Chapter 8 Pathophysiology of Injury to the Overhead-Throwing Athlete
After studying this chapter, the reader will be able to do the following:
Conte et al1 performed a study over a 5-year period from 1995 to 1999 that determined the prevalence of upper extremity injuries in Major League Baseball. They found an injury rate of 27.8% and 22% involving the shoulder and elbow, respectively. The authors also reported in a prior study between 1989 and 1999 that 48.4% of all injuries in Major League Baseball involved pitchers.1 The data suggest that half of all Major League Baseball injuries that necessitated removal of the athlete from the active roster and placed on the disabled list were related to pathology to the upper extremity.1,2
STAGES OF OVERHAND THROWING
Windup
The purpose of the windup is to organize the body beneath the arm to form a stable platform. The body must perform in sequential links to enable the hand to be in the correct position in space to complete the assigned task. The scapulohumeral rhythm must place the hand in an optimal position for propulsion. The humeral head is centered in the glenoid during the first initial phase of elevation via the supraspinatus. Due to the windup phase having such individualistic styles among athletes, there is no consistent pattern of muscle activity.
Late Cocking
The supraspinatus, infraspinatus, and teres minor are active in this phase but become quiet once external rotation is achieved. Deceleration of the externally rotating humerus is accomplished by contraction of the subscapularis. The subscapularis remains active until the completion of late cocking. The serratus anterior and the clavicular head of the pectoralis major have their greatest activity during deceleration. The biceps brachii aids in maintaining the humerus in the glenoid by producing a compressive axial load. At the end of this phase, the triceps begins activity and provides compressive axial loading to replace the force of the biceps. The capsule winds tightly in preparation for acceleration. The humeral head experiences a force of anterior translation equivalent to 40% of body weight.3
Acceleration
Acceleration is a ballistic action lasting less than one tenth of a second. The ball is accelerated from 4 mph to 90 mph or higher.4 This rapid acceleration produces angular velocities that have reported as high as 9198 degrees/sec.5 The scapula is protracted, rotated downward, and held to the chest wall by the serratus anterior. The arm continues into forward flexion and is marked by the maximal internal rotation of the humerus. The humerus travels forward in 100 degrees of abduction but adducts about 5 degrees just before release. The latissimus dorsi and pectoralis major deliver the power to the forward-moving shoulder. The subscapularis activity is at maximum levels as the humerus travels into medial rotation. The triceps develops strong action in accelerating the extension of the elbow.
The forces developed in this instant reflect the body’s ability to generate power and encase itself in a protective mechanism. Pappas et al5 reported peak accelerations approaching 6000 degrees/sec. Gainer et al6 reported 14,000 inch lbs of rotatory torque produced at the shoulder. This torque develops 27,000 inch lbs of kinetic energy in the humerus.
Follow-Through
The task of documenting the sequence of muscle activity during the act of pitching has allowed the musculature acting on the glenohumeral joint to be divided into two groups.7 The first group of muscles consists of those that are most active during the second and third phases of throwing and early and late cocking. They are least active during the acceleration phase. The deltoid, trapezius, external rotators, supraspinatus, teres minor, and biceps brachii comprise this first group.
It has been postulated that in order for the elite pitcher to reach velocities of mid to upper 90s, excessive external rotation of the glenohumeral joint must occur during the late cocking and acceleration phase of throwing. This hyperexternal rotation is often seen in elite pitchers who appear to have a set point of external rotation that they know they need to attain to throw with maximum velocities. These high-level pitchers have a proprioceptive sense of reaching their set point of hyperexternal rotation, which they call the slot.8
The amount of external rotation at the glenohumeral joint has been measured to reach upwards of 130 to 170 degrees during this phase of throwing.8 The arm has been clocked at moving from 7000 to 9000 degrees/sec during the acceleration phase of throwing as it moves into internal rotation at the glenohumeral joint.9 Jobe et al10 described that one of the main reasons shoulder pain occurred during the act of throwing was an impingement-instability overlap. They postulated that repetitive throwing and this hyperexternal rotation gradually induced a serial stretching of the anterior capsuloligamentous complex. According to Jobe et al,10 this would then lead to the anterosuperior migration of the humeral head during throwing, thus inducing subacromial impingement symptoms, and affect the athletes’ throwing ability. However, these authors reported only a 50% success rate of pitchers returning to sport for 1 year following open capsulolabral reconstruction.11
In the past the primary rationale for the ability to reach these amounts of hyperexternal rotation was thought to be due to serial laxity of the anterior capsuloligamentous tissues.12 This repetitive microtrauma eventually could lead to subluxation and eventually dislocation or the so-called “dead arm syndrome.”
INTERNAL IMPINGEMENT
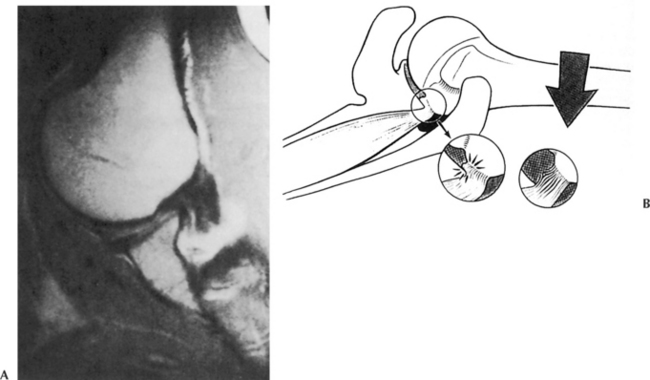
Walch et al13 were the first to describe a condition known as internal impingement, which relates to intra-articular compression that occurs in all shoulders when they are in the abducted and hyperexternally rotated position. Walch described that in the position of 90 degrees of abduction and 90 degrees of external rotation position, the posterosuperior rotator cuff, mainly the supraspinatus, contacts the posterosuperior glenoid labrum and may become impinged between the labrum and the greater tuberosity (Figure 8-1). Jobe extrapolated this observation to the throwing athlete and described the propensity of internal impingement to possibly lead to injury to the rotator cuff, glenoid labrum, and osseous structures.14 Jobe also hypothesized that internal impingement in throwers might worsen over time due to the serial stretching of the anterior capsuloligamentous structures. Jobe believed there was a hyperangulation occurring at the humeral head as opposed to hypertranslation that needed to be kept in check by the subscapularis during the act of throwing to help control this hyperexternal rotation.14
The thrower with internal impingement will most often complain of pain in the posterior aspect of the shoulder in the late cocking and early acceleration phases of throwing.15 The posterior impingement sign can confirm a diagnosis of tears into the posterior labrum or rotator cuff, or both.16,17 In this test the patient is positioned supine with the shoulder in 90 degrees of abduction and maximum external rotation (Figure 8-2). Re-creation of the patient’s symptoms with the arm in this position elicits pain of a deep nature within the posterior aspect of the shoulder. Applying a posteriorly directed force (as in the relocation test) to the humeral head while in the position of 90 degrees of abduction and maximum external rotation that reduces or eliminates the posterior pain may also be diagnostic.17 The surgical approach to address the previous description of internal impingement led to anterior capsulolabral reconstruction under the hypothesis that the anterior microinstability was the underlying mechanism of the internal impingement. However, the results of this surgical intervention for throwing athletes remained unpredictable.11,18
Gerber and Sebesta19 arthroscopically assessed 16 individuals who were not described as throwing athletes with moderate to severe and primarily unexplained shoulder pain provoked by anterior elevation and internal rotation and who were unresponsive to subacromial injection. None of the patients had signs of instability. The authors determined that when the subjects’ arms were internally rotated and elevated below 90 degrees, impingement occurred between the deep surface of the subscapularis tendon and the anterior glenoid labrum and rim. Gerber and Sebesta’s study suggests that in addition to the posterosuperior impingement of the supraspinatus tendon originally described by Walch, anterosuperior impingement of the deep surface of the subscapularis is a form of intra-articular impingement.19 This impingement may be related to a lack of deceleration control or eccentric strength of the external rotators during the follow-through phase of throwing, which could result in an excessive amount of flexion and coupled internal rotation leading to the intra-articular subscapularis impingement.
Other authors such as Halbrecht et al20 and Burkhart et al8 disagreed with the premise that anterior instability would aggravate internal impingement. They felt that an anterior instability would most likely lessen the posterosuperior glenoid contact with the rotator cuff due to the fact that the unstable shoulder is subluxing anteriorly. This could be an underlying reason why anterior stabilization procedures did not appear to have predictable and promising results in the overhead-throwing athlete.
More recently, Burkhart and Morgan,21,22 on the basis of two arthroscopic studies, clinical observation, and biomechanical data, have questioned the role of microinstability as the universal cause of throwing injuries. Burkhart et al reported on 53 baseball players, 44 of whom were pitchers, who had Type II superior labrum anterior to posterior (SLAP) lesions that were surgically repaired after failed conservative rehabilitation. Arthroscopic repair of these Type II SLAP lesions returned 87% of these athletes to a preinjury level of performance.21 This was superior to the reported successful return of athletes after open anterior capsulolabral repairs, which ranged from 50% to 68% return to sport.11,18 Burkhart et al do not believe that the underlying lesion is the anterior capsular laxity or microinstability but that the SLAP lesion induces a “pseudolaxity,” which has led to the erroneous diagnosis of microinstability.8
Pitchers and throwing athletes are believed to be at risk of developing SLAP lesions due to the obligatory tightening of the posteroinferior glenohumeral capsule.8 In studying 372 professional baseball players, Wilk and Meister23 have reported that external rotation on average is 7 degrees greater in the throwing shoulder and internal rotation is 7 degrees greater in the nonthrowing shoulder. The average total shoulder range of motion was reported as 129.9 plus or minus 10 degrees of external rotation and 62.6 plus or minus 9 degrees of internal rotation. The authors coined the term total motion concept to describe total shoulder motion being equal to the summation of external and internal rotation. Thus an individual with an imbalance of external to internal rotation as such would lend to dynamic instability with overhead throwing.
In 1991, Verna was the first to recognize the relationship between gross internal rotation deficit (GIRD) and shoulder dysfunction in the throwing athlete.24 During a baseball season he assessed 39 professional pitchers who were determined to have 25 degrees or less of total internal rotation at spring training (GIRD, ≥35 degrees in each of these pitchers). During the course of the study and season, 60% developed shoulder problems requiring them to stop pitching. These findings of restricted internal rotation correlate with a tight posteroinferior capsule but can also be attributed to tightness of the external rotators and osseous adaptations of the humeral head or glenoid.2
Cooper manually stretched 22 Major League pitchers daily to minimize GIRD to less than 20 degrees during the 1997, 1998, and 1999 professional baseball seasons.8 During those seasons, he reported innings lost, no intra-articular problems, and no surgical procedures in the study group. These reports help substantiate that a prophylactic-focused posteroinferior capsular stretching program is successful in minimizing GIRD and is effective in preventing secondary intra-articular problems, particularly posterior Type II SLAP lesions.8
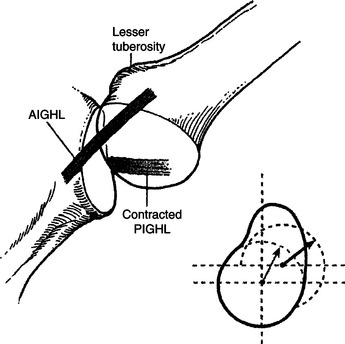
According to Burkhart et al,8 this acquired loss of internal rotation caused by the posteroinferior capsule contracture is the “essential lesion” that leads to a secondary resultant increase in external rotation. They believe this occurs via two mechanisms by which a tight posterior capsule induces hyperexternal rotation of the humerus. First, the tethering effect of the posterior capsular contracture shifts the glenohumeral contact point posterosuperiorly, allowing the greater tuberosity to clear the glenoid rim through a greater arc of external rotation before internal impingement occurs (Figure 8-3). Second, the shift in the glenohumeral contact point reduces the cam effect of the proximal humerus on the anteroinferior capsule to allow greater external rotation due to the redundancy in the capsule (Figure 8-4). They define GIRD as a loss in degrees of glenohumeral internal rotation of the throwing shoulder compared with the nonthrowing shoulder. Glenohumeral internal rotation deficits of 15 to 20 degrees have been associated with nonsymptomatic pitchers, while symptomatic pitchers have reported deficits as high as 45 degrees.2,22
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree