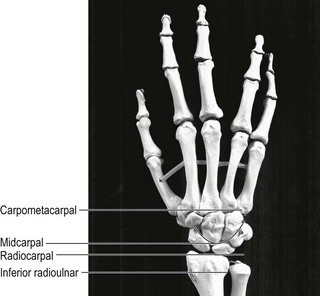
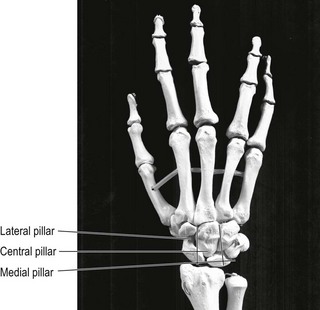
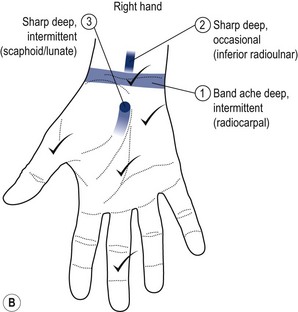
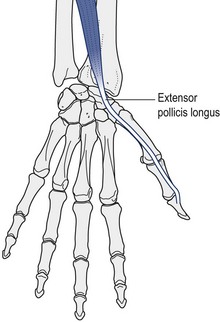
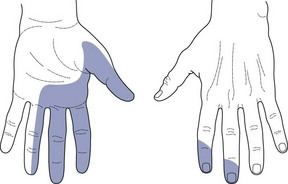
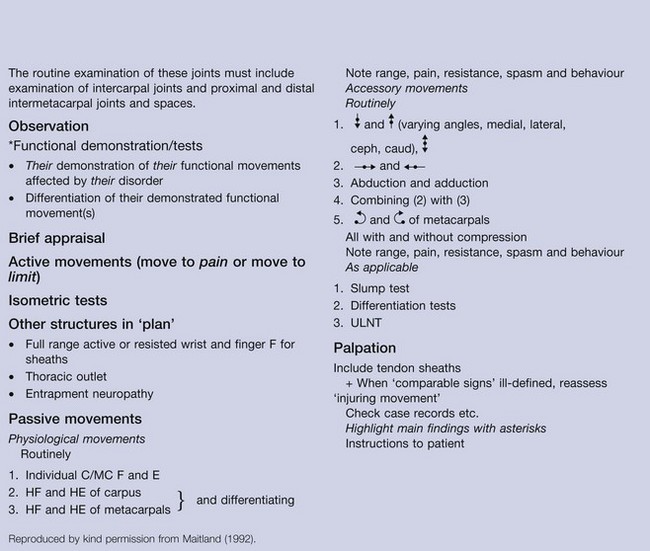
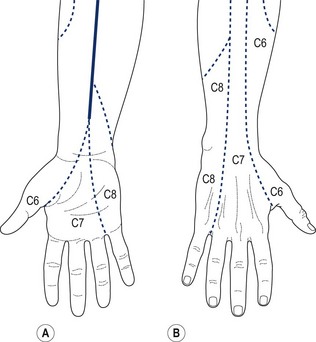
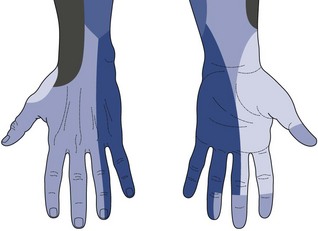
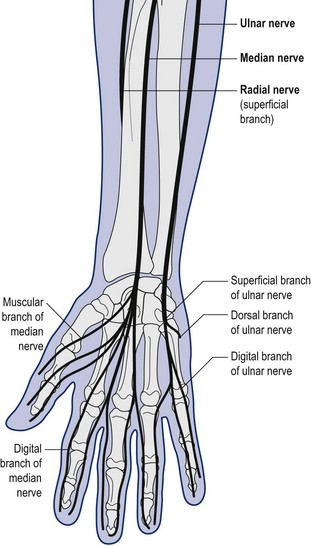
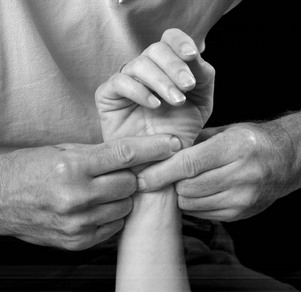
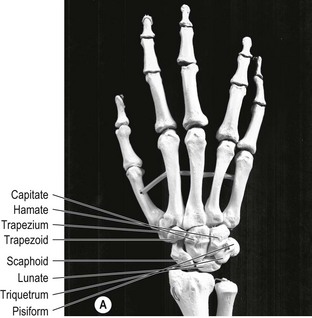
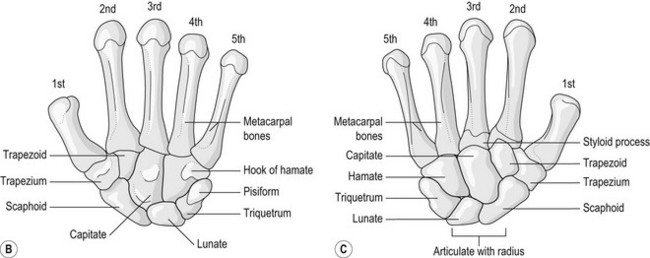
6 The bio-psychosocial role of the hand is greater than that of any other part of the body. Hofer (2009) has long recognized the role of the tactile kinaesthetic system (touch or feeling) in the development of mankind. The hand and the brain act as a functional unit. The hand occupies a central place and is highly represented within the sensory homunculus. The hand within the sensory homunculus plays an important role in maintaining internal homeostasis and balance relative to the socioemotional environment and functioning. Manual therapists, too, are clearly a professional group whereby if they experience a small loss of function of the hand, there will be major consequences in terms of participation (job and hobbies) and quality of life (feeling of fulfilment). The effect of the smallest derangement or disease on functioning and disability is crucial. The International Classification of Functioning, Disability and Health (ICF) ( WHO 2001) provides an ideal framework for identifying the impact of hand disorders on functioning, participation and social and environmental factors in an individual’s life. Moseley et al. (2008) suggest that chronic pain may lead to reduced tactile acuity and that a clear relationship exists between pain intensity, tactile acuity and cortical reorganization. Their research shows that when pain resolves, tactile function improves and cortical organization normalizes. This demonstrates yet again the close relationship between hand and brain. 1. Nociceptive pain: recent onset symptoms which correspond to a traumatic or injurious event, normally accompanied by the cardinal symptoms of inflammation, such as swelling, heat, redness and signs of sympathetic activity (e.g. sweating), which brings us immediately to the next category – output (see below). 2. Peripheral neurogenic mechanisms: not only paraesthesia or atrophy suggest a pathological process in the nerve, but also factors of a vascular, mechanical (stretching, compression) or systemic nature. All will increase the chemical or mechanical sensitivity of the nerve and implicate it as the source of pain or movement dysfunction. The hypothesis of double crush, as described by Upton & McComas (1973) (of 115 patients with carpal tunnel syndrome, 81 had a cervical origin), is particularly relevant for the upper extremity with canal syndrome or entrapment neuropathy. Mumenthaler (1979) found that of 4958 carpal tunnel operations 9% of patients had a painful shoulder and Narakas (1990) found that of 1916 carpal tunnel operations 26% had a painful shoulder. The T4 syndrome described by Maitland et al. (2001) is another frequent situation involving symptoms of autonomic origin, distributed in the whole hand or arm, outside the dermatomes but in the sudotomes ( Jeangros 2011). Central sensitization processing occurs in chronic peripheral neuropathies, high input of action potential or injuries to other structures. As already mentioned, it also depends on the condition of the sensitivity of the CNS, which is altered by affective and cognitive dimension ( Gifford 1998). Kapandji (1982) has suggested that the following ranges of movement are considered as normal average values for the wrist and hand: Figure 6.1 A The carpal and metacarpal bones of the left hand; B palmar aspect; C dorsal aspect. B and C reproduced from Williams and Warwick 1973, with permission. • Wrist flexion and extension 85° each (movement taking place primarily at the radiocarpal and midcarpal articulations) • Wrist radial deviation 15°, wrist ulnar deviation 45° (movement taking place primarily at the radiocarpal joint with accompanying movement at the radioulnar, intercarpal and carpometacarpal joints) • Wrist pronation 85°, supination 90° (movement taking place primarily at the inferior and superior radioulnar joints, accompanied by rotation at the radiocarpal, midcarpal and carpometacarpal joints). The carpal bones can be described in terms of their rows for examination, differentiation and localization of treatment ( Fig. 6.2): the proximal row of carpal bones consists of the scaphoid, lunate, triquetrum and pisiform; the distal row of carpal bones consists of the trapezium, trapezoid, capitate and hamate. These rows therefore are components of the radiocarpal, midcarpal and carpometacarpal joints. The carpal bones can also be described in terms of pillars ( Fig. 6.3): the lateral pillar consists of the scaphoid and trapezium or trapezoid, the central pillar consists of the lunate and capitate and the medial pillar consists of the triquetrum, pisiform and hamate. The value of this is that, ideally, the mobility within the central pillar should be greater than the medial and lateral pillars when individual carpal mobility is tested ( Kapandji 1982). The metacarpophalangeal (MCP) joints can flex on average to 90° (similar to the interphalangeal (IP) joints) and can be passively rotated by 60°. The sequence for examination and treatment of the MCP and IP joints is described in detail on pages 363– 369. A good working knowledge of surface anatomy ( Hoppenfeld 1976, Kesson & Atkins 1998) will enhance the clinician’s accuracy in localization and application of forces during movement analysis of the wrist and hand. • A good working knowledge of surface anatomy of the wrist and hand will help to team up the patient’s wrist and hand symptoms with a recognizable joint, peripheral nerve or muscle. • Activity limitations which include the prehensile or non-prehensile functions of the wrist and hand will strengthen the hypotheses suggesting a local disorder. • A strong relationship between the symptoms and mechanical trauma or stress to the wrist and hand is what the clinician should expect. Essentially, the patient would be expected to complain of pain, stiffness, swelling, loss of function, loss of feeling and weakness of the wrist and hand. As discussed earlier in this chapter, a large or ‘real size’ wrist and hand chart should be used so that the precise area of the patient’s symptoms can be represented more accurately ( Fig. 6.4). In this way the area which the patient describes as being painful is often diagnostic in itself. A band of pain across the wrist is common in radiocarpal joint disorders; inferior radioulnar joint pain is usually felt locally and deep. Any referred pain is usually felt to spread from the joint towards the elbow. Pain arising from any of the intercarpal joints is always felt locally, although it may radiate out from a central point of the disordered joint. Pain from the intermetacarpal joints will be felt locally at their bases and over the joint. Pain and swelling over the abductor pollicis longus or extensor pollicis brevis tendons indicates a diagnosis of de Quervain’s tenosynovitis. Paraesthesia of the thumb, index, ring and half the middle finger is a common presentation in carpal tunnel syndrome ( Figs 6.5 and 6.6). A large diffusion of symptoms in the whole hand, occasionally accompanied by heaviness and tiredness of the whole hand, forearm, or whole arm, may lead to suspect a TOS (thoracic outlet syndrome) or a T4 syndrome ( Maitland et al. 2001, Jeangros, 2011) with the output as the dominant pain mechanism. Often, the history of the patient’s symptoms will correspond to the different recognizable patterns as described by Corrigan & Maitland (1983): • Spontanous insidious onset corresponds mostly to degenerative rheumathological disease such as arthritis or tendinopathy through overuse or repeated friction • Peripheral neurogenic mechanisms may also be considered, but are more difficult to detect, especially if they are not accompanied by paraesthesia or atrophy • Traumatic events, fractures (Colles’ fracture, scaphoid necrosis, etc.), intra- and periarticular, soft tissue (tendon, ligament, etc.) injuries should be considered. With a hypothesis of output pain mechanisms, it may be necessary to decide to treat the thoracic spine at the first treatment, either by mobilization or manipulation with the aim of calming down the sensitivity of the sympathetic trunk. This treatment could also be performed in a sympathetic slump position ( Jeangros 2011). • The observation begins when the patient enters the room and shakes hands. At this point the therapist is already evaluating the patient’s willingness to move and use the hand. The therapist will also become aware of the strength of the patient’s grip. • Inspection of the cardinal signs – colour changes of the skin, inflammation, deformity, trophic changes (skin, nails, hair), other circulatory changes, as well as general dexterity. • Let the patient demonstrate the activity reproducing their pain or producing a degree of discomfort which is considered as abnormal, limited or impairing. • Look for alignment faults with grip, including the ability to fully oppose the thumb and the range of finger flexion. • Look for gripping with the wrist in flexion or gripping with the wrist deviating (usually radial because of overpull of extensor carpi radialis brevis). • Analyze and record the ranges of movement, the symptom response and the quality of movement. • Pain increased by weight-bearing activities could confirm a more intra-articular participation. • For pain arising from the inferior radioulnar joint the functional demonstration may involve the action of turning on a tap. The point at which the pain comes on with supination is determined and in this position the ulna can be moved further into the range to determine any increase in pain. • Active movements of the whole hand with grade III+ overpressure if necessary, recording range, symptom response and quality of movement (palmar flexion 85°, dorsal extension 85°, ulnar adduction 45°, radial abduction 15°) and brief appraisal tests should also include, pronation, supination, horizontal flexion and horizontal extension. • Indication for using these ‘if necessary tests’ would be, on the one hand, to recognize the typical pattern (for example, pain after repeated movement and stiffness after rest) or localization of a muscle or tendon (knowing that most of the strains occur at the musculotendinous junction). • On the other hand, as it is nearly impossible to mobilize a joint of the wrist without having the fingers of the therapist affecting a tendon, it seems important to differentiate first if the pain is coming from a tendon or another structure. • Other indications for using isometric tests would be a diagnosis of de Quervain’s disease, Dupuytren’s contracture, a past history of overuse (secretary with mouse), a recent overstretching, a traumatic event or a muscle strain confirmed by an MRI or not. • Finkelstein’s test is, for example, used when considering dysfunction of the abductor pollicis longus and the extensor pollicis brevis suggesting a de Quervain tendinopathy: flexion (and adduction) of the thumb combined with a strong ulnar deviation. This test is very similar to the neurodynamic test ULNT 2b ( Butler 1991) for testing the radial nerve, and will need further differentiation with elbow extension, scapular elevation or lateral flexion of the cervical spine. Symptoms are seldom related to a single structure. • Most of the muscles and tendons in the hand cross more than one or two joints and perform eccentric contraction. This means the hand contains a greater proportion of mobilizing rather than stabilizing muscles. • Isometric tests are first performed in neutral and then in the functional position. The localization of symptoms and direct palpation (or deep friction) can help to differentiate beween muscles and tendons. • Tendons are tested by full stretching, maximal elongation. Further differentiation between the tendon and the sheath of the tendon (tenosynovitis) can be made by compressing the tendon at the painful spot and letting the tendon move through range. • The grip strength test can be used for re-evaluation, but is not pathognomonic. If symptoms follow a dermatomal distribution ( Fig. 6.7) or if there is a history of cervical spine involvement then a thorough neurological examination of the upper extremity is necessary. In this case, a peripheral neurological examination of the sensitivity (light touch and pinprick, reflexes and motor power will be assessed) ( Fig. 6.8). Neurodynamic tests are obligatory where there is a need to differentiate between structures causing symptoms in the upper extremity. The distribution of symptoms will determine whether there is a need to use the ULNT1 (median bias), ULNT 2b (radial bias) or ULNT 3 (ulnar bias) ( Butler 1991). • Identification of surface anatomy landmarks ( Hoppenfeld 1976). • Identification of signs of movement impairment (temperature changes, excessive sweating, soft tissue changes including swelling and soft tissue thickening, bony abnormalities such as exostosis). • Palpation of the median, ulnar and radial nerves around the wrist and hand for mechanosensitivity, symptom reproduction and signs of swelling or thickening ( Fig. 6.9). • Palpate tendons and tendon sheaths where tenosynovitis may be evident (abductor pollicis longus and extensor pollicis brevis in particular). • Brachial and radial pulses to check for circulatory viability.
Management of wrist and hand disorders
Introduction
Defining the dominant pain mechanism
Input
Output
Processing
Deciding the normal range or ideal range for wrist and hand movement ( Fig. 6.1)
Subjective examination (C/O)
Kind of disorder: establishing the patient’s main problem(s)
Areas of symptoms
History (present and past)
Planning the physical examination (P/E)
Physical examination (P/E) (Boxes 6.1–6.9)
Observation
Functional demonstration
Active movements of whole hand
If necessary tests
Isometric tests (grip strength test)
Neurological examination
Neurodynamic tests
In supine lying
Inspection and palpation