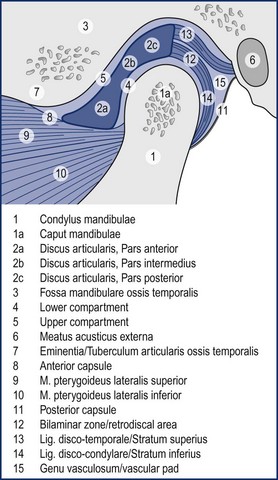
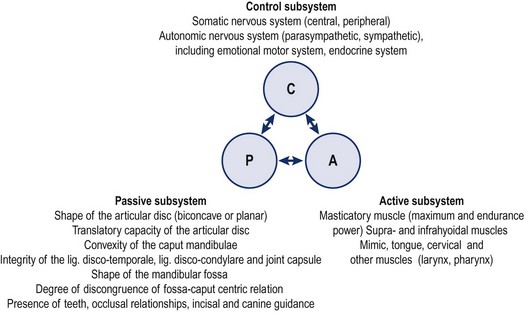
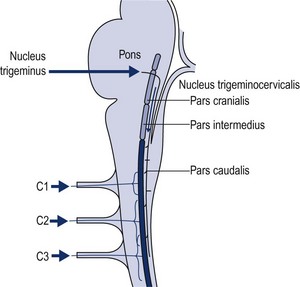
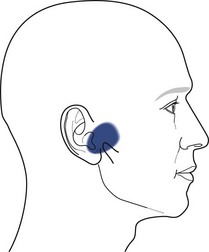
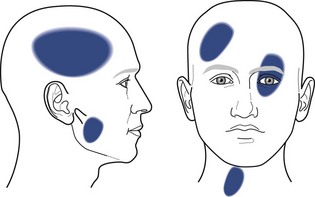
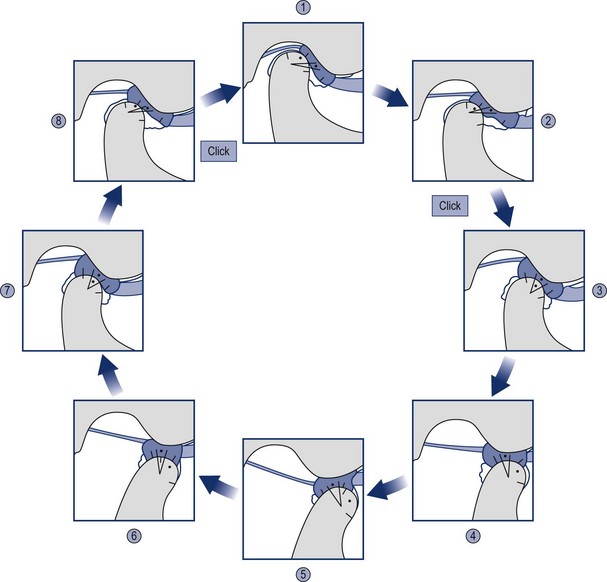
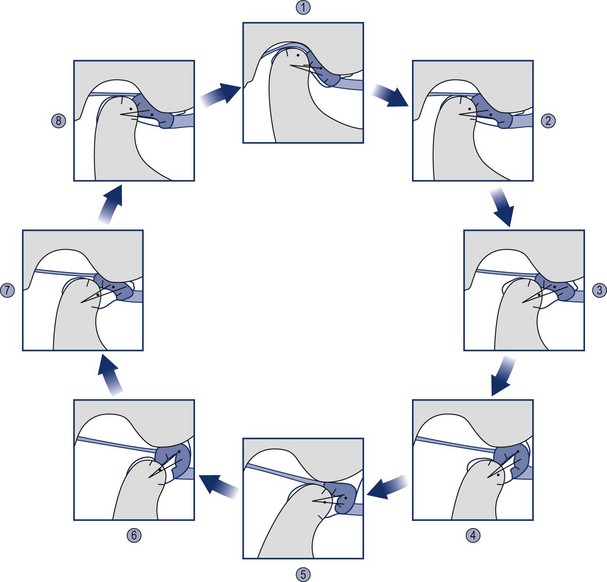
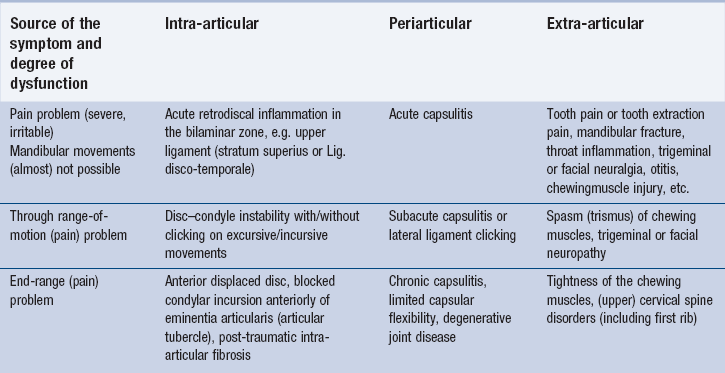
3 Finally, women in their reproductive years suffer up to four times more from craniomandibular dysfunctions than men ( LeResche et al. 1997, Cairns et al. 2003). There are several accepted explanations for this. There are differences in stress coping between men and women. Female hormonal factors, such as the effects of oestrogen, play a role in pain threshold and intensity before the menopause and women’s chewing muscles have less endurance and less force than those of men. Specific factors that only affect women should be considered in the management of dysfunctions, for example, changing contraceptives or applying appropriate relaxation modalities. These can be decisive factors in the long-term success of treatment. For comprehensive theoretical information the reader should refer to anatomical, biomechanical, dental and orthodontic textbooks (e.g. Ide et al. 1991, Fitzgerald 1992, Kraus 1994, Okeson 1985, 1996, 1998). Selected areas are explored in this chapter to give some insight into the most common dysfunctional, pathological conditions. • The fossa of the temporal bone articulates with the mandibular head, which is elliptical and mushroom-shaped. Its cartilage is fibrous, not hyaline, and undergoes remarkable changes in shape in the course of an arthropathy (Müller et al. 1992ab). • The anterior capsule is attached approximately 4.4 mm (standard deviation 1.7 mm) anteriorly of the eminentia articularis (articular tubercle) ( Johansson & Isberg 1991), allowing the mandibular head to move beyond the tubercle. The joint partners are not congruent and movement and position of the mandibular head is aided by the articular disc. The disc is a three-dimensional, biconcave, hat-shaped cartilage structure with thick anterior and posterior parts as well as a thin intermediate part, which divides the joint into two compartments with two different movement tasks. • The posterior border of the disc is aligned on top of or even slightly anterior to the mandibular head (11 or 12 o’clock position in radiological terms). The physiological position of the mandibular head in the temporal fossa in a closed mouth position with maximum intercuspation (full teeth contact) is defined by the concept of centric relation (CR): most anterior, most cranial and midway between medial and lateral, with the disc in its correct position ( Schimmerl et al. 1993, Bumann & Lotzmann 2000). It is estimated that 85% of the entire population show a different condyle fossa position in habitual occlusion, called centric occlusion (CO). In dentistry it is a major task to maintain or to restore the centric relation. Note that the normal resting position of the mandible in a closed mouth situation is slightly discluded (upper postural position of the mandible, UPPM), indicating the proprioceptive abilities of the stomatognathic organ ( Kraus 1994). • A main function of the lateral pterygoid muscle is to control fossa-disc-condyle stability in rest and during movements. The muscle acts as a fine-tuning, balancing, local stabilizing muscle ( Osborn 1995a, Langendoen 2004, Phanachet et al. 2003, 2004). There is experimental two-dimensional evidence that the DA moves passively over the condylus ( De Vocht et al. 1996) and that activity of the lateral pterygoid muscle is not required. • In dentistry, the retrodiscal intra-articular area is called bilaminar zone (BZ). It contains synovial fluid, the genu vasculosum, a vascular pad acting as an artero-venous shunt during mouth movements and which has significant inflammatory potential as well as two ligaments ( Schimmerl et al. 1993). • The upper ligament, the Lig. disco-temporale or stratum superius, can be folded and lengthened, enabling translation of the disc-condyle complex in the upper joint compartment. The ligament is anchored in the permeable petro-tympanic fissure, containing fibres of the chorda tympani and may be the explanation for a type of tinnitus in temporo-mandibular arthropathies. • The lower ligament, the Lig. disco-condylare or stratum inferior, is non-elastic, remains the same length during movements, thus preventing translation in the lower joint compartment, which is designed for rotation only ( Rees 1954, Dauber 1987, Bumann et al. 1991, Eckerdal 1991, Scapino 1991, Rodríguez-Vázquez et al. 1993, Wilkinson & Crowley 1994, Chiarini and Gajisin 2002, Linsen et al. 2006). • Therapeutically, the above implies that anterior-posterior, posterior-anterior and longitudinal cranial accessory movements of the mandible are contraindicated treatment directions in by far the majority of articular TMD cases. • The innervation of the TMJ and the masticatory muscles is supplied by auriculotemporal, masseteric and buccinator end branches of the mandibular branch (NV3) of the trigeminal nerve (CN5). The trigeminal nerve complex plays a major role in sensory innervation of almost all craniofacial structures, is connected with several other cranial nerves (facial, vestibulocochlear, glossopharyngeal, vagus nerves) and its relevance is further outlined below ( Fig. 3.1). • The five axial movements of the mandibula are called: • Due to the Siamese twin construction both joints move at the same time, symmetrically or asymmetrically. • Depression, protrusion and laterotrusion are excursive movements as the disc-condyle complex can move beyond the anterior tubercle, whereas the returning movements of the disc-condyle complex into the fossa are named incursive. Although most patients complain of excursive movements, the cause of the dysfunction is often due to a-physiological incursive movement such as a preliminary occlusal contact of two molars. • The functional chewing movement is a three-dimensional event with a favourite chewing side and a contralateral balance side. • Arthrokinematically the joint shows at depression: initial rotation of the mandibular head in the lower compartment is gradually followed by anterior translation of the disc-condyle complex over the joint surface of the fossa in the upper compartment (Piehslinger et al. 1993, 1994, Ferrario et al. 2005, Mapelli et al. 2009). Limited upper compartment translation is a recognized major etiological factor in the onset and development of an arthropathy. • Increased intra-articular pressure, for example, due to a physiological compression, makes the disc act like a suction cup, inducing a vacuum between its intermediate part and the fossa ( Nitzan & Marmary 1997). • Another simultaneous or subsequent factor is a compensatory physiological translation in the lower compartment, commonly occurring in cases of underdevelopment of the antero-posterior size of the mandibular head, which negatively extrapolates the fossa-caput discongruence (Müller et al. 1992ab). The latter is one more reason to avoid anterior-posterior or posteroanterior accessory movements, whereas longitudinal caudad distraction, manually, with a continuous distraction splint (for approximately six months) and subsequent dental restoration, seem the appropriate management for most arthropathies ( Hugger et al. 2004, Linsen et al. 2006). • The mandibular heads’ fibrous cartilage enables gradual rebuilding from a rounded shape to an anterocaudad slope, induced by pathological translation in the lower compartment. This is considered a major component in arthropathies such as disc instabilities. • As the anteroposterior diameter of the mandibular head cannot be influenced therapeutically, other components, as outlined in Panjabi’s stability model (Panjabi 1992ab) are challenged to compensate. • Panjabi’sstability model consists of three interacting subsystems: the passive, the control and the active ( Fig. 3.2). • The passive subsystem in relation to the temporomandibular complex contains the joint surfaces of the temporal fossa and mandibular head, the anterior and posterior capsule, the extra-, peri- and intra-articular ligaments, the articular disc and all teeth (occlusal component). Occlusal faults such as a lack of molar disclusion in the resting position of the mandible, preliminary molar contact at incursive movements, lack of incisive guidance at anterior as well as lack of canine guidance at lateral movements or a lack of posterior support due to loss of molars ( Dulcic et al. 2003) are all considered relevant causal factors for dysfunction and can be dentally managed. • Further deficits of the passive subsystem are recognized being relevant factors in TMD, for example: • All this can be compensated within the limits of physiological tolerance by adequate functioning of the other subsystems and remains subclinical. If the limits of structural tolerance are exceeded, for example, by distress factors, the system will decompensate (Okeson 1985, 1996, 1998, Hansson et al. 1987). • Distress factors can be categorized within the concept of the control subsystem. The control subsystem for the craniofacial complex contains many parts of the peripheral and central somatic nervous system (SNS) and autonomic nervous system (ANS), such as: • Peripheral course of cranial (primarily trigeminal, facial, glossopharyngeal, vagus, accessory, hypoglossal) and cervical nerves from the cervical plexus and upper cervical posterior rami including autonomic gangliae as well as the sympathetic trunk ( Pedulla et al. 2009). • Central nervous system parts with motor nuclei in the brainstem (the truncus cerebri contains pons, mesencephalon, medulla oblongata) and upper cervical myelum, including the nucleus trigeminocervicalis (spinal sensory nuclei of the trigeminal nerve) ( Price et al. 1976, Sessle et al. 1976, Bushnell et al. 1984, Kojima 1990, Widenfalk & Wiberg 1990, Fitzgerald 1992, Neuhuber 1998, Imbe et al. 1999, Iwata et al. 1999, Gibson & Zorkun 2008). • The latter receives nociceptive and thermal trigeminal as well as facial, glossopharyngeal and vagal input and its caudad part expands at least to the C3 segment. • Within the spinal trigeminal nucleus, information is represented in an onion skin fashion. The lowest levels of the nucleus, the pars caudalis in the upper cervical cord and lower medulla, represent peripheral areas of the face (scalp, ears and chin). Clinically, this is the most commonly affected area in TMD patients and so it is important to include the upper cervical spine in the assessment and management of TMD ( Clark et al. 1987, Browne et al. 1998, Friedman & Weisberg 2000, Huelse M 1998, Reisshauer et al. 2006, Toti et al. 2010). Higher levels in the upper medulla, the pars intermedius, represent more central areas (nose, cheeks, lips). The highest levels in the pons, the pars cranialis, represent the mouth, teeth, and pharyngeal cavity ( Figs 3.3 and 3.4). Figure 3.3 Spinal sensory nuclei of the trigeminal nerve for thermal and nociceptive afferences: nucleus trigeminocervicalis, pars cranialis, intermedius and caudalis. Figure 3.4 Representation of facial areas in the nucleus trigeminocervicalis. 1. Pars cranialis: mouth, teeth, pharyngeal cavity. 2. Pars intermedius: nose, cheek. 3. Pars caudalis: scalp, ears, chin. • Trigeminal, facial and vagus motor nuclei are directly influenced by the limbic system, also known as the Emotional Motor System (EMS) ( Holstege et al. 1996; Holstege 2001, van der Horst et al. 1997, 2001, Gerrits et al. 1999, 2004, Mouton et al. 2005). • Distress-induced limbic system activity, for example, resulting from the amygdala, nucleus retroambiguus or the periaqueductal grey) can activate several descending motor pathways causing: • The EMS offers, in the absence of direct peripheral nervous connections, an explanation for the reflectory Meersseman phenomenon ( Esposito & Meersseman 1988, Huelse & Losert-Bruggner 2002, Entrup 2009, Fischer et al. 2009) that malocclusion, limited mandibular depression and limited length of some pelvic muscles correlate. • The EMS is clearly demonstrated by football and hockey coaches during matches. Chewing gum may increase alertness and reduce stress ( Tahara et al. 2007, Hellhammer et al. 2009, Scholey et al. 2009, Smith 2010, Johnson et al. 2011) demonstrating that parafunctional habits, to a certain extent, are a useful congenital strategy to cope with stress ( Slavicek & Sato 2004). • Panjabi’s model can be used to address a major question in dentistry ‘How much occlusion do we need?’ Whereas persons with positive interactions between the three subsystems can easily deal with a suboptimal occlusion, patients with further dysfunctions (of the passive subsystem: hypermobility, small mandibular condyle, of the control subsystem: excessive parafunctional habits of the active subsystem: weak muscles) need the best possible occlusal relationships (Okeson 1985, 1996, 1998, Hansson et al. 1987). The model also confirms the recognized necessity for interdisciplinary cooperation. • Psychological factors, being part of the control subsystem, are generally considered relevant in TMD ( Stam et al. 1984, Dworkin et al. 1990, Dworkin & LeResche 1992, Suvinen et al. 1997, Auerbach et al. 2001, Dworkin et al. 2002, Rantala et al. 2003, Ohrbach et al. 2010). • Stress coping and management of stress-induced complaints are a common component of the overall management plan and may include splint, cognitive behavioural, pharmacological, body-mind and physical therapy. The role of the physiotherapist in this field may vary from applying local massage or electrotherapy to relax chewing muscles, individual body-mind therapy such as craniosacral therapy, bio- and myofeedback with breathing procedures, to group therapies with a social character such as yoga, qi gong, or meditation classes. • Relaxing effects on the autonomic nervous system can be monitored with heart rate variability (HRV), a mode to assess the state of the parasympathetic nervous system ( Brown & Gerbarg 2005, Cysarz & Buessing 2005, Jovanov 2005, Lee et al. 2005, Khattab et al. 2007, Raghuraj & Telles 2008, Li et al. 2009, Schmidt & Carlson 2009, Asher et al. 2010, Patra & Telles 2010, Tang et al. 2009, Matsubara et al. 2011, Nugent et al. 2011). • Gender differences can play a role in all three subsystems and specific female characteristics need to be considered, for example: A structured standardized questionnaire and examination such as Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD of the Department of Oral Medicine, Orofacial Pain Research Group, University of Washington, Seattle USA, Dworkin & LeResche 1992, List & Dworkin 1996, Dworkin et al. 2002) may be advocated for a number of reasons in multidisciplinary clinical or scientific settings. However, the RDC/TMD questionnaire has recognized limitations in the diagnosis of some articular conditions ( Look et al. 2010) and the Maitland model of a semi-structured dialogue is preferred as it enables the clinical physiotherapist to gain in-depth information, to develop various hypotheses simultaneously, and to recognize mixed conditions using sound clinical reasoning. Four types of complaints can be considered as leading symptoms for TMD: • Pain just in front of, at or in the ear on mandible (mouth) movements • Sounds just in front of, at or in the ear on mandible (mouth) movements • A blocked mouth opening or closing, all indicating an intra- or periarticular dysfunction • Pain in the masseter and temporal region at mouth opening, chewing or in the early morning, indicating an extra-articular problem A patient with a TMD most commonly has symptoms associated with mandibular movements, such as wider mouth opening, indicating that the source of the TMJ is structural (intra-/peri-articular or extra-articular). Apart from pain, the main symptom of TMD can be a block, or a clicking sound. • Figure 3.5 shows the commonest pain areas described by patients with an intra- or periarticular TMJ disorder ( Campbell et al. 1982). Figure 3.5 Typical primary area of symptoms in intra- and periarticular temporomandibular joint disorders. • Figure 3.6 shows common pain sites in patients with extra-articular dysfunctions (Svensson et al. 2003). Figure 3.6 Typical myogenic or other areas of pain and symptoms in extra-articular temporomandibular joint dysfunctions. • Symptoms can include local pain over chewing or hyoidal muscles, radiating pain from trigger points of chewing, hyoidal or cervical muscles, for example, radiating to the teeth, mandible pain after a fracture, etc. • Pain in the jaw can be related to periodontal dysfunctions, tooth decay or infection (odontogenic pain), which may also cause referral of pain locally from the teeth along the jaw. • Aching in the cheeks and jowls could be due to a disorder of the parotid glands. This will be accompanied by changes in function of the salivary glands such as overproduction or dryness of the mouth, even during eating. • Ongoing neck pain that is not responding to adequate neuromusculoskeletal treatment may be due to parafunctional habits or occlusal faults and needs dental screening (Clark et al. 1987, 1993, Browne et al. 1998). • TMD may be accompanied by tinnitus or may mimic otological disorders such as middle ear infections, which, however, are accompanied by alteration in auditory function and vestibular function (vertigo). • The craniofacial area can host many different, bizarre, often called ‘associated symptoms’ that may have a viscero- or neuro-cranium background and may be related to upper cervical and cranial nerves, meninges, cranial bones and osseous connections, parasinuses, auricular or other structures or even neoplasms ( Ciancaglini et al. 1994, International Headache Society 2003, Parker & Chole 1995, Steigerwald et al. 1996, Tuerp 1998, Wright et al. 2000, Lam et al. 2001, Peroz 2001, 2003, Tuz et al. 2003, Sobhy et al. 2004, Wright 2007, Biesinger et al. 2008, 2010, Boesel et al. 2008, Losert-Bruggner 2000). • Such symptoms can be pins and needles affecting the head, face or tongue, spasm or trismus of the masticatory muscles, tinnitus, dizziness, vestibular disturbance, tearing, difficulties at swallowing, feeling of a lump in the throat, dystonia, dysfunctions of classic senses (olfaction, audition, vision, gustation, tactition), nausea, as well as loss of concentration, memory loss, panic attacks and various types of headaches, such as tension type, migraine with or without aura and neuralgic pains ( IHS 2003). All these symptoms require specific neurological screening of the central nervous system, the upper cervical and cranial nerves, as well as radiological and/or ear, nose and throat (ENT) screening. • True trigeminal neuralgia is characterized by severe episodes (attacks) of, often unexpected, burning neuralgic pain, for example, due to arterial compression of the trigeminal nerve (CN5) when leaving the pons or after a herpes zoster virus infection, and is a primary indication for pharmacological or surgical management. • The mandibular condyle is a relatively common site of (often) benign tumours. Obvious accompanying signs will be a swollen mass and other signs of impending or actual inflammation. Pain will be relatively constant and unchanging with rest. • Symptoms such as pain along the zygomatic arch or the frontal bone accompanied by pressure changes and respiratory dysfunction may well be of sinus origin. • Synovial joints also occur between the thyroid cartilage and the sides of the cricoid cartilage, the laminae of the cricoid cartilage and the base of the arytenoid cartilage and occasionally between the lesser and greater cornua in the hyoid bone ( Banks & Hengeveld 2005). It is not common for these joints to be painful but as they possess synovial joint material and are supported by ligaments, they occasionally give rise to local symptoms. • Typical provoking and/or limited activities in TMD are wider mouth opening when eating, biting, chewing, yawning, singing, kissing, swallowing and prolonged playing of instruments such as the violin, flute or other wind (brass) instruments ( Yap et al. 2001). • Parafunctional habits, for example, teeth grinding or clenching (bruxism), inducing muscle pain normally bothers most sufferers in the early morning after sleep or at times of increased distress, whereas occlusal faults may cause muscle pain at (sub)maximal use of the chewing muscle, for example, in biting ( Svensson et al. 2008). It is estimated that up to 80% of all TMD patients may suffer this type of myogenic pain ( Graber 1989, Bendtsen et al. 1996), which are would primarily be managed by dentists or orthodontist ( Ommerborn et al. 2011). • Biting on the tongue may be a stress-induced coordination problem. • Psychosocial factors should be ruled out by screening (yellow flags). • While muscle pain is common, muscle lesions are rare. • Chewing and supra- or infrahyoidal muscles may include trigger points with typical patterns of radiation, for example, teeth pain from a medial pterygoid trigger point at biting (Svensson et al. 2003ab, Bertilsson & Strom 1995). • Tension-type headaches and muscular neck pain may be accompanied by temporal, masseter or pterygoidal muscle pain. • Only one in eight patients may show a true, isolated arthropathy, with or without clicking; however, they need more often and longer physiotherapeutic treatments than patients with myogenous problems. • The remaining 8% of all TMD patients seem to have oro-craniofacial symptoms from other sources such as the cervical spine or the cranial nerves ( Graber 1989). • Therapists in practices might not see many patients with severe or irritable pain, who are unable to move the mandible and cannot use the mouth at all. • The source of intra-articular pain is likely to be in the bilaminar zone, as the retrodiscal area has a large inflammatory capacity. These patients are likely to be managed by the dentist with anti-inflammatory drugs, local cooling and a splint. • Clicking sounds are most often a sign of instability of the disc–condyle complex on excursive and or incursive movements. • The disc may be anteriorly, anteromedially or anterolaterally displaced in static occlusion or is displaced during excursive movements. The most classic one, accompanied with a louder click on opening is due to repositioning of the disc on the condyle, whereas the anterior displacement click, terminally at elevation, may not be heard or felt. The clicking on opening may appear initially, intermediate or terminal during opening, representing a further development of the pathology, eventually leading to a non-repositioning situation with the anterior displaced disc limiting full mouth opening ( Figs 3.7 and 3.8). Figure 3.7 Temporomandibular joint internal derangement, reciprocal click. (From Kraus 1985. Reproduced with kind permission.) Figure 3.8 Temporomandibular joint internal derangement-closed lock. (From Kraus 1985. Reproduced with kind permission.) • Eminentia clicking is due to poor control at terminal depression or initial elevation and may develop into a block if, when yawning, the patient is unable to close the mouth again. • A repositioning might need to be performed under general anaesthetic. • A lateral ligament clicking or snapping through range of mandibular motion can be palpated superficially with a finger tip on the lateral pole of the condyle. • This is normally not painful and may be due to a lateral malposition of the condyle, causing an increased tension in the lateral capsule and ligament. • Crepitations are normally signs of degenerative processes, roughing of temporal fossa or articular disc surfaces, maybe accompanied by morning stiffness of the jaw, however are seldom painful. • Occasional, almost silent, popping sounds may be caused by sustained compression-induced fibrous adhesions between the fossa and disc. • A fracture of thin osseous border with the meatus acusticus externa may cause an over-/underpressure-induced movement of the remaining capsule at every mandibular movement and so a loud audible snapping noise ( Muhl et al. 1987, Westesson & Eriksson 1985, Osborn 1995b, Capurso 1997, Widmalm et al. 1996, 2003ab, Prinz 1998abc, Bumann & Lotzmann 2000, Leader et al. 2003). • These ‘in range-of-motion’ clicking conditions are contraindications for intra-articular directed manual therapy techniques, whereas longitudinal caudad directed techniques to mobilize the capsular structures may be beneficial to deload the intra-articular structures as well. • End-range intra-articular conditions, such as fibrosis after trauma or surgery, are far less common in daily practice; however, they might profit from transverse medially directed accessory movements at the limit of the problematic excursive movement(s). • Active training of the rotatory movement component in the lower joint compartment, however, is generally indicated to support the effect of passive movements (see Fig. 3.55). • An extra-articular, muscular dysfunction commonly represents an end-range problem, even to such an extent that it prevents an end-range joint examination, which needs immediate management, if possible ( Table 3.1). Table 3.1 Examples of TMD categorized according the localization of symptoms in relation to the temporomandibular joint and the degree of the dysfunction • The laryngeal or hyoid joints and muscles may cause local symptoms such as a feeling of a lump in the throat or a sore throat on swallowing, talking or coughing, which requires medical as well as cervical and psychosocial screening ( Pancherz et al. 1986, Winnberg 1987, Winnberg et al. 1988). • Acute pain problems are likely to be managed by dental medical disciplines. • Traumatic onsets may have injured, or even fractured, the mandible, the condyle, the bilaminar zone of the TMJ or other skull and neck structures as in motor vehicle accidents, falls with direct impact on the mandible when skiing, biking, being hit at boxing and martial arts or by a hockey stick, being kicked by a horse, or being hit by an elbow, a head or a shoe at soccer ( Weinberg & Lapointe 1987, McKay & Christensen 1998, O’Shaughnessy 1994, Garcia & Arrington 1996, Abd-Ul-Salam et al. 2002). • Even a tooth extraction might become a trauma for the TMJ, with a subsequent inflammation of the bilaminar zone or capsulitis. • A severe retrodiscal inflammation may cause an anterior disc displacement. • Arthroscopy may have been performed to remove a displaced disc. This procedure is not performed routinely, as the disc may resolve in the anterior capsule without causing many problems. • Surgery, in contrast, may be necessary after trauma (fracture) or in the case of neoplasms. • Previous surgery or arthroscopy of the TMJ may demand extensive rehabilitation for mandibular movements and resting position as well as for the cervical spine. • The onset of the problem might reveal a specific use category. • Some examples are biting a hard nut, a big apple, a king-size burger, intensive training with (new) musical instruments (jaw muscles, larynx or hyoid region pain), or a period with prolonged and increased distress prior to examinations. • Further common causes are long dental treatment, characterized by maximum mouth opening, an occlusal problem, for example, after dental treatment (new filling), orthodontic management with braces, or other excessive, aberrant use of the mandible. • Even learning a new language might cause transient functional complaints. • Professional singing may lead to complaints at maximum mouth opening, for example, an inability to close the mouth (closing block) when the head of the mandible cannot overcome the tubercle at the beginning of the incursive movement in hypermobile women. • Recognition of the appropriate use category will lead to adequate management and a change in practice. • Recognized distress factors may be the cause of myogenic complaints or even the onset, rather than the cause, of intra-articular complaints. • Bruxism-induced muscle pain may account for 30% of all complaints ( Graber 1989). The pain is originally felt at the temporal and/or masseter area; however, it may spread to the anterior and posterior neck area in later stages. • Local symptomatic treatment is normally insufficient and long-term success is related to recognition and managing the causal stress factors. • The main reason for spontaneous pain in the jaw region is odontogenic and dental treatment will normally be successful. Hidden tooth infections, possible causing diffuse general complaints, challenge clinicians and scientists, and may only be discovered after a long period of suffering. • Answers to further targetted questions may reveal a hidden cause of the problem. • Analysis of previous trauma, events, psychoemotional and socioeconomic factors as well as further investigations may reveal a range of predisposing factors: • Occlusal faults may explain spontaneous symptoms of myogenic origin that are estimated to account for 50% of all complaints ( Graber 1989). • Dysfunctions of the anterior upper cervical spine offer another regular explanation for facial pain. • Postural faults, such as an exaggerated thoracic kyphosis with flexion of the lower cervical spine, lead to a compensation in the upper cervical spine into extension (poking chin), a posterior change of the upper postural resting position of the mandible and habitual occlusion (bite) ( Fink et al. 2003, Klemm 2009, Mansilla-Ferragut et al. 2009, Matheus et al. 2009, Munhoz & Marques 2009, Saito et al. 2009, Schupp et al. 2009, Toti et al. 2010). • A posterior shift of the mandibular condyle challenges the physiological centric relation and may induce intra-articular compensation and hyperactivity of the chewing muscles. • In the absence of any predisposing factor, diseases such as benign neoplasms, gland and lymphatic disorders should be taken into consideration, as well as mandibular and tooth growth anomalies in children ( Egermark et al. 2003, Tecco et al. 2010, Thilander et al. 2002). • Establishing the patient’s history will help towards the diagnosis and the assessment of the stability of the disorder. • The fibrous type of cartilage of the mandibular head allows a long slow development of degeneration without complaints. After the onset of arthrogenic problems, however, imaging procedures will show a progressed stage of the pathology and recovery might take a long time or fail. • Many patients with a long history report different types of management that have not been completely successful. • Ongoing complaints affecting the facial area may have a large impact on daily life and psychoemotional state. • Persisting impairments and related sensitization of the central nervous system with secondary hyperalgesia and allodynia may lead to the condition becoming chronic, with spreading or bizarre pain patterns and descriptions, accompanied by other psychosomatic symptoms that may overshadow the somatic and still relevant dysfunctions. • A psychosomatic origin (parafunctional habits causing myogenic pain) as well as psychoemotional consequences of ongoing complaints justify psychosomatic management approaches such as pain management strategies (coping, pacing, graded exposure), cognitive–behavioural therapy, bio- or myofeedback or mind-body therapies, for example, craniosacral therapy, as part of the overall management. • Cranium techniques can be applied in different ways depending on the present state of the patient and the actual aim of the therapy ( Ridley 2006). • With structure-directed treatment, cranium techniques may be applied end range, whereas emotional states might profit from very gentle, slow rhythm handling, inducing balancing effects on the autonomous nervous system, measurable with heart-rate variability (HRV) and the emotional motor system, for example, measurable with EMG of the chewing muscles (see the section on Management). • The patient’s answers to routine questions about their general health, other medical problems, use of medication and unexplained weight loss may suggest non-neuromusculo-skeletal disorders, serious pathology or relevant comorbid factors that require further examination a change in management or caution. • Women might suffer more frequent and stronger pain due to oestrogen and may need to be referred to a gynaecologist. Specific medication or a change of the type of contraceptive pill might be indicated. • Imaging procedures are considered important ancillary tools for precise diagnosis. An (ortho)pantomogram is an X-ray procedure performed by the dentist or orthodontist, mainly for dental diagnostics, however, it also shows both TMJ and the atlas-axis relation. • In the case of suspected intra-articular temporomandibular disorder, functional magnetic resonance imaging (MRI) in a closed mouth and open mouth position is a mandatory examination. Further mandibular positions might be examined, for example, while the patient is wearing the splint. • Functional MRI reveals the physiological or pathological position of the disc, an instability of the articular disc, the precise direction of displacement, repositioning of the disc, or lack of, the degree of compensatory or degenerative changes of the head of the mandible, additional inflammatory signs, and also muscular or other anomalies ( Schmid et al. 1992, Pressman et al. 1992, Schimmerl et al. 1993, de Laat et al. 1993, Langendoen-Sertel & Volle 1997, Mueller-Leisse et al. 1997, Yang et al. 2002, Guler et al. 2003, Rocha Crusoé-Rebello et al. 2003, Kitai et al. 2004, Pedulla et al. 2009). • Re-examination after a six-month continuous distraction splint therapy usually shows a stable distraction, indicating the newly formed connective tissue in the distraction-induced joint space. • Special attention should be given to splints that patients may or should wear on the upper or lower dental arch ( Bumann & Lotzmann 2000, Tuerp et al. 2004, Al-Ani et al. 2005). • The main types of splints are: 1. Relaxation type of splint (‘Michigan’) or other devices with the same aim, such as an anterior bite stop or a nociceptive trigeminal inhibition tension suppression system (NTI-tss) ( Stohler & Ash 1986, Canay et al. 1998, Becker et al. 1999, Baad-Hansen et al. 2007, Macedo et al. 2007, Kares 2008). The splint is worn during sleep with the aim of reducing grinding, thus protecting teeth against abrasia by optimizing occlusion as well as frontal and canine teeth guidance. Patients report that jaw muscle pain, as well as (tension type) headaches and neck pain are positively influenced. In extreme cases (bruxomania), this type of splint may be worn during the day as well. 2. Repositioning splint. Only indicated in acute disc displacements with an intact morphology of the disc and the retrodiscal ligaments. To be worn to induce a stable repositioning of the disc and in combination with anti-inflammatory drugs. 3. Distraction (or decompression) splint. Indicated in intra-articular disorders, however mainly used in disc displacements with pain, to continuously distract the head of the mandible (six months, 24 hours a day), enabling the formation of hard connective tissue in the joint space that serves as a substitute disc ( Hugger et al. 2004). 4. Centric relation splint. This aims to optimize the centric relation, reducing bilaminar and periarticular loading ( Tuerp et al. 2004). This type can be used in articular conditions when a distraction splint is rejected by a patient. • Splints normally have a built-in frontal and canine teeth guidance to optimize the quality of the mandibular movement and prevent adverse tissue loading ( Fitins & Sheikholeslam 1993). • Special questions and specific examination procedures for upper cervical risk factors are described in Chapter 4 of Maitland’s Vertebral Manipulation ( Blake & Beames 2013). • If the patient has not been referred by a dentist, a consultation is recommended for occlusal screening and, if necessary, management ( Egermark et al. 2003, Suvinen & Kemppainen 2007, Tecco et al. 2010). For examination of cervical and thoracic structures, see Maitland et al. 2005 and Chapter 4 of this volume for examination of shoulder girdle structures. Examination of the upper cervical spine should always be included in an initial craniomandibular examination ( Box 3.1). • Swelling/hypertrophy, for example, convexity of masseter area ( Fig. 3.9) Figure 3.9 Convexity of cheek: A indicating masseter hypertrophy due to parafunctional habit (bruxism) or B occlusal fault. (Reproduced with the permission of the Interdisciplinary Forum for Cranio-Facial Syndromes (IFCFS).) • Any obvious skull or mandibular developmental abnormalities, for example, open mouth/lips and/or discluded/occluded resting position of the mandible (also, ask the patient about the resting position of the tongue). • Note nasal or mouth breathing. • Horizontal alignment of the eyes, zygomatic arches, auricular tragus or ear lobe and mouth. • Symmetry in vertical dimension of the lateral canthus of the eye – corner of the mouth. • Overbite or loss of vertical dimensions can be assessed by comparing the distances between the lateral canthus of the eye and the corner of the mouth. • With the anterior nasal spine and the point of the chin ( Trott 1986, Kraus 1994). These two distances are normally equal but overbite is present if the second measurement is more than one centimetre less than the first. • Anterior neck with hyoid bone and larynx cartilages (including the cricothyroid joint). • If pain around the TMJ is reproduced during eating with upper cervical extension and mandibular depression ( Fig. 3.11): Figure 3.11 Differentiating between the upper cervical spine (extension) and TMJ (depression) of pain in an eating position. • If pain is felt at waking up prone with the head rotated ( Fig. 3.12), does the contraction of the chewing muscles produce pain in the temporal or masseteric area? Is palpation of muscular sites painful? Figure 3.12 Differentiating between upper cervical spine (rotation) and TMJ (depression, lateral movement) in prone lying with rotated head. • If throat pain is reproduced during extension of the head, stabilize the head at the point of onset of the symptoms and ask the patient to swallow or move the position of the tongue to differentiate between the laryngeal and hyoid joints and the anterior cervical intervertebral structures. • Check for the correct position of the tongue at the hard palate when swallowing. • Observe the habitual occlusion. • Opening the mouth as widely as possible while monitoring cervical movement. • Clenching the teeth tightly. • Move the mandible maximally to the left and right ( Fig. 3.13). Figure 3.13 Brief appraisal of lateral movement to the left and right in sitting. Lateral movement to the right shows a malocclusion-related compensatory cervical tilt. (Reproduced with the permission of the IFCFS.) • In supine lying, with bilateral condylar palpation and sight of the incisal and canine teeth. • The therapist sits beyond the patient’s head facing the patient’s feet. • The patient has to open his lips actively at all times during testing. • Assess pain, quantity and quality such as clicking sounds, incisal and canine guidance, deflective occlusal contact, note and differentiate deviations or deflections. • Apply overpressure if appropriate, with stabilization of the cervical spine. • Note the effects of head on neck, neck on neck and neck on trunk position on ranges of TMJ movement, pain response and clicking ( Lee et al. 1995, de Wijer et al. 1996abc, Palazzi et al. 1996, Higbie et al. 1999, Ioi et al. 2008). • The examination movements may be applicable as treatment techniques in selected cases. Figure 3.14 Active mouth opening with bilateral condylar palpation and observation of the mandibular course of the movement. • Pain: where and when (in mm)? Related to clicking? No pain: apply overpressure by applying a ‘money-counting’ kind of movement with the thumb and index finger. The tip of the thumb should push the upper incisal teeth upwards and the tip of the index finger should push the lower incisal teeth caudally. The other hand is placed behind the occiput and cervical spine with the anterior side of the shoulder on the frontal bone to stabilize the head and the neck. • Range: measure in mm including vertical overbite (normally 4 mm), normally 40–55 mm or the width of three fingers (index, middle and ring finger) at the proximal interphalangeal joints (PIP). • Is there limitation in range with pain in a chewing muscular area? Treat immediately with local massage, hold-relax techniques, electro-massage or taping to relax the tensed muscle ( Figs 3.16 and 3.17). Figure 3.16 Hold-relax technique, biting, with transverse application of spatulas to relax masticatory muscles and gain range of motion.
Management of craniomandibular disorders
Introduction
Theory – functional anatomy
Causes and contributing factors for craniomandibular dysfunction
 protrusion or protraction (forward shifting of the chin)
protrusion or protraction (forward shifting of the chin)
 retrusion or retraction (shifting the chin posteriorly)
retrusion or retraction (shifting the chin posteriorly)
 laterotrusion or lateropulsion (lateral movements to the left and right).
laterotrusion or lateropulsion (lateral movements to the left and right).
 a small anteroposterior diameter of the mandibular head (Müller et al. 1992ab)
a small anteroposterior diameter of the mandibular head (Müller et al. 1992ab)
 a deep steep fossa, indicating an increased resistance for excursive movements and muscle activity in the lateral pterygoid muscle ( Osborn 1995a)
a deep steep fossa, indicating an increased resistance for excursive movements and muscle activity in the lateral pterygoid muscle ( Osborn 1995a)


 licking, chewing and swallowing
licking, chewing and swallowing
 and, with an additional hormonal component, lordosis behaviour or receptive posture in females. The latter implies changing tone and activity of abdominal, back, psoas major, adductors and hamstrings during the menstrual cycle.
and, with an additional hormonal component, lordosis behaviour or receptive posture in females. The latter implies changing tone and activity of abdominal, back, psoas major, adductors and hamstrings during the menstrual cycle.
 passive subsystem: hypermobility, a small mandibular condyle (Müller et al. 1992ab)
passive subsystem: hypermobility, a small mandibular condyle (Müller et al. 1992ab)
 active subsystem: less muscle endurance power ( van Eijden et al. 1995, English & Widmer 2003)
active subsystem: less muscle endurance power ( van Eijden et al. 1995, English & Widmer 2003)
 control subsystem: different stress coping strategies, hormonal aspects that increase pain sensitivity ( LeResche et al. 1997, Cairns et al. 2003) and muscle tension.
control subsystem: different stress coping strategies, hormonal aspects that increase pain sensitivity ( LeResche et al. 1997, Cairns et al. 2003) and muscle tension.
Subjective examination
Kind of disorder
Areas of symptoms (body chart)
Behaviour of symptoms (over a 24-hour period)
History of symptoms (present and past)
Trauma
Events
Spontaneous onset
 an old condylar fracture or juvenile rheumatoid arthritis might have led to a degenerative joint disease
an old condylar fracture or juvenile rheumatoid arthritis might have led to a degenerative joint disease
 a range of congenital abnormalities, maldevelopments of mesodermal structures such as a cleft palate, a suboptimal or absent dental or orthodontic management during the growth years to asymmetrical joints
a range of congenital abnormalities, maldevelopments of mesodermal structures such as a cleft palate, a suboptimal or absent dental or orthodontic management during the growth years to asymmetrical joints
 a too small anteroposterior diameter of the condyle to disc-condyle instability
a too small anteroposterior diameter of the condyle to disc-condyle instability
 a loss of molars to increased joint compression, mainly in elderly people.
a loss of molars to increased joint compression, mainly in elderly people.
Gradual onset
Contributing factors
Medical screening questions
Physical examination
Observation
In sitting

En face
Functional demonstration

 stabilize the head at the onset of pain and increase or decrease the mandibular depression
stabilize the head at the onset of pain and increase or decrease the mandibular depression
 stabilize the mandible at the onset of pain and decrease and increase upper cervical extension.
stabilize the mandible at the onset of pain and decrease and increase upper cervical extension.

 stabilize the head at the ‘bite’ of pain and increase or decrease the lateral deviation of the mandible in the appropriate direction
stabilize the head at the ‘bite’ of pain and increase or decrease the lateral deviation of the mandible in the appropriate direction
 stabilize the mandible in depression/lateral position and increase or decrease the cervical spine
stabilize the mandible in depression/lateral position and increase or decrease the cervical spine
 apply temporomandibular and upper cervical accessory movements (for example,unilateral posteroanterior) in the rotated position for further confirmation.
apply temporomandibular and upper cervical accessory movements (for example,unilateral posteroanterior) in the rotated position for further confirmation.
Brief appraisal
In sitting


Active movements
Mouth opening (depression) ( Figs. 3.14 and 3.15)


![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree