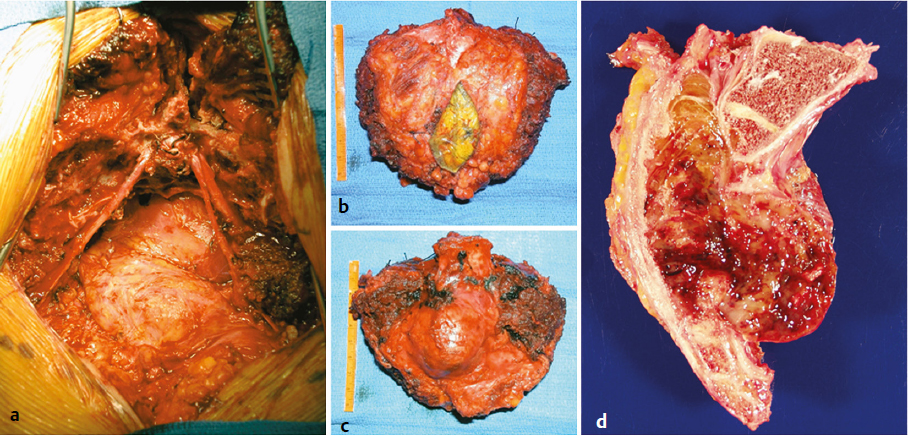
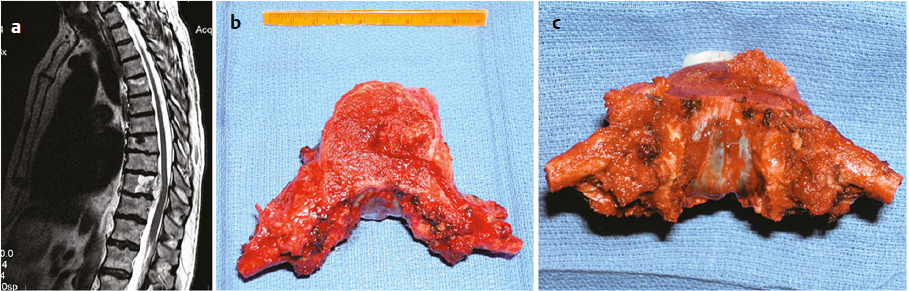
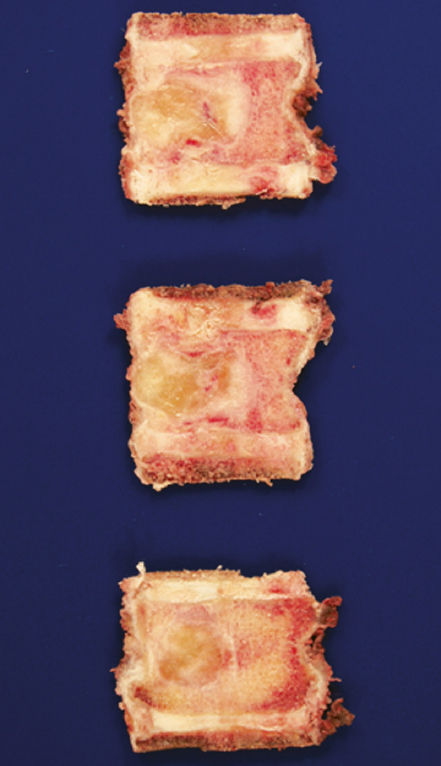
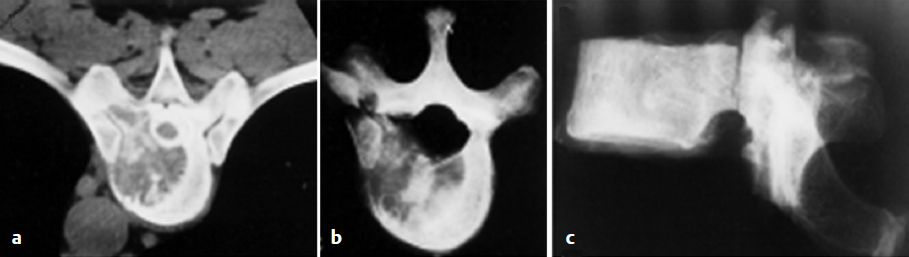
11 Cure, or long-term local control, represents the primary goal in the treatment of primary tumors. Various staging systems were developed in order to facilitate prognostication of the probability of cure and survival and to help direct treatment decisions. Physicians most commonly use the Enneking staging system when discussing primary musculoskeletal tumors.1 Because primary extradural tumors of the spine represent a subset of musculoskeletal tumors, the Enneking system and principles that were initially developed in the context of appendicular tumors have been applied to spinal tumors. Although spinal and appendicular tumors may be histologically identical, the anatomic challenges encountered in the spine distinguish the spinal tumors from their appendicular counterparts. The Weinstein-Boriani-Biagini (WBB) surgical system and the Tomita surgical classification of vertebral tumors were developed in order to facilitate the application of the Enneking concepts to the spine and to describe the specific vertebral elements that harbor the tumor and the extent of intra- and extraosseous extension.2,3 Based on the circumferential extent of the tumor and the amount of paraspinal and epidural extension, the systems help predict the margins that may be achieved during surgery. The surrounding structures, tissue planes, and associated neural elements change along the course of the spinal column; therefore, the safety and feasibility of attempting a resection of a clear surrounding margin or en-bloc excision also must be considered in the context of the specific tumor level. Thus, although amputation of a large portion of the sacrum with surrounding musculoskeletal structures and sacral nerve roots may result in minimal structural and neurologic compromise, higher amputation would generally be associated with profound neurologic deficits and require extensive reconstruction. How much margin should there be, and is a margin necessary, are frequent questions that arise with regard to spinal tumors. To answer this, an understanding of the definition of a margin is critical. Surgical margins in spinal surgery are defined by conventions adopted from the orthopedic extremity literature. But the terms in use are frequently misused, which has contaminated the spinal tumor surgical literature. In addition to understanding what the definition of a margin is, correlating the type of margin that is required with the pathology being treated is critical to delivering the appropriate treatment to a specific patient. Margins can be defined as positive, marginal, wide, and radical.1 A positive margin means that residual tumor remains within the patient. A marginal margin indicates that tumor comes up to the margin of the specimen, but it is contained within the capsule of the tumor. A wide margin indicates that a tumor has been excised and at least 1 cm of healthy tissue has been excised surrounding the tumor. A radical resection means that the tumor is removed and the entire compartment within which the tumor resides is also removed. The margin gives no information on how a surgical resection was undertaken; it only describes the resultant surgical bed. Often, in spinal oncology, unfortunately, only marginal margins are surgically feasible. Resection of sacral chordomas, even with nerve sacrifice, and resection of soft tissues including skin, fat, and muscle, and planning an osteotomy rostral to the extent of tumor usually still results in a marginal margin. It is rare that sacral chordomas do not have ventral extension of the tumor into the pelvis behind the rectum. In most cases, the tumor capsule is preserved at this margin, but the resection margin is at the mesorectum. Without resection of the rectum, sacral chordoma resections are marginal at the ventral margin or the mesorectum (Fig. 11.1). Patients with mobile spine osseous tumors typically present with epidural extension. In this situation, without dural resection, the best margin will be a marginal margin at the tumor capsule along the dura (Fig. 11.2). Wide margin resections are possible with spinal tumors in rare situations. Some patients may present with small tumors completely contained within the vertebral body (Fig. 11.3), and, in these situations, complete resection of the vertebral body with the tumor can result in a wide margin. Fig. 11.1a–d A large sacral chordoma with ventral extraosseous extension. (a) The postoperative surgical field demonstrates the proximity of the tumor to the intrapelvic organs. (b) Posterior view of the specimen demonstrates the wide margin of healthy tissue, which can be obtained. On the other hand, the anterior (c) and lateral (d) views of the specimen show a marginal margin at the site of ventral extraosseous extension of the tumor. (Courtesy of Jean-Paul Wolinsky, MD.) Radical resections of the spine are technically possible but are not performed. A radical resection requires resection of the tumor and the entire compartment within which the tumor lies. In an extremity tumor, this would involve resection of the tumor, the bone from which it arises, and the muscles inserting into the bone through their distal insertions. An example would be a tumor arising in the tibia, with a planned resection being an above-the-knee amputation, above the muscular insertions of the muscles surrounding the tumor. In the spine, a conceivable example would be a sacral tumor, contained within the sacrum, with no ventral extension through the sacrum, and no extension of the tumor to the dura, where a hemicorporectomy is performed. This operation would most likely never be proposed for such tumor architecture, irrespective of the pathology, as the morbidity of the operation would be unacceptable. With extension of the tumor to the dura, a radical resection, even with a hemicorporectomy would not be possible, as resection of the dural “compartment”, would require resection of the dura throughout the entire spine and cranium. Fig. 11.2a–c (a) Sagittal T2-weighted magnetic resonance imaging (MRI) of a T10 chordoma with epidural extension. Superior (b) and posterior (c) views of the vertebrectomy specimen demonstrate that only a marginal margin was obtained due to the dorsal extension of the tumor into the epidural space, with tumor displacing the posterior longitudinal ligament. (Courtesy of Jean-Paul Wolinsky, MD.) Fig. 11.3 A malignant peripheral nerve sheath tumor entirely confined to the vertebral body without extraosseous extension. This tumor was resected with a wide margin of bone. (Courtesy of Jean-Paul Wolinsky, MD.) The Spine Oncology Study Group evaluated the reliability of the application of the Enneking and WBB staging systems in the spine using a series of primary tumor case examples.4 Moderate interobserver reliability was demonstrated in the use of the Enneking staging system, an Enneking-recommended surgical margin, the WBB layers, and the WBB-recommended resection. The intraobserver reliability was near-perfect for the Enneking staging system and substantial for the WBB system. The Enneking tumor extent determination proved particularly challenging, with only slight to fair interobserver reliability. A multicenter cohort study examined the correlation between the ability to achieve an Enneking-recommended margin and the outcome of surgery for primary osseous tumors of the spine.5 Patients harboring tumors that were amenable to resection with the margin that is recommended by the Enneking staging system had significantly lower local recurrence rates compared with patients in whom an optimal margin could not be achieved. However, we must emphasize that the resectability of the tumor with an appropriate margin is largely an intrinsic characteristic associated with the individual histology, grade, location, and size. This is supported by the observation that in the study cohort, the Enneking-recommended margin could not be achieved in a significant majority of high-grade tumors and tumors located in the cervical and thoracic spine, but could be achieved in a significant majority of benign tumors and tumors located in the sacrum. Furthermore, the risk of blood loss of more than 5,000 mL and the risk of infection were significantly higher in patients who underwent surgery for Enneking-recommended margins. Further complicating the literature is the misuse of the terms spondylectomy, en-bloc spondylectomy, total en-bloc spondylectomy (TES), intralesional, and en-bloc resection. Spondylectomy means removing the entire segment of the spine (the vertebral body, pedicles, superior and inferior articulating processes, pars, transverse processes, lamina, and spinous process) (Fig. 11.4). It is a surgical technique, but does not specify if the tumor is removed in an en-bloc or intralesional fashion. An entire spinal segment can be removed “piecemeal” and result in a spondylectomy, but this should not be confused with an en-bloc resection. The terms en-bloc spondylectomy and total en-bloc spondylectomy (TES) are frequently used in the primary tumor literature,6 but in the mobile spine they are seldom, if ever, performed. An en-bloc spondylectomy would require resection of the spinal segment without violating any portion of it. Because each spinal segment of the mobile spine contains the spinal cord or the cauda equina, removal of the vertebra without opening of the spinal canal ring would require transection of these neural elements with the specimen. This does occur in the sacrum, when sacral amputations are performed, as the sacrifice of nerves roots in this region is usually undertaken to achieve a meaningful resection.7 The term intralesional resection should be used anytime the tumor capsule is violated and the tumor is entered. Even if the intent of the tumor resection is to remove the entire specimen in one piece, if the specimen demonstrates that the margin was violated on pathological review, then this is an intralesional resection. If a surgery plan incorporates the need for a planned transgression of the tumor8 (Fig. 11.5) in order to achieve a resection, this is, by definition, an intralesional resection despite complete removal of the tumor. The term en bloc is used if the tumor is removed in one piece without violation of the tumor margin. Certain tumor pathologies require en-bloc resections with negative margins to achieve local tumor control. In certain circumstances, an en-bloc resection might be used to control blood loss in vascular tumors even if the tumor pathology does not require an en-bloc resection for tumor control. Likewise, an en-bloc resection may be employed to achieve a complete resection if the tumor and surrounding anatomy have become distorted, and the interpretation of tumor margins would be complicated by an intralesional resection. Fig. 11.5a–c (a) A computed tomography (CT) scan of a T10 solitary breast metastasis with invasion of the vertebral body, epidural space, pedicle, and the costovertebral joint. Horizontal (b) and lateral (c) radiographs of the specimen showing the intralesional resection of the tumor with intentional transgression of the pedicle with tumor invasion.10 (Reproduced with permission from Lippincott Williams & Wilkins.)
Margins in Spine Tumor Resection: How Much Is Enough? Is Planned Transgression Okay?

 Introduction
Introduction
 Margin Definition
Margin Definition
 Surgical Technique Terminology
Surgical Technique Terminology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree