences in shoulder lateral, but not medial, rotation were substantiated in a group of older male and female subjects.84 Additionally, the older female subjects, who were between the ages of 60 and 84 years, demonstrated significantly more shoulder flexion, extension, and abduction than did their male counterparts.84 In contrast, in a study of 894 subjects over the age of 65 in which shoulder abduction was measured, results revealed that females had less shoulder ROM than men.10 In the sample presented, about 50% of subjects were over the age of 78, and the authors speculated that functional use of the shoulder may have differed between males and females, with older males possessing increased function and therefore increased ROM compared with females.10 Differences in elbow ROM between male and female subjects have been demonstrated in older adults in two studies. These studies examined similar age groups (55 to 84 years compared with 60 to 84 years), and both demonstrated a significantly increased amount of elbow flexion in female compared with male subjects.75,84 One study also reported a significantly greater amount of elbow extension in female subjects.84 Wrist and hand motions also appear to differ in male compared with female subjects. Allander et al3 reported significantly higher ranges of wrist flexion and extension in female than in male adults. Increased wrist extension and adduction (ulnar deviation) in females, but not increased wrist flexion, were reported in a sample of older adults.84 In a study of 120 young adults (aged 18 to 35 years), Mallon et al51 demonstrated increased active and passive extension at all joints of the fingers (metacarpophalangeal, proximal interphalangeal, and distal interphalangeal) in female subjects compared with males. Details of studies undertaken to investigate differences in ROM according to sex are found in Appendix B. Only two studies have investigated the differences between males and females in ROM of the lumbar spine before adulthood. Using a tape measure to measure flexion and lateral flexion, Haley et a136 compared 142 females versus 140 males between the ages of 5 and 9 years and reported that girls were significantly more flexible than boys. Conversely, van Adrichem and van der Korst82 used a tape measure to measure lumbar flexion in children between the ages of 6 and 18 years and reported that no significant difference was discerned between boys (n = 149) and girls (n = 149). Differences in lumbar ROM between the sexes in older subjects remains unclear. Macrae and Wright50 also used a tape measure to measure lumbar flexion, but in an older (aged 18 to 71 years) sample of 195 females and 147 males. The authors reported that, regardless of age, males had significantly greater lumbar flexion than females. This result of males possessing greater lumbar flexion (and extension) ROM than females was supported by McGregor et al54 (103 males vs. 100 females; aged 20 to 70 years) and Troke et al80 (196 females, 209 males; aged 16 to 90 years) for young subjects. However, both of these studies reported that with increased age, no difference in lumbar ROM was noted between the sexes. Greater flexion in males than in females was supported in a later study by Moll and Wright,56 who compared the differences between 119 males and 118 females, also using a tape measure. In addition, Moll and Wright56 reported that males had greater lumbar mobility than females for extension, but that females had greater motion for lateral flexion than males. The opposite was reported by Sullivan et al,77 who, after comparing flexion and extension in 686 males and 440 females between the ages of 15 and 65 years, reported that males had greater flexion ROM than females, and that females had greater extension ROM than males. In contrast, when comparing lumbar ROM in 50 males and 50 females ranging in age from 20 to 60 years, van Herp et al83 reported “consistently greater flexibility in males than in females throughout the age range” and in all movements. When examining the differences in lumbar rotation related to sex, Boline et al14 compared the amount of lumbar rotation in 14 males with the amount of rotation in 11 females and reported that no significant difference existed between males and females in terms of right and left rotation. This equality of lumbar rotation between the sexes at all ages was supported in the study by Troke et al.80
MEASUREMENT of RANGE of MOTION and MUSCLE LENGTH
CLINICAL RELEVANCE
NORMATIVE DATA FOR RANGE OF MOTION AND MUSCLE LENGTH
FACTORS AFFECTING RANGE OF MOTION
Lower Extremity


Upper Extremity
Lumbar Spine
Cervical Spine and Temporomandibular Joint
DIFFERENCES IN RANGE OF MOTION BASED ON SEX
Upper Extremity
Lumbar Spine
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


MEASUREMENT of RANGE of MOTION and MUSCLE LENGTH: CLINICAL RELEVANCE