Chapter 16 Manual Therapy in Sports Rehabilitation
OVERALL THERAPEUTIC AIMS
The place to start one’s understanding of the therapeutic potential of MT in sports rehabilitation is to identify the overall therapeutic aims.1 The ultimate goal is to assist two principal body processes:
Adaptation and its opposite dysfunctional adaptation can take many forms. One form is dysfunctional adaptation due to poor quality repair. Once the inflammatory phase is nearing completion, an adaptive remodeling process commences.2–6 This process is highly dependent on the stresses that are imposed on the tissue.7–11 A dysfunctional adaptation may ensue if, for any reason, the normal mechanical environment for repair is not provided. The most striking example is the atrophy seen when tissues are immobilized in a plaster cast.12–18 Such immobilization leads to muscle wasting, excessive connective tissue proliferation, and loss of sarcomeres in series resulting in general shortening.19–21 This change in the tissues is an adaptation process, albeit a dysfunctional one. The therapeutic aim under these circumstances is to create a “mechanical environment” in which the MT techniques and exercise provide the needed physical stimulation to “redirect” the adaptation process.
Adaptation and repair can also be seen in the motor system. Adaptation to physical experiences in the form of plasticity has been shown to occur throughout the neuromuscular continuum including the brain,18,22–31 spinal cord,32–35 motoneuron pools,36–38 and finally the servant of the nervous system—the muscle.39,40 Repair takes different forms in the nervous system depending on whether the system is damaged or intact. Structural repair of damaged neural tissue is seen in such conditions as head injuries.41–43 Another form of “functional repair” is seen in the nervous system following musculoskeletal injuries. In these conditions the nervous system is intact but associated with reorganization of motor control to protect the injured area.44 Repair can be viewed as a change from a dysfunctional motor pattern of injury to a normal function seen following full recovery. Postural instability often observed following ankle injury is an example of such dysfunctional motor pattern.45 In this condition functional training is known to assist the recovery of motor control from an injury state to a more functional state, resulting in stability improvements. In both the damaged and intact nervous system the therapeutic aim is to assist the transition of the neuromuscular system from a dysfunctional to a functional state. These conditions will require manual approaches that provide a particular physical environment in which neural repair and adaptation can take place.
The examples given earlier demonstrate that repair and adaptation are multidimensional processes, and to activate them different therapeutic approaches are necessary. Accordingly, the manual techniques used at each dimension and with each process will change dramatically. This brings up an important clinical question: If techniques change with each dimension and process, how does one choose which technique to use? This clinical conundrum can be resolved by using the Dimension Model of Manual Therapy.1 This useful model enables one to match the most effective MT techniques and the patient’s condition/process.
DIMENSIONAL MODEL OF MANUAL THERAPY
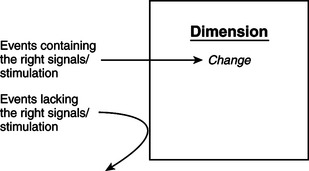
The dimensional model of MT is a practical tool for developing clinical strategies that allow one to maximize the efficacy of the therapeutic intervention. In this model, MT techniques and their effects can be described in three dimensions (Figure 16-1):
Figure 16-1 The dimensional model of manual therapy.
(Modified from Lederman E: The science and practice of manual therapy, ed 2, London, 2005, Churchill Livingstone.)
Tissue Dimension
Techniques that stimulate repair play an important role in the rehabilitation of sports injury. These techniques are often used in combination with “pump” techniques that aim to stimulate fluid flow. Together, these techniques impose positive mechanical stresses on the tissue necessary for regeneration and remodeling, as well as stimulating local fluid flow. Such effects on fluid dynamics may help tissue reperfusion, improve tissue nutrition (in time of increased metabolic needs),46 reduce swelling, and improve tissue washout of inflammatory byproducts. This could assist repair, as well as influence local pain mechanisms.
Improving fluid flow may also help ischemic musculoskeletal conditions often seen in sports, such as compartment syndromes,47 chronic myalgias,48,49 and nerve root irritation.50,51
Another common clinical presentation is reduced range of movement as a result of injury or long-term nontraumatic events, such as postural sets, patterns of behavior,52 sports,53 aging,54,55 and central nervous system damage.56–58 Accordingly, a large group of manual stretching techniques is aimed at improving tissue length and flexibility.
Neurological Dimension
These changes in the neurological dimension underlie a wide range of conditions both in the intact and damaged nervous systems.1 These can present as postural and movement dysfunction often associated with sports injuries, as well as conditions associated with central nervous damage, such as spinal cord and head trauma.
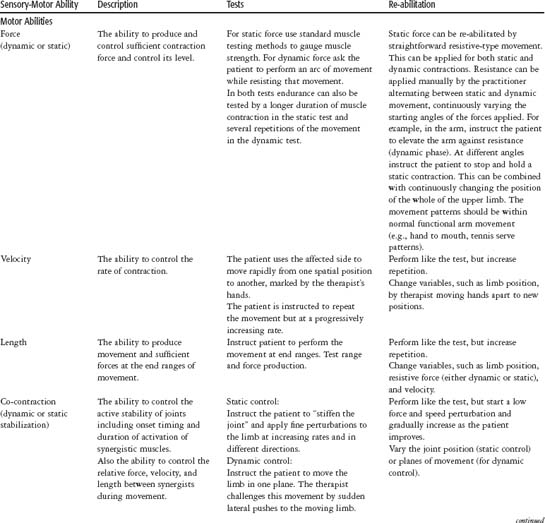
In both the intact and damaged nervous systems the initial neuromuscular rehabilitation is manual in nature. The nervous system is well buffered against external influences, and previous manual approaches had been largely ineffective at influencing this system. A new, more active approach has been developed in MT over the past 10 years.1 Some of these techniques are described as follows and in Table 16-1.
CLINICAL EXAMPLES OF DIMENSIONAL MODEL
Another clinical example is a tennis player who presents with severe neck and suprascapular pain, which is affecting playing performance. The onset of symptoms coincided with an emotionally stressful event in the patient’s personal life. This is an example of a patient whose physical symptoms could be psychosomatic in nature. Using the dimensional model, one can analyze the condition as a sequence that started in the psychological dimension in response to a particular stressful event. The next stage in the sequence is the abnormal and subconscious increase in neuromuscular activity to the now painful muscles (inability to motor relax; see later discussion on motor abilities).78–83 This phenomenon occurs in the neuromuscular dimension. This process culminates in the local tissue dimension as overuse damage to the muscle fibers, manifested as painful and tender areas in the muscles of the neck and scapular muscles. This clinical example involves a condition that “resides” in three dimensions, with each dimension requiring a different therapeutic approach and specific manual techniques (i.e., manual approaches that will help calm and relax the patient in the psychological dimension; manual techniques that will address the increased neuromuscular activity in the neurological dimension; and, finally, techniques that will address long-term changes in the muscle, such as chronic repair process and shortening).
MANUAL THERAPY—A SIGNAL FOR CHANGE
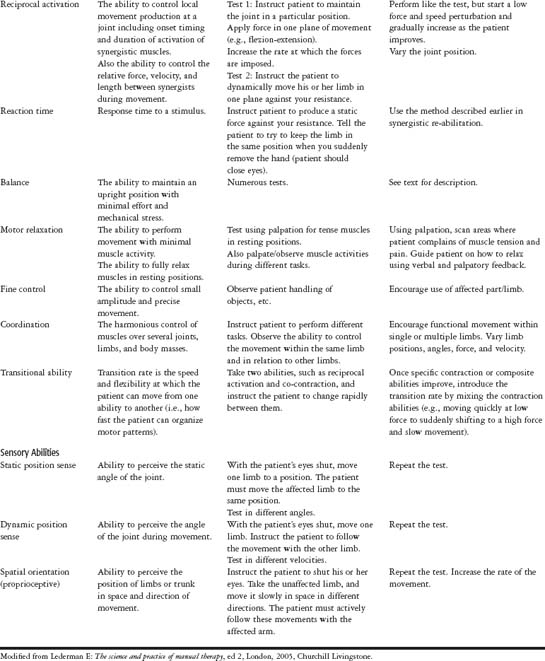
Each dimension in the dimensional model can be pictured as a door with a combination lock. The doors are the natural buffers of the body against unwanted external influences. In daily life these buffers allow only particular events to influence one’s system, while others are deflected (Figure 16-2). For example, the neuromuscular system adapts to certain events, such as repetitive exercise, but not to single motor events, consequently “forgetting” many insignificant daily actions. The signals that do activate the processes and behavior of the system can be likened to the code in the combination lock. Each of the three dimensions has a door with its own particular (and highly specific) combination code. Events that have the right code will be more successful in bypassing these buffers. This principle applies to manual events. Techniques that contain these code elements are more likely to have long-lasting therapeutic effects and vice versa. The research task that therapists have at hand is to identify the code elements for each dimension/process and incorporate them into their manual techniques.
CHARACTERISTIC OF SIGNALS/STIMULI IN THE TISSUE DIMENSION
Repair
Research in the past few years has demonstrated why MT can have such profound effects on repair and adaptation. This is related to a physiological phenomenon called mechanotransduction, a process whereby mechanical signals are converted into biochemical signals by fibroblasts and muscle cells, culminating in synthesis of different building blocks of connective tissue matrix and muscle proteins.84–95 This process is at the heart of repair and adaptation and is probably the mechanism for change activated by MT. When one stretches a muscle, the mechanical tension is a signal for the myocytes to synthesize the contractile proteins. These will be deposited in series, like beads on a chain, resulting in long-term muscle elongation.
Repair is a highly adaptive process, and the regeneration and remodeling of tissue depend heavily on the mechanical environment of the tissue (mechanotransduction). A well-established fact is that repair responds well to mechanical stimulation in the form of movement.6–18 Movement provides a blueprint from which the regenerating connective tissue scaffolding is reconstructed. Movement has been shown to be highly effective in improving the rate of recovery, improving the quality of the regenerating tissue, reducing hospital stays, improving the quality of cartilage repair, improving circulation, and reducing edema in the tissues.96–112
Repair will fail if the tissues are not provided with mechanical stresses. This will manifest in excessive connective tissue proliferation, adhesion formation, and a low-quality matrix that is mechanically weaker. In the muscle-tendon unit this will result in atrophy shortening and abnormal revascularization.12–18
The mechanical force should be dynamic/cyclical, repetitive,97–117 and within the normal physiological ranges. Human and animal studies have shown a trend in which dynamic and cyclical events are more effective than static mechanical events in stimulating repair. Movement can be either in the form of passive joint oscillation or active by assisted movement.
Some research on joint repair suggests that passive movement, in comparison with active movement, is ideal in the early stages of repair because it provides a better control of the stresses imposed on the tissues.115,116 Movement is also important in stimulating fluid flow at the site of damage necessary for successful repair (see later).
Different MT techniques can be selected according to their content of code elements. The greater code elements a technique has, the more effective it is likely to be at assisting repair and vice versa. The manual techniques that contain these mechanical code elements are harmonic techniques,118 oscillatory techniques, joint articulation, and soft tissue massage techniques (for more superficial tissues).
Harmonic techniques were developed by Lederman118 with the particular aim of providing repair-assisting manual techniques. Harmonic technique is a form of oscillatory technique that provides continuous passive motion (depending on the area of the body, the frequency is about 60 cycles per minute and can be applied for periods up to 20 minutes).
Techniques that provide passive movement will also have an effect on the transsynovial pump, a physiological system in joints responsible for stimulating fluid flow in and out of the joint space.119–121 These techniques are important in treating joint injuries where there is inflammation, effusion, and edema.
Fluid Flow
Gross fluid flow in the body is generated by mechanical pump systems (heart, vascular pump, muscle including peristalsis, respiratory pump, and movement). All these systems share similar mechanical properties. They work on the principle of the pulsatile pump, which generates fluctuating pressure gradients within and between the different fluid compartments (fluid moving from high-pressure to low-pressure areas).122 From these systems important clues can be obtained as to the mechanical nature of manual pumping techniques. To stimulate fluid flow these techniques should provide
The compression should be in a cyclical pattern alternating between compression and decompression. This alternating manual pressure should be rhythmic and repetitive, comprising many cycles during single and subsequent treatments.123–126
The potency of different manual therapy techniques in stimulating flow can be estimated by their content of pump code element. In order of efficacy are harmonic pump techniques, massage (if performed with compression rather than stretching), and effleurage for superficial drainage. Techniques that provide rhythmic movement will also activate fluid flow (see previous discussion on repair).118
Length Adaptation
The physical signals necessary for length adaptation have been identified from the extensive research into physiology stretching. These manual techniques should provide127–141
Stretching should be performed at slow rather than high velocities and kept stretched sufficiently long (anywhere from 6 to 60 seconds; however, duration will be affected by variables, such as the force used, the diameter and length of the tissue, the level of tissue damage, inflammation, and scar formation).133–141 Slow and sustained stretching allows the tissue to gradually elongate, bringing it more rapidly to the end-elastic range.133–141
Generally the fibroblast and myocytes are more responsive to dynamic rather then static stimuli.92–95 Therefore introducing repetition can greatly enhance the long-term effects of stretching. This can be applied in different time scales—as rhythmic low amplitude oscillation at the end-elastic range, as repetition several times a day, and as repetition that is carried out over several weeks.
From the previous code one can identify the manual therapy techniques that are likely to be more effective in promoting length adaptation. They are static and rhythmic stretching and can be either passive or active (e.g., muscle energy techniques). Important differences between passive and active stretching are discussed fully in Lederman.1
CHARACTERISTIC OF SIGNALS/STIMULI IN THE NEUROLOGICAL DIMENSION
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree