CHAPTER 91 Manipulation and Manual Methods
INTRODUCTION
Central axis pain is, perhaps, the core enigma of spine disorders. The diagnosis is one often made by exception and involving many forms of trial therapy before conclusion. Like all other sources of spine pain, the diagnosis may be confounded by the presence of other potential pain generators that have overlapping clinical and physical symptoms. Discogenic pain has variable presentation from primary, centralized aching spinal and paraspinal pain to bizarre sclerotomal pain of the lower extremities. Severity may wax and wane as patients undergo differing levels of weight-bearing load to their spine with episodes of overstrain to the disc material. Various forms of treatment from medication to spinal manipulation give relief that is temporary. Exercise may be relieving or aggravating. In a retrospective study, Smith and colleagues1 noted that 68% of patients with positive discography improved without surgery over a 4-year interval while 24% deteriorated. Some patients require more treatment to relieve their suffering than others. However, weight-bearing and activity intolerance is a consistent pattern among the various presentations of central axis pain.
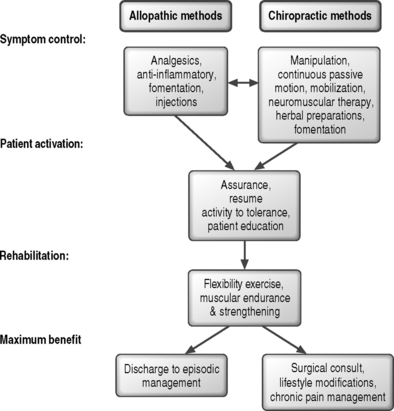
The key purposes for providing treatments (Fig. 91.1) are to relieve suffering, improve function, and maximize healing capacity. The nonoperative allopathic methods most often employ biochemical mediators to manage symptoms, followed by biomechanical interventions to modify loading of the spinal tissues to reduce local stress concentrations and strengthen core muscles while maximizing pain-free flexibility. The chiropractic methods seek to minimize or alter local physical tissue stress through the use of applied forces and moments, followed by interventions to modify behaviors that load the tissues, strengthen muscle and increase trunk stiffness, and improve pain-free flexibility. Should either approach be insufficient, a surgical consultation can be considered. The practical difference, ignoring the debates over disciplinary jargon, is the relative emphasis on the best means to reduce tissue stress, inflammation, and pain. The allopathic view relies heavily on chemical intervention to block pain and suppress inflammation followed by efforts to reduce tissue stress. The chiropractic view prefers to alter the mechanical environment, allowing inflammation and pain to subside. Patients often consult both types of care simultaneously without disclosing to either. Increasing professional interactions between the groups suggest that a meaningful number of cases may benefit from both approaches.
Spinal manipulation is a mechanically applied therapy used to relieve nociceptive pain and improve function. A number of clinical and physiological effects are known2–4 and their attributes require appropriate and skillful application to achieve safe and successful outcomes.5–9 The clinical benefit from use of these procedures has been studied10,11 in subacute and chronic back pain cases, a heterogeneous population of patients including many with central axis pain. This chapter will discuss the theoretical underpinnings of spinal manipulation and its use in the management of central axis pain.
THE BASIS OF SPINAL MANIPULATION
The lesion
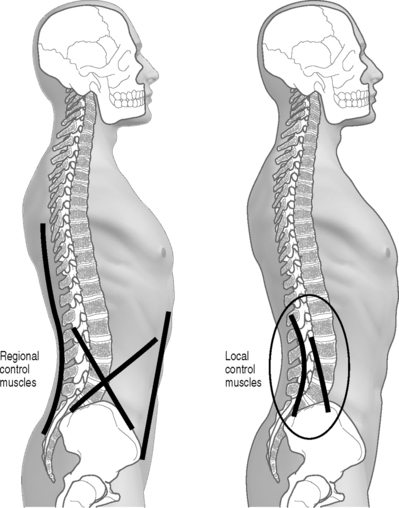
The mechanism of the manipulable spinal lesion is characterized biomechanically as a buckling event. These phenomena have been observed in orthopedics for some time among some patients with an unstable wrist carpus12,13 and are associated with multiarticular kinetic chain systems like the spine that rely on biarticular muscles for establishing local mechanical equilibrium and control. Detailed review of the biomechanics of these lesions can be found elsewhere.14–16 Briefly, buckling may involve single functional spinal units or an entire spinal region. They are caused by a mismatch in timing or amplitude of response between the local and regional muscular control systems (Fig. 91.2). A local shift of intersegmental joint configuration occurs within the bounds of normal range that is disproportionate to the task at hand. Symptoms arise from the increase in local tissue strain. The clinical presentation of the patient and the exact symptoms depend on the identity of the tissues strained to injury threshold and the presence of comorbid conditions.
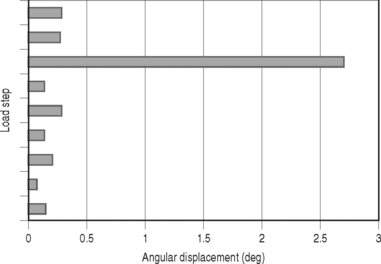
The mismatch between the demand of spinal load and appropriate local intersegmental stiffness results in a sudden shift in relative joint configuration (Fig. 91.3). That is, there is a disproportionate repositioning of the joint within the bounds of its normal functional range. Instead of supporting the patient’s posture and activity with minimum local tissue strain, the new configuration may result in a local stress concentration leading to symptoms of the involved tissue. Effectively, while the buckled equilibrium may be functional, it is with increased cost in terms of comfort. These types of buckling phenomena have now been observed under biomechanical testing conditions in vitro for isolated segments17–19 as well as the lumbar region20 and, by happenstance, during experimental studies of weight lifters when an unexpected injury occurred.16,21
The factors associated with development of local buckling are found in Table 91.1. Prior injury or degenerative disease potentiates buckling, allowing it to occur more easily, effectively lowering the critical load requirements and reducing the ultimate load capacity. Fig. 91.4 describes the chain of events leading to symptoms.
Table 91.1 Etiologic factors for local joint buckling events based on available biomechanical experiments in vitro and in vivo15,16
| Causative | Facilitating |
|---|---|
| Sudden incremental load after prolonged static posture | Vibrating environments |
| Unexpected load | Disc damage |
| Rapid load events (500 lb/sec) | |
| Uncoordinated/fatigued effort |
Diagnostic findings
The determination of a manipulable lesion in isolation is relatively straightforward but is made more complicated by the presence of other pathology. Table 91.2 provides a review of findings warranting a trial of spinal manipulation. Unraveling symptoms that may respond to manipulative methods, however, is easily achieved through a trial therapy interval. Provocative testing can be used to identify the specific directions of loading that give comfort and relieve symptoms. Such maneuvers guide the selection of treatment procedures that match patient needs. These maneuvers apply controlled forces and moments, often involving postural positioning or tasks, to the suspected dysfunctional joint. Based on knowledge of any comorbid pathoanatomical diagnosis and associated findings (palpation sensitivity, flexibility, orthopedic/neurologic testing and imaging/laboratory test results), initial trials of provocation are performed in an effort to reduce local tissues stress. The principal governing diagnostic interpretation is the partitioning of patient response to applied loads into categories of those that relieve or those that aggravate symptoms. Results that reduce symptoms and any referred or radicular pain components are the desired motions for directing the choice of procedure and the application of manipulative methods. Joint or nerve blocks may be helpful in identifying the pain generator (facet, sacroiliac, or nerve root) and quelling local inflammatory responses that may be interfering with patient recovery.
Table 91.2 Signs and symptoms of the isolated manipulable lesion
| Local back pain with or without limb pain absent progressive neural signs |
| Focal sensitivity to manual pressure |
| Local muscular hypertonicity with or without tender points |
| Limited joint compliance in mid-range position and/or end-range limitations with pain on overpressure testing |
| Reproduction of symptoms with joint compliance or end-range motion testing |
| Local soft tissue edema |
| Altered local skin turgor, temperature or color |
Manipulation skill and control factors
Manipulation, like all other therapy, must be performed using sufficient skill and knowledge. Applications include the ability to use thrusting and nonthrusting techniques where appropriate, which requires an in-depth clinical assessment and differential diagnosis.22 Used in trained hands, these methods are remarkably safe.23–25 Evidence shows that minimally skilled individuals are ineffective in producing good outcomes6 with recovery from a symptomatic episode. Efforts to extend one’s practice into the field of manipulation based on superficial weekend training programs may be pedagogically wrong and potentially dangerous.26,27
Threshold is defined as the application of necessary and sufficient joint load to effect a change in its behavior and symptoms. Threshold levels are a function of patient joint stiffness, soft tissue viscoelastic properties, and muscular tension that may vary themselves, based on age, severity or acuteness of symptoms, and patient anxiety levels. Assessment of tissue condition to guide application of the procedures is a skill developed through supervised practice and experience. In cases where there are multiple tissue elements involved (e.g. reactive muscle tension, capsular swelling, adhesions, hemorrhage), sequential procedures may be necessary. Staged procedures can speed the removal of local fluid or breakdown interstitial adhesions without exceeding patient tolerance for more severely injured or sensitive tissues. Choice of treatment modality is dependent on the presence or absence of pain during the examination (provocation testing). Empirically, patients with localized pain seem to respond better to impulse loads as long as the preliminary joint positioning can be engaged without difficulty.22 Patients who are unable to be effectively positioned or have chronic or referred pain may initially benefit more rapidly using procedures without impulse.
Effective dosage and duration of therapy varies with patient cooperation on reducing aggravating factors, performing recommended exercises to gain stability, the presence of other pathology or degenerative change, and condition severity. In general practice, initial treatment dosage is 2–3 sessions per week. Haas et al.28 have shown a direct relationship between treatment frequency and outcome scores for pain and disability for patients with chronic low back pain. A statistically significant linear relationship noted greater improvement for patients treated 3–4 times per week over a 3-week period. Across the literature, the average number of treatment sessions to maximum improvement for uncomplicated cases ranges from 8 to 18 with a range of approximately 1–40 treatments, depending on complexity and complications.29,30
TREATMENT METHODS
Manual therapy concerns itself with the treatment of functional disturbances of muscle and joints including their local or remote symptoms. There are a number of ways in which manual therapy has been divided for discussion. Manipulation is a specific form of manual method that uses rapid impulse loads to the body structures. Manipulation can be quantitatively differentiated from other methods on the basis of speed of application14 and the differing response of the body tissues to rapid loading. While many systems of manual treatment methods exist, including manipulation, the common factor is the controlled application of loads (forces and moments) to the spine. The various approaches may be most easily understood when broken down into their biomechanical control parameters. Such classifications also help to align treatment objectives to therapeutic goals. That is, the body’s biomechanical response to load application will depend on tissue properties and their reserve viscoelastic and stiffness characteristics. The various procedures span a spectrum of force and moment amplitude, speed, and direction of application that are designed to influence joint and disc strain and normalize mobility.
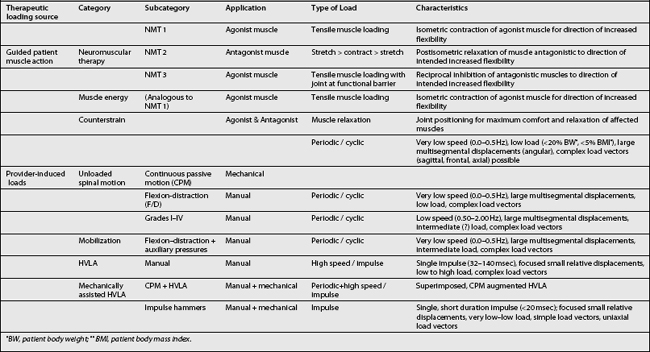
The therapeutic loads can arise from two primary sources. They are generated either by action of the treating physician or from patient muscle action (stretching, relaxing, or contracting) under the guidance of the provider. Depending on the clinical discipline base (chiropractic, osteopathy, or manipulative medicine) of the provider administering these procedures, the specific name will vary (Table 91.3). Guided patient muscle action may be termed neuromuscular therapy, muscle energy, or counterstrain maneuvers. Provider-induced motions are typically characterized by repetition rate, speed, and amplitude and fall under the terms manipulation or adjustment and mobilization. Finally, various assistive devices that may be used to control the patient motion direction, rate, and amplitude are termed mechanically assisted procedures. These latter may be coupled with manipulation methods to provide motion assisted manipulation procedures.
Guided patient muscle activation
Neuromuscular therapy (NMT) utilizes direct muscle action as well as associated neuromuscular reflex mechanisms to improve mobility and normalize muscle tone. Its action is based on the principle that inhibited or weakened agonists or competition of hypertonic antagonists may limit joint function. For example, spinal motion of rotation may be limited by inhibited contralateral transversospinal groups or by shortened ipsilateral transversospinal muscles. The pattern is determined by provoking local joint motion and determining its relative compliance in a direction and contrasting that with the presence of muscle tenderness and relative hypertonicity.22 There are three types of NMT, their use being dependent on whether the desired effect is to relax hypertonic agonists or strengthen them or to relax hypertonic antagonists as noted below.
NMT1: Agonist muscle considered weakened or hypotonic.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree