2 Treatment Techniques Manual techniques are among the most basic of the treatment techniques available to physiotherapists in their approach to treatment, and they are also among the most valuable in relation to pelvic floor disorders. With an optimum amount of pressure placed on target tissues in the proper location, the physiotherapist is able to facilitate and strengthen musculature, decrease unwanted tensions, mobilize structures and tissues, and relieve pain [Wise 2003]. In general, the pelvic floor responds well to the manual approach, and the proprioceptive effect of this form of treatment cannot be overstated. The manual physiotherapy techniques used for the pelvic floor musculature are similar to those used for muscle and tissue elsewhere in the body. They can be done on the surface of the perineum, and internally, by vaginal or by anal palpation. Techniques such as massage, transverse frictions, proprioceptive stimulation, myofascial release, trigger-point pressures, the use of the myotatic reflex, muscle energy, mobilizations, passive movements and manual resistance are used for a variety of purposes [Markwell 2001, Shestack 1977]. With a detailed questionnaire, a thorough pelvic floor evaluation and a review of pertinent reports, the physiotherapist defines the patient’s list of problems and establishes treatment goals. The manual technique to be employed is chosen according to these goals of treatment. Throughout the manual approach, the physiotherapist is able to concurrently evaluate, treat, reevaluate, and adapt the treatment process. It is very important to explain to the patient the nature of the manual technique to be performed, its goal, and the approximate sensation that will be produced. Clear verbal consent from the patient is essential, and it is advisable to repeat the request of consent when changing from vaginal to anal palpation. Regular eye contact with the patient is recommended, as any form of unease will usually be visible through facial expression, and this will often precede any verbal mention of discomfort or local physical response. The physical response within the tissues of the pelvic floor gives the therapist essential cues about the effect of the manual technique. It is through communication with the patient and experienced palpation of the tissues that the therapist is able to gauge the patient’s reaction and to adapt the application of the technique accordingly. The five common goals of pelvic floor physiotherapy, and the rationale for the manual approach to be employed, are discussed below. Table 2.1 summarizes the goals of therapy and the corresponding manual techniques [Brown 2001]. Many patients may have difficulty in understanding the configuration of the pelvic floor musculature and in comprehending the nature of its contraction [Wallace 1994]. This is not surprising, as the musculature is relatively hidden, and the movement produced by its contraction is three-dimensional. Also, the osseous movement resulting from a pelvic floor contraction is not easily evident to the patient. Compare this, for example, with the easily visible angular displacement caused by a biceps contraction in the upper extremity. Facilitation will help the patient to learn to contract the musculature, and will help encourage the less active of the muscle fibers to come into play. This may be necessary in the absence of local pathology, as well as for patients who may have difficulty in contracting because of direct injury, abnormal tone, or nerve damage. Facilitation is indicated when the patient’s contraction is absent or inadequate, or when the contraction is inconsistent in strength, duration or in the facility of its recruitment.
2.1 Manual Physiotherapy Techniques for Pelvic Floor Disorders
 Facilitation
Facilitation
1 Facilitation of muscular contraction
|
2 Mobilization
|
3 Strengthening
|
4 Normalization of tone
|
5 Pain modification
|
Simple directive pressures can be used for pro-prioceptive facilitation [Cotelle 1990]. For an external approach, the pad of the thumb or forefinger is placed over the labia, pressing in towards the vagina. As the patient is asked to contract the pelvic floor, she feels the pressure and makes the neuromuscular connection (Fig. 2.1). Tapping can also be done, with quick and successive light taps on the skin surface over the desired muscle group. Both the direct pressures and the tapping procedures prove to be even more effective when done internally, directly over the muscle belly, by vaginal or by anal palpation.
We may also facilitate with massage. Perineal massage, usually performed internally, helps to improve circulation and proprioceptive awareness. A crooked finger position is best used, with two digits massaging the superior surface of the pubococcygeal portion of the levator ani group, with vaginal palpation (Fig. 2.2). Gentle but firm pressure is used, massaging in an anterior to posterior direction from the pubis to the coccyx, then releasing the pressure and recommencing, again from anterior to posterior. For greatest comfort, the massage procedure is first completed on one side and then the other. This approach is especially useful for patients with asymmetrical strength. Deeper massage may also be done vaginally, pressing in deeply, over the iliococcygeal portion of the levator ani muscle on either side. These techniques may also be used for facilitation via anal palpation.
Passive mobilization of the soft tissue may also facilitate a pelvic floor contraction. If the patient cannot generate enough force to mobilize the muscle completely, the therapist may assist the contraction by mobilizing the pelvic floor superiorly [Chiarelli 1992]. Firm pressure is placed on the surface of the perineum, pressing superiorly on both sides as the patient is asked to contract. This assistance will allow the patient to feel the motion of a full contraction even if she is not able to perform it entirely on her own.
The physiotherapist may make use of the myotatic reflex in order to facilitate a contraction [Caufriez 1988, 1989]. The bulbocavernosus reflex is used to elicit a reflex contraction of the pelvic floor via a quick stretch at the introitus, and is used for proprioception and facilitation. To elicit the reflex, two fingers are placed in the vagina. With pressure on the central perineal tendon, the tissues are first gently pulled posteriorly and laterally towards the ischial tuberosity until a certain amount of tension is encountered. A short-duration, high-intensity stretch is then performed in a posterolateral direction in order to reflexively elicit a contraction at the anal sphincter and pelvic floor. Once the reflex has been performed, the patient is asked to contract actively to benefit from the neuromuscular stimulation that has just taken place. Also, the patient may be asked to contract during the elicitation of the reflex.
Patients who are already able to generate some form of contraction may benefit from manual resistance as a facilitatory technique. The application of enough pressure against the muscle belly to prevent displacement will oblige the muscle to work isometrically and encourage more muscle fibers to work, and with more intensity.
 Mobilization
Mobilization
Limited mobility of the structures and tissues within the pelvic floor may contribute to symptoms such as pain and/or decreased contractility [Travell and Simons 1983]. The restrictions may be of an osteoarticular nature or soft tissue, at the level of the skin, muscle, or fascia [Tousignant 1989]. The detailed pelvic floor evaluation should include an evaluation of tissue mobility as well as an evaluation of the resting position and passive movements at the sacrococcygeal joint. At rest, the sacrococcygeal joint is flexed approximately 30 and it should have a flexion–extension range of approximately 30 [Thompson 1977].
Massage techniques may be used to mobilize some soft-tissue restrictions. The basic massage technique described above, when performed with adequate pressure and stretch, is a very useful mobilization technique. Transverse frictions may be added, perpendicular to the muscle fibers, to help break down adhesions and mobilize. Myofascial release is another manual technique in which gentle yet constant pressure is applied in order to improve the mobility and function of the myofascial component of the tissue [Travell and Simons 1983]. With directive pressures performed internally over the superior surface of the pelvic floor, the therapist encourages tissue release and mobilization. With myofascial release, one is said to work through the layers of resistance, as continued pressures will allow for the release of fascial and muscular layers, one at a time. Promoting fascial, or connective tissue mobility is key to promoting pain-free function of surrounding units [Shelly 2002, Dereix 2002]. Once the mobility has improved, the muscle contraction may more easily be performed, and pain levels may decrease.
Stretching techniques are also instrumental in mobilization. Taking into consideration the funnel-type configuration of the musculature, the therapist may encourage elongation by applying a gentle yet firm stretch in the direction of the muscle fibers, holding for a minimum of 20 seconds. Stretching techniques may also be done at the entrance to the vagina for the mobilization of skin and connective tissue—for example, in the case of patients with related dyspareunia.
Muscle energy techniques are among the most useful mobilizing techniques for the pelvic floor as they are usually very effective and quite painless [Gardiner 1976]. As there is no true antagonist muscle group to the pelvic floor musculature, a contraction of the agonist is used in order to obtain subsequent relaxation. If the patient’s contraction against resistance is pain-free, a maximal contraction is performed against the resistance of the therapist’s digits. A more complete relaxation is the desired result, and can be followed by a manual stretch technique for optimal mobilization. This is an internal technique.
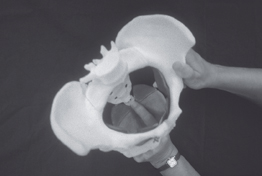
If the restricted mobility is at the osteoarticular level, specific sacrococcygeal joint mobilizations may be done [Tousignant et al. 1995]. Palpation of this joint is best done bimanually, with an internal palpating digit on the anterior aspect of the coccyx and an external digit palpating posteriorly. In this manner, the joint may passively be brought through its range, from flexion towards neutral and back into flexion again. Joint mobilization of accessory movements such as traction, side bending, and anteroposterior gliding may also be done at the sacrococcygeal joint line (Fig. 2.3). Muscle energy techniques are found to be quite helpful in this area, performed in conjunction with joint mobilization techniques.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree