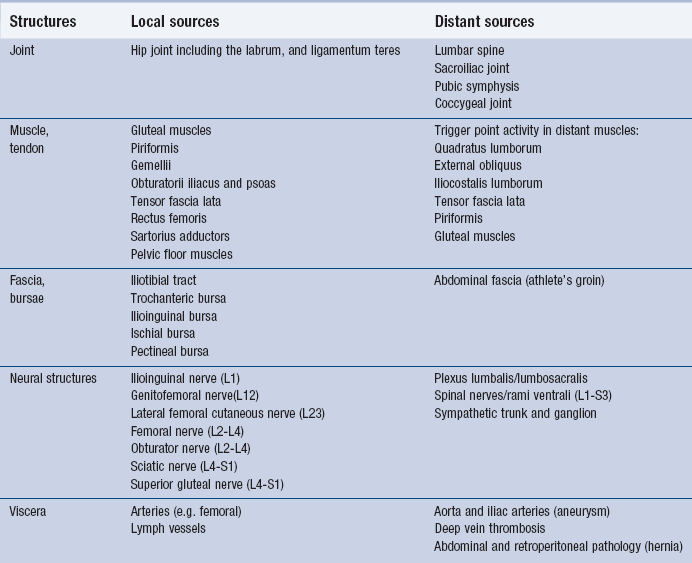
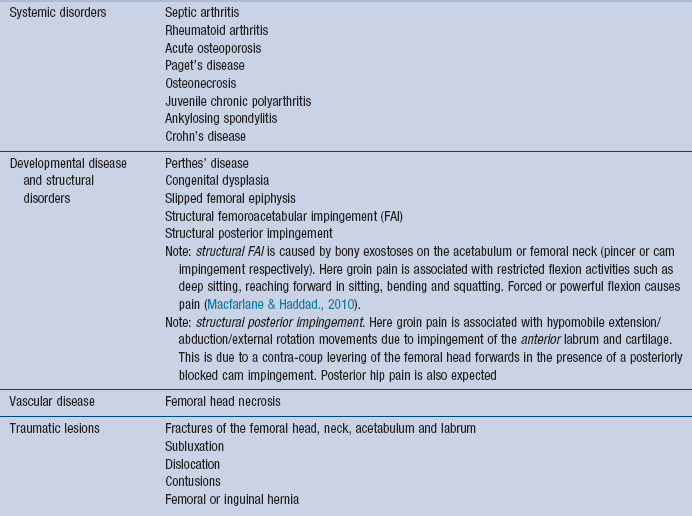
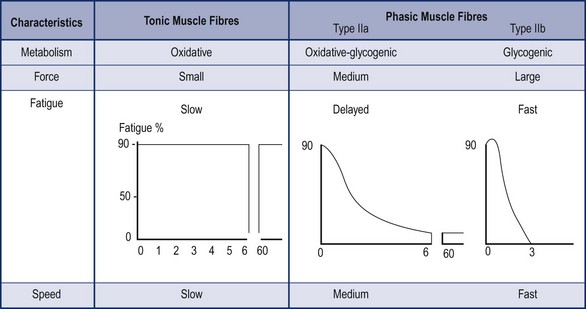
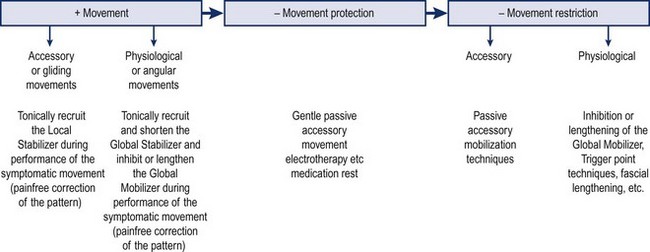
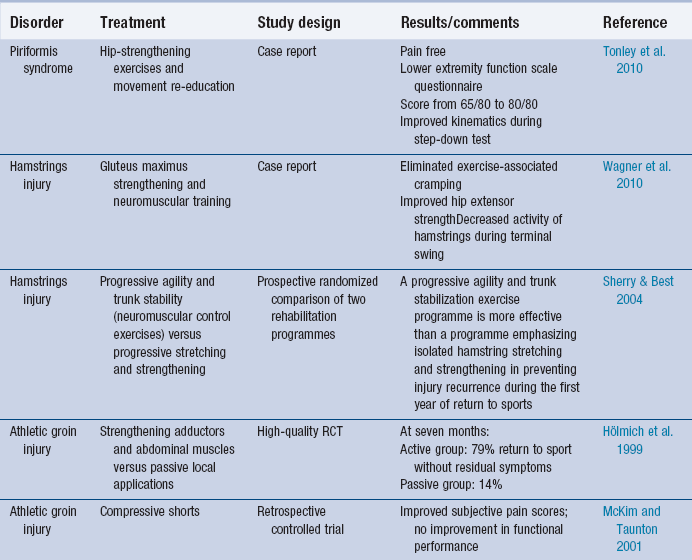
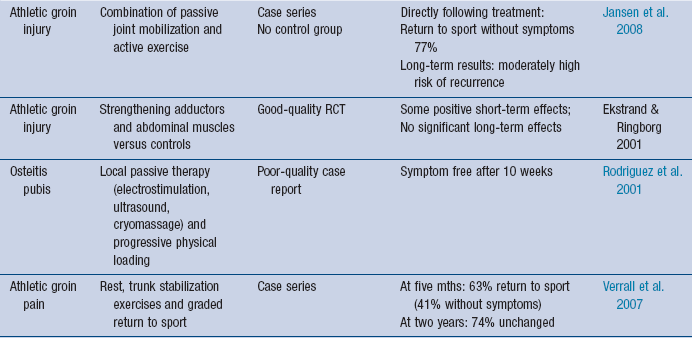
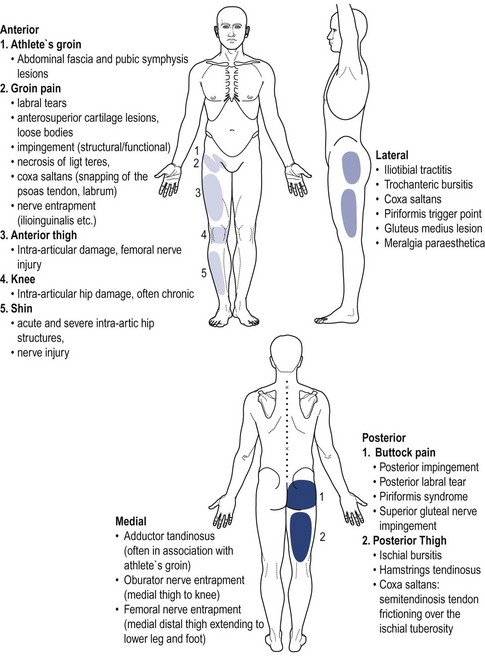
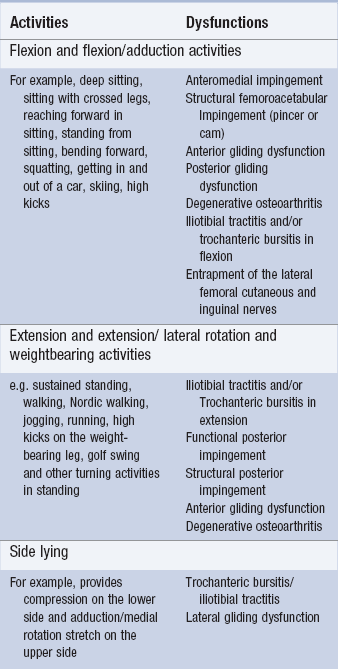
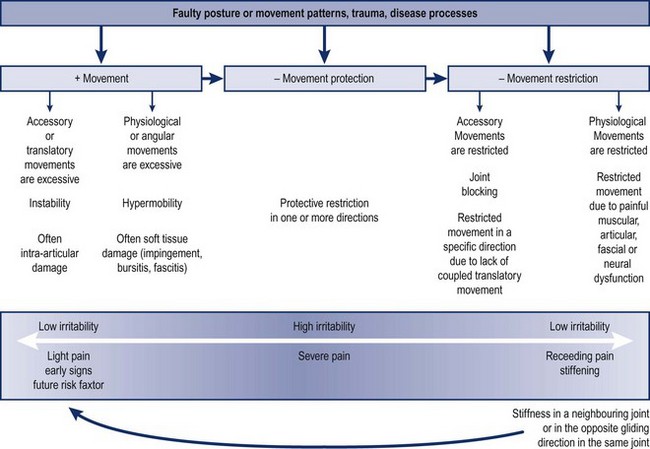
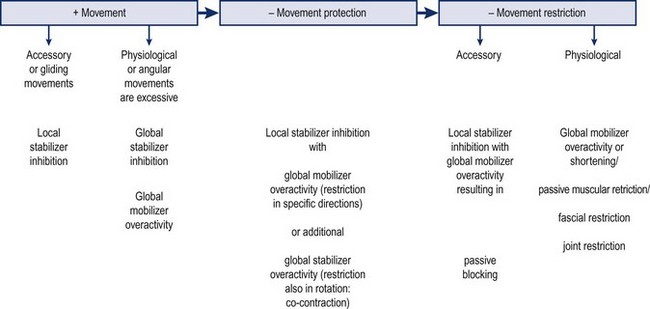
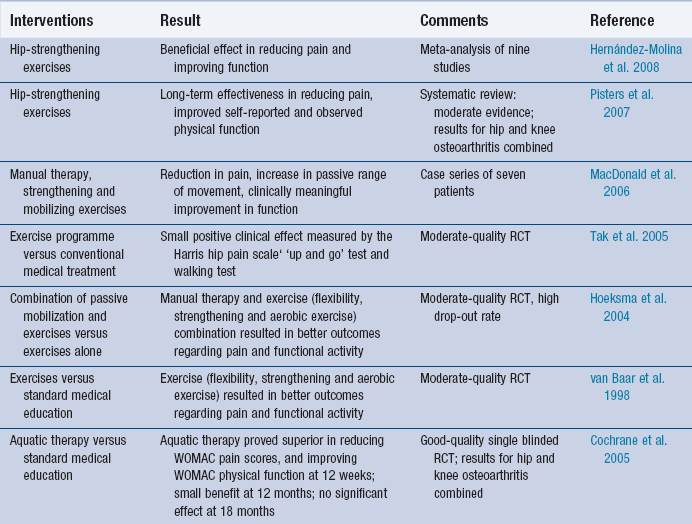
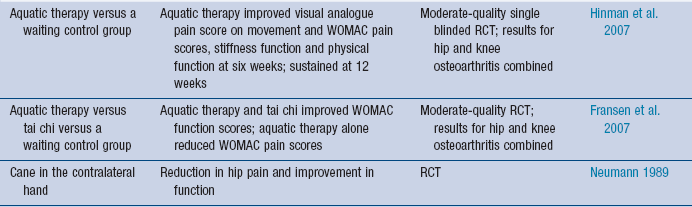
7 Local as well as distant structures capable of referring pain into the hip region are listed in Table 7.1. A knowledge of clinical patterns, differentiation tests and screening procedures will be necessary to distinguish between these structures. These may be divided into movement dysfunctions or overload. 1. Movement dysfunctions: According to Sahrmann (2002), faulty posture and dysfunctional movement patterns are not only the result of pain and pathology but may also cause these lesions. If the symptomatic structure alone is treated (with passive movement, for example) and the dysfunction or ‘cause of the cause’ ( Maitland 1991) is disregarded, symptoms could well reoccur. In fact, in cases of minor instability or impingement, mobilizing gently in the direction of symptoms to decrease pain may meet with limited or short-lived success. If stronger mobilizing techniques progressing into pain are applied symptoms may suddenly increase. This is a clinical indication that functional factors need be addressed. In Table 7.2 a number of disorders are listed where the functional cause assumes particular importance. Table 7.2 Components of hip disorders: functional causes 2. Overload or overuse per se may in time lead to degenerative change or stress fracture. If malalignment is also present then otherwise normal stresses may excessively load one part of the hip joint, the surrounding nerves or myofascial structures. Individuals working at heavy jobs (e.g. furniture movers) or individuals engaged in sports with poor technique or inadequate training procedures (e.g. running on hard surfaces) may subject their joints to overload. Similarly, nerve entrapments such as meralgia paraesthetica are reported to have contributing overload factors: obesity, the wearing of tight jeans and wide belts resulting in compression ( Butler 1991). A range of pathobiological disorders may contribute to movement disorders of the hip ( Table 7.3). These disorders may be categorized as: • Systemic disorders with spontaneous development of acute symptoms. Here medical care is important. • Developmental and structural disorders: both dysplasia and Perthes’ disease may contribute to structural change and the development of femoroacetabular impingement ( Fraitzl et al. 2007, Rab 1999, Friend & Kelly 2009, Li & Ganz 2003), which in turn is said to be implicated in the development of degenerative osteoarthritis ( Ganz et al. 2003, Beck et al. 2005, Bardakos & Villar 2009). Where structural change is present, surgery may be the priority for treatment. • Traumatic disorders where tissue healing times will affect dosage and progression of treatment. In order to organize and prioritize treatment the model in Figure 7.1 developed by the author may be useful. In this model, major categories of dysfunction are shown. These are determined by examining the amount of movement taking place in the symptomatic joint in the main symptomatic direction. For example, the hip or a structure primarily related to hip movement produces symptoms on sitting, squatting or stair climbing. These flexion activities as well as isolated hip flexion would be assessed to determine whether or not the amount of movement is excessive or restricted according to generously standardized expected ranges of movement. Figure 7.1 Integration of structural and functional disorders. Reproduced with permission from Addison (2002). 1. + Movement dysfunction would indicate that the symptomatic movement is excessive or uncontrolled. This dysfunction may be subdivided into excessive physiological (or angular) movement and excessive accessory (or gliding) movement. • + Physiological movement dysfunction. Here the physiological movement is uncontrolled allowing increased end-of-range movement (hypermobility). Excessive physiological movement is generally readily observable. If neighbouring joints in the movement chain are also hypermobile, the hip may not become symptomatic as forces would be shared along the chain. However, if the neighbouring lumbar, sacroiliac and knee joints are stiff then repeated bending movements or forceful hip flexion movements during sport may traumatize the hip leading, for example, to impingement of anterior soft tissues including the labrum. According to Martin et al. (2006), labral tears have been arthroscopically identified – although not in isolation – in 90% of mechanical hip pain. A number of authors link labral damage to the development of capsular laxity and vice versa ( Schenker et al. 2005, Martin et al. 2006), suggesting that better end-range control of this movement may help reduce symptoms as well as recurrences. Other dysfunctions linked to excessive physiological movement have been listed in Table 7.2. • + Accessory movement dysfunction. Here the translatory or gliding movement is uncontrolled resulting in a variable and undependable centre of rotation. This will also affect physiological movement and may be experienced as a lack of ‘through’ range movement control; for example, if the patient attempts to stand on one leg with his hip joint in the ‘physiological’ neutral position (neutral flexion/extension, abduction/adduction, medial rotation [MR] and lateral rotation [LR]), the hip ‘jerks’ or ‘wobbles’ and cannot remain still. These joints may not necessarily exhibit increased end-of-range movement but the ‘neutral zone’ has been shown to be increased ( Panjabi 1992) with subsequent loss of a reliable ‘translational neutral position’ (midposition of three-dimensional translation movements). This may be referred to as ‘stability dysfunction’. In addition, excessive gliding may be associated with increased end-of-range movement in the normally coupled physiological direction. A certain amount of posterior gliding is coupled with hip flexion. If this gliding is excessive the flexion movement may also seem excessive. In fact, the actual angular movement in the joint may be restricted but the disturbed gliding produces a hinge-like gapping movement and a seemingly increased flexion. Alternatively, the condition may elicit protective reactions in the effected direction resulting in decreased range of movement. However, in both situations the increased shearing movements are detrimental to the cartilage as well as irritating to the synovium and are thought to contribute to joint effusion and, in time, osteoarthritis. These joints are classed as ‘unstable’. 2. − Movement dysfunction due to protective reactions. In order to be placed in this category the condition must be ‘irritable’ according to the Maitland Concept definition. In this case, the protective reactions in a single or multiple direction are considered initially necessary. Whether the symptoms are due to acute trauma, to overuse or abuse of the joint, correction of the symptomatic movement would be detrimental at this stage. Once the irritability factor has been reduced, the condition may be reclassified into one of the other categories. 3. − Movement dysfunction due to restriction. This dysfunction may be subdivided into restricted physiological (or angular) movement or restricted accessory (or gliding) movement. • − Physiological movement dysfunction. If specific ranges of movement are not used, adaptive restriction may occur in time. Disuse may result from habitual patterns or protective reactions. Habitual patterns may be due to restricted movement in non-symptomatic neighbouring joints (see the arrow in Figure 7.1). In the case of pathological disorder (e.g. ankylosing spondylosis), protective reactions may be appropriate and some movement restriction unavoidable. In other cases, a restrictive pattern may remain because the patient failed to fully use the joint although the disorder was no longer irritable. • − Accessory movement dysfunction – the blocked joint. If gliding movement (e.g. anterior glide) is excessive in one direction it may in time become restricted in the opposite direction (posterior glide) (see the curve in Figure 7.1). Since hip flexion is coupled with posterior glide, the flexion may become restricted. Patients often describe a bursting feeling at end of range. Muscles may be generally classified into local stabilizers, global stabilizers and global mobilizers according largely to their biomechanical characteristics (see Table 7.4 and Box 7.1). The classification of lumbar and hip muscles is shown in Box 7.2. Table 7.4 Biomechanical characteristics of global stabilizers and global mobilizers Muscle imbalance and associated dysfunctions are illustrated in Figure 7.2. From this it may be postulated that pain due to excessive gliding movements in the hip (irrespective of whether physiological movements are hypermobile or restricted) will require better recruitment of the local stabilizers as treatment. For selective physiological movement in a joint it is important that the global stabilizers work efficiently. If physiological hip movement is excessive due to inhibition of the global stabilizers with multi-joint global mobilizers dominating, then the hip – relative to other joints above and below along the movement chain – will move excessively. Hence hypermobility disorders require global stabilizer recruitment/shortening and mobilizer inhibition/lengthening. Figure 7.2 Muscle imbalance and associated dysfunctions. Reproduced with permission from Addison (2002). By irritable disorders the local stabilizers may be tonically inhibited (see ‘ Motor Control’ below). Here it is necessary that the capsule can expand to cope with excessive intra-articular swelling. Co-contraction or protection provided by the global muscles will ensure that the joint is temporarily spared. However, the joint will receive little proprioceptive input making it more difficult to recruit the local stabilizers particularly if this situation is maintained once pain and swelling have subsided. For adequate motor control the appropriate muscle fibre type should be recruited. All human muscles contain tonic and phasic muscle fibres. Characteristics of these muscle fibres are shown in Figure 7.3. The presence of pathology also inhibits tonic fibre activity in the local stabilizers and interferes with timing of their contraction. Pain or swelling have been shown to delay their activity ( Stokes & Young 1984). For detailed information on the selection and progression of treatment techniques with passive mobilization see Chapter 1 of Hengeveld and Banks (2014). The following suggestions summarized in Figure 7.4 integrate functional factors. • If the disorder is irritable or severe and the pain mechanism is nociceptive, gentle passive accessory movement (particularly distraction and rotation techniques) may be used for pain modulation and to help in dispersing swelling. Protective deformities may temporarily be advantageous. Medication and rest – including the use of walking aids – may be necessary. • If the disorder is not irritable or severe, the following guidelines may help determine treatment priorities: In restricted joints where compressive force is related to symptom production the use of compression may at some stage be incorporated into treatment. Maitland (1991) suggests that mobilizations with compression may stimulate synovial fluid flow and improve cartilage nutrition, which may be important in the early stages of osteoarthrosis. The peripheral anterior surface of the femoral head is a common site of cartilage lesions (Bullough et al. 1973 cited in Sims 2003). Sims (2003) states that this area will contact in internal rotation and adduction and suggests that this may explain the beneficial effects of the hip flexion–adduction technique. Patients with osteoarthritis are the most commonly referred single group for physiotherapy. Table 7.5 lists evidence-based recommendations for treatment. Table 7.5 Evidenced-based interventions for osteoarthritis RCT = randomized control trial, WOMAC = Western Ontario and McMaster Universities Arthritis Index ( Royal Australian College of General Practitioners (2009), Cibulka (2009), Zhang et al. (2008)) In the case of soft tissue injury (including labral injury), there is growing interest in the effects of neuromuscular training as opposed to stretching or strengthening training. Labral tears, for example, have been related to forceful external rotation particularly in sports and activities such as golf, soccer and dancing. According to Martin et al. (2006), labral tears have been arthroscopically identified – although not in isolation – in 90% of mechanical hip pain cases. A number of authors link labral damage to the development of capsular laxity and vice versa ( Schenker et al. 2005, Martin et al. 2006), suggesting that better end-range control of this movement may help reduce symptoms as well as recurrences. Some evidence largely from case reports is listed in Table 7.6 to support neuromuscular training and movement re-education (particularly the activation of the appropriate global stabilizers) for various hypermobility dysfunctions. In the subjective examination, ‘making features fit’ ( Maitland 1991) is important: a given hypothesis should take on form from different pieces of information in the subjective examination and confirmation should be sought in the physical examination. 1. Patients may present with the main problem being pain which significantly limits daily life activities. This gives some indication of the severity or irritability of the disorder. However, perceived pain should bear some relation to perceived disability – high reports of pain coupled with only limited disability may represent a psychosocial risk factor hindering recovery to full function. Similarly low pain reports may be linked to considerable disability. In fact, where patients have learned to live with their pain by restricting activity, the irritability factor may be underestimated. Such patients may have some pain or discomfort after walking, gardening or driving a car, but if they prolong the activity, they may suffer acute exacerbation 2. Patients may report limitations in daily activities due to large restrictions of range of motion with associated pain being less of a problem. Soames (2003) lists the required range of movement for specific activities as follows: Magee (2008) gives differing measures. This can be due to a number of factors such as stair and sitting heights and according to the degree of compensation allowed in surrounding joints. For example, tying shoes requires 50° flexion ( Soames 2003) but 120° flexion according to Magee. It would be expected that Soames’ patients are compensating to a greater extent in neighbouring joints. However, this increased load on surrounding structures may injure them. In fact, the whole lower quadrant movement system is at risk of becoming symptomatic if further impairment of joint mobility occurs. Typical pain patterns and associated hip dysfunctions are delineated in Figure 7.5. The ‘C’ sign – demonstrating the area of pain by holding around the hip with fingers anteriorly and thumb posteriorly – is thought to be indicative of intra-articular pathology, for example, arthritis, cartilage and labral damage, necrosis of ligamentum teres, etc. ( Magee 2008). In particular, pain due to degenerative arthritis is often dull deep and aching frequently referring vaguely to the anterior thigh and/or knee ( Wroblewski 1978, Poppert & Kullig 2011). Lesions in the anterior superior labrum-cartilage zone are likely to be confined to the groin and to be sudden, sharp and stabbing on weight bearing ( Liebold et al. 2010). If radiating tingling or burning pain is present, nerve entrapment should be considered while inflamed fascia (iliotibial tract) may also produce burning pain or a ‘numb feeling’ without true numbness being present. Painful snapping and weakness should also be noted. Clinical patterns may be related to: Where trauma is involved, the mechanism of injury may give important information: • Before posterior gliding dysfunction (see Table 7.7) is implicated, a dashboard or similar injury with posterior subluxation of the hip is sought in the history. • A fall on the outside of the trochanter may result in lateral soft tissue injury, medial cartilage injury ( Magee 2008) or fractures depending on the forces involved. Particularly in older patients, osteoporosis may be considered. Musculotendinous lesions are often directly related to trauma ( Agre 1985). If no obvious trauma is present: • Repeated forceful end-of-range loading may play a role in the more insidious overall development of symptoms. This is typical in sports and activities such as football, martial arts, ballet and golf. • An assumed relatively sudden onset due to twisting movements on one leg may be indicative of labrum tears ( Sims 1999) or local muscular or ligamentous lesions. Hamstring injury, for example, is likely to result from rapid forceful change from concentric to eccentric activity ( Verrall et al. 2001) and is likely to reoccur in 34% of cases ( Croisier 2004). • Overuse and misuse of the structures may lead to the gradual development of symptoms over time with little initial interference in daily life activities. Gardening in excessive hip flexion (jackknife position) rather than sharing the flexion proportionally over the knee and spine will gradually stress the hip region. • Walking with poor motor control at the hip is a further example ( Gunn 1980, Weinstein 1992). If excessive hip movement compensates for stiffness or pain in neighbouring joints, the course of symptoms over time may shift from an initially painful lumbar spine or knee to the hip. The importance of correcting compensations as soon as pain and injury levels allow is therefore clear. Moreover, an originally one-component movement disorder in the lumbar spine, pelvic or hip region may develop into a multi-component disorder over the course of years ( Ekberg et al. 1988). For example, poor motor control of the pelvic girdle may be associated in time with a symptomatic sacroiliac joint and pubic symphysis, with irritation of weak abdominal fascia and associated adductor tendinosis ( Hölmich 1999). Similarly, complications while giving birth may produce pelvic muscle lesions and asymmetries affecting the entire hip and pelvic region producing long-term debilitating symptoms ( Hungerford et al. 2004). Such factors need consideration when planning the first one to three sessions of the physical examination. In the past history, developmental disorders may have been diagnosed. Dysplasia (particularly in girls) has been shown to develop in later life into femoroacetabular pincer impingement and Perthes’ disease or epiphysiolysis of the femoral head (more often in boys) can develop into femoroacetabular cam impingement ( Ganz et al. 2003). These structural impingements may initially present as intermittent groin pain which increases with high demands on the joint or from activities such as sustained deep sitting ( Leunig & Ganz 2005). • As well as routine information about the patient’s general health, weight loss, radiographic findings, medication intake, etc., particular attention needs to be given to screening questions regarding urogenital and intestinal functions ( Boissonnault 1995, Goodman & Snyder 2000). • In particular where symptoms do not seem to be directly related to movement functions these screening procedures must be taken into consideration.
Management of hip disorders
Introduction
Components of hip disorders
Structural sources
Functional causes (contributing factors)
Functional cause
Disorder
Hypermobility dysfunctions
Global muscle imbalance
Functional anterior or anteromedial impingement
Groin pain associated with hypermobile flexion or combined flexion-adduction movements (the high kicks of ballet and martial arts) resulting from a lack of deceleration force from antagonistic muscles such as the deep gluteus maximus or posterior gluteus medius (global stabilizers)
Functional posterior impingement
Buttock pain associated with hypermobile extension/abduction/external rotation movements due to impingement of the posterior labrum and posterior soft tissues. The superior gluteus maximus (global mobilizer) is overactive; the iliacus and the short adductors (global stabilizers) are inhibited
Iliotibial tractitis and/or trochanteric bursitis in flexion
Discomfort or stretching/burning pain in the superior gluteus maximus muscle or it’s fascia (lateral hip) with restriction of flexion or combined flexion-adduction activities. Superficial gluteus maximus is overactive or shortened. Confined sitting will produce unavoidable stretch in the muscle if the patient is unable to flex the lumbar spine (lack of knee room) or abduct the hips. Deep turns during skiing and lying on the affected side (compression of soft tissue) or non-affected side (stretching) may also irritate this condition
Iliotibial tractitis and/or trochanteric bursitis in extension
Lateral hip pain associated with repeated extension/rotation activities such as jogging. It results from an overactive tensor fascia lata (global mobilizer) pulling the iliotibial tract forwards over the trochanter. The posterior gluteus medius (global stabilizer) is inhibited. It may be aggravated by lying on the affected or non-affected side
Entrapment of the lateral femoral cutaneous and inguinal nerves
Lateral thigh or groin pain on sustained excessive flexion particularly in obese individuals or those with wide hips, may cause nerve compression and irritation
Athlete’s groin
Pain may be widespread over the pubic symphysis, groin, medial thigh and sacroiliac joint or restricted to the falx region adjacent unilaterally to the pubic symphysis. Global stability dysfunction in the pelvic ring as a whole is often involved, associated with inadequate fascial covering in the falx region of the lower abdomen. Pain may be aggravated by forceful rotation movements, stop–go activities or forceful sit-ups
Ischial bursitis/bicipital tendinosus, bursitis, muscle tears (especially in the adductors, psoas and biceps femoris muscles and their associated bursae)
Local pain in the affected structures often associated with pelvic stability dysfunction in the presence of overactive hip muscles seeking to provide stability, particularly during forceful stop-go activities
Restrictive dysfunctions
Degenerative osteoarthritis
Groin pain or generalized pain associated with weight-bearing (joint surface compression) and end-of-range activities (capsular tightness). Hence restrictions may be present in deep sitting, sitting with crossed legs and getting in and out of a car. In particular, multiple movement directions may be restricted rather than single directions
Excessive intra-joint gliding (minor instabilities)
Local muscle imbalance
Inhibition of tonic activity in psoas, the gemelli and the obturatorii as a unit
Anterior gliding dysfunction
Often unspecific or sometimes sharp groin pain due to generalized synovitis or stretch /impingement of anterior structures. Joint blocking may occur if the femoral head remains in an anterior position so that normal coupling of posterior gliding with physiological flexion cannot take place. Open-chain flexion movements (e.g. during stair climbing) may result in labral, chondral and other soft tissue irritation, including iliopsoas tendinopathy. Inhibition of psoas (local stabilizer responsible for tightening the capsule and hence preventing it’s impingement) is one of the features of this dysfunction. During open and closed chain extension activities anterior structures will also be stressed. The patient may also avoid trunk movements involving hip lateral rotation in standing
Posterior gliding dysfunction
Buttock pain due to excessive posterior gliding within the joint. Flexion or flexion/adduction movements may be limited due to reactive inhibition and apprehension (fear of posterior subluxation). The patient may avoid sitting or squatting or sit on one buttock with the affected hip in extension over the side of the seat. Standing and lying supine with the affected hip in slight abduction and lateral rotation are preferred positions. It occurs often in association with trauma, e.g. dashboard injury or landing on a hard surface by long-jump
Lateral gliding dysfunction
Generalized pain or lateral pain standing on one leg with adducted (hanging) hip or when lying on the non-affected side. Tonic activity in psoas, gemelli and obturatorii as a unit is lacking. This condition may be found in combination with hip dysplasia
Pathobiological disorders
Applied theory
Integration of structural and functional disorders
Muscle classification and associated muscle imbalance
Muscle classification
Global stabilizers
Global mobilizers
One joint
Two-joint or multi-joint
Deep
Superficial
Direction of pull produces joint compression
Direction of pull: movement-orientated
Muscle length: long
Muscle length: long
Force vector + force lever optimal for joint compression (minimal muscle mass or muscle strength necessary)
Force vector + force lever optimal for large range of movement, speed, acceleration and joint distraction (large muscle mass/muscle force necessary)
Muscle fibres are broad and take an oblique course (shock-absorbing)
Muscle fibres take a linear course (strength is maximally directed)
Control of rotation – especially decelerating
Produce strong flexion/extension (largely aligned in the sagittal plane)
Control of physiological movement in a particular peripheral joint (responsible for selective movement) or the form of the curve in a vertebral section
Produces movement along the length of the movement chain and is therefore relatively non-selective
Muscle imbalance and associated dysfunction
Motor control
Treatment principles
 Where excessive physiological movement (hypermobility) is found in the symptomatic direction active stabilizing exercise may be the treatment of choice (e.g. better end-range control of lateral rotation for specific labral lesions, or athlete’s groin). If pain occurs during low-level activity, correcting the movement pattern by tonically recruiting and shortening the global stabilizer and inhibiting overactivity in the global mobilizer will help achieve a pain-free movement pattern. For excessive lateral hip rotation, for example, recruiting the anterior gluteus medius and minimus and the short adductors while inhibiting the piriformis and superior gluteus maximus may achieve this aim.
Where excessive physiological movement (hypermobility) is found in the symptomatic direction active stabilizing exercise may be the treatment of choice (e.g. better end-range control of lateral rotation for specific labral lesions, or athlete’s groin). If pain occurs during low-level activity, correcting the movement pattern by tonically recruiting and shortening the global stabilizer and inhibiting overactivity in the global mobilizer will help achieve a pain-free movement pattern. For excessive lateral hip rotation, for example, recruiting the anterior gluteus medius and minimus and the short adductors while inhibiting the piriformis and superior gluteus maximus may achieve this aim.
 If the hip is compensating with excessive movement for restriction in neighbouring joints these joints can be mobilized at some stage (e.g. excessive hip external rotation during a golf swing may compensate for lumbar spine or knee rotational restrictions).
If the hip is compensating with excessive movement for restriction in neighbouring joints these joints can be mobilized at some stage (e.g. excessive hip external rotation during a golf swing may compensate for lumbar spine or knee rotational restrictions).
 Where excessive gliding movement (minor instability) contributes to dysfunction in the symptomatic direction, pain-free tonic recruitment of the segmental stabilizers while maintaining normally painful positions and performing normally painful activities may help restrain excessive gliding. Similarly, passive accessory mobilization in the opposite direction to pain may be necessary if this direction has become stiff.
Where excessive gliding movement (minor instability) contributes to dysfunction in the symptomatic direction, pain-free tonic recruitment of the segmental stabilizers while maintaining normally painful positions and performing normally painful activities may help restrain excessive gliding. Similarly, passive accessory mobilization in the opposite direction to pain may be necessary if this direction has become stiff.
 Where restriction in the coupled gliding direction is found to block the physiological movement, passive accessory joint mobilization, may be the treatment of choice. Because gliding and physiological movements are coupled (Matles 1975, Simoneau G, Hoenig K Lepley J et al 1998 cited in Sims (2003), mobilizing an accessory movement such as posteroanterior glide may restore extension movement. Sims (2003) states that the migratory ‘up and out’ presentation of osteoarthrosis may lack longitudinal caudal motion whereas the medial migratory presentations may lack lateral gliding motion.
Where restriction in the coupled gliding direction is found to block the physiological movement, passive accessory joint mobilization, may be the treatment of choice. Because gliding and physiological movements are coupled (Matles 1975, Simoneau G, Hoenig K Lepley J et al 1998 cited in Sims (2003), mobilizing an accessory movement such as posteroanterior glide may restore extension movement. Sims (2003) states that the migratory ‘up and out’ presentation of osteoarthrosis may lack longitudinal caudal motion whereas the medial migratory presentations may lack lateral gliding motion.
 Restriction in physiological movement may be helped by a combination of muscle lengthening, trigger-point techniques or fascial techniques, etc.
Restriction in physiological movement may be helped by a combination of muscle lengthening, trigger-point techniques or fascial techniques, etc.
Evidence supporting practice
Subjective examination
Main problem (‘Question 1’)
Areas of symptoms (body chart)
Behaviour of symptoms
 according to Maitland et al. (2001), an intra-articular disorder with a degree of inflammation might be suspected if symptoms are more constant in their behaviour, are perceived as deeply localized and more restricting in daily life activities and if regular changes in resting positions are needed. Systemic inflammatory disease such as rheumatoid arthritis may occur more spontaneously and episodically with morning pain and stiffness lasting longer than an hour. Concomitant multi-joint involvement is a feature.
according to Maitland et al. (2001), an intra-articular disorder with a degree of inflammation might be suspected if symptoms are more constant in their behaviour, are perceived as deeply localized and more restricting in daily life activities and if regular changes in resting positions are needed. Systemic inflammatory disease such as rheumatoid arthritis may occur more spontaneously and episodically with morning pain and stiffness lasting longer than an hour. Concomitant multi-joint involvement is a feature.
 labral tears: here forceful rotation is often involved and may be accompanied by a clicking sensation in the groin.
labral tears: here forceful rotation is often involved and may be accompanied by a clicking sensation in the groin.
 Tendinopathies and muscle lesions: pain is clearly pinpointed by the patient and reproduced on stretching or contracting the muscle or during stop-and-go activities ( Agre 1985).
Tendinopathies and muscle lesions: pain is clearly pinpointed by the patient and reproduced on stretching or contracting the muscle or during stop-and-go activities ( Agre 1985).
 Joint surface of the hip: reproduction of symptoms occurs during weight-bearing activities, particularly sustained standing. Sudden loading of the joint surface, for example, when moving out of sustained positions such as sitting may also produce symptoms ( Arnold et al. 1972).
Joint surface of the hip: reproduction of symptoms occurs during weight-bearing activities, particularly sustained standing. Sudden loading of the joint surface, for example, when moving out of sustained positions such as sitting may also produce symptoms ( Arnold et al. 1972).
 Capsular tightness: end-of-range movements may aggravate symptoms.
Capsular tightness: end-of-range movements may aggravate symptoms.
 Fascia: under tension, burning or prickling symptoms may occur.
Fascia: under tension, burning or prickling symptoms may occur.
 Nerve entrapment (e.g. meralgia paraesthetica): burning pain during the night is typical.
Nerve entrapment (e.g. meralgia paraesthetica): burning pain during the night is typical.
 The symptomatic activity and subsequent analysis of the movement direction together with type and area of symptoms ( Fig. 7.5) will help establish the dysfunction. It also helps the therapist focus on the movement direction requiring careful assessment and later treatment. Direction-specific aggravating activities with their typical movement dysfunctions are listed in Table 7.7.
The symptomatic activity and subsequent analysis of the movement direction together with type and area of symptoms ( Fig. 7.5) will help establish the dysfunction. It also helps the therapist focus on the movement direction requiring careful assessment and later treatment. Direction-specific aggravating activities with their typical movement dysfunctions are listed in Table 7.7.
History
Special questions and medical screening questions
Management of hip disorders