Management of Vascular Injuries Following Soft Tissue and Bony Trauma
Gustavo S. Oderich
Timothy M. Sullivan
Accidental injuries affect 2.6 million people in the United States each year. Mechanisms of injury include penetrating, blunt, and iatrogenic trauma. It is estimated that vascular trauma affects 0.2% to 4% of all injured patients. Therefore, approximately 20 to 100,000 patients will sustain a vascular injury. Over 80% of these vascular injuries will be located in extremities. Ninety percent of all vascular injuries are associated with penetrating trauma, of which 70% are due to gunshot injuries, 20% are due to stab wounds, and 10% are due to blunt trauma. Combined vascular and orthopaedic trauma is relatively uncommon, accounting for less than 1% of all cases of traumatic injuries. Vascular injuries can occur because of the superficial location of vessels, their proximity to bones, and their relatively fixed position across joints. Patients sustaining combined injuries are exposed to substantially increased risk of amputation and limb dysfunction. This chapter focuses on the indications, contraindications, preoperative planning, operative approach, and results of repair of the most common combined vascular and orthopaedic injuries.
Indications/Contraindications
Primary repair of arterial and venous injuries is indicated to control bleeding and/or to relieve limb or organ ischemia. Life-threatening injuries should be recognized early during the resuscitation phase and prioritized before proceeding with vascular and orthopaedic repair. Arterial injuries affecting only one of the tibioperoneal or forearm arteries may be treated conservatively provided that there is no evidence of distal ischemia. Nonocclusive arterial injuries (e.g., small intimal flaps or dissections) incidentally found on imaging studies can be safely observed. The benign natural history of these injuries is well documented in several large series; operative repair is required in less than 1% of patients.
Extremity trauma with complex soft tissue, vascular, and skeletal injuries poses one of the most difficult management problems. Patients should be evaluated by a multidisciplinary team. Coordinated interaction of various specialists including a vascular, orthopaedic, and plastic surgeon is of paramount importance to optimize outcome. Injuries of the head, chest, and abdomen may require additional neurosurgical and general trauma consultation. Every effort is made to balance the potential success of an arterial reconstruction and correction of the orthopaedic injury with the overall clinical status of the patient and the potential for complete functional recovery. In general, once life-threatening injuries are stabilized, treatment priorities are as follows:
Control of bleeding and restoration of arterial inflow.
Fracture reduction and stabilization.
Soft tissue coverage.
Vascular repair should be prioritized over definitive orthopaedic repair. Any delay in vascular reconstruction is a gamble and may risk the only opportunity for limb salvage. Patients with stable fractures or dislocations in which minimal manipulation and length discrepancy is anticipated should be treated with immediate definitive arterial revascularization. However, patients with severely comminuted fractures and dislocations, segmental bone loss causing limb discrepancy, or severe soft tissue disruption and contamination should be treated initially with temporary intra-arterial shunts. In these cases, it is wise to delay the definitive vascular reconstruction until wide debridement and initial skeletal repair are accomplished.
Contra-indications for vascular repair include presence of other life-threatening injuries requiring immediate attention or causing hemodynamic instability. Several predictive factors should be taken into consideration when deciding to perform revascularization versus primary amputation (Table 6-1). Overall, approximately 10% to 20% of patients with complex extremity injuries have nonsalvageable limbs and require primary amputation. Assessment of these patients should be individualized. Several factors should be taken into consideration, including the overall clinical status, severity of the arterial, neurologic, and orthopaedic trauma, and expected functional recovery. A primary amputation is considered in cases of dysvascular extremity with complex fractures and extensive soft tissue and nerve damage. Patients with major nerve transections (e.g., tibial nerve transection) and open comminuted tibiofibular fractures with arterial injuries (Gustilo III-C) have very poor functional outcome and high amputation rates; these patients are generally treated with primary amputation. Major nerve transections should be confirmed by direct visualization. Other indication for amputation is prolonged ischemia time (>12 hours) with evidence of a cadaveric extremity (e.g., mottled with absence of motor function, arterial, or venous Doppler signals).
Preoperative Planning
Prolonged ischemia time is the most important factor associated with limb dysfunction or amputation. A high index of suspicion coupled with accurate neurovascular examination is necessary for prompt diagnosis of a vascular injury. Accurate diagnosis of vascular injuries is an essential aspect in the preoperative evaluation of patients with complex extremity trauma. Prompt restoration of arterial blood flow within 6 hours from the time of initial extremity injury is the most critical factor that determines limb salvage and function.
Complete history including the mechanism of trauma, associated injuries, medical history, medications, and allergies should be recorded. Extremity vascular trauma is immediately apparent because of external bleeding, hematoma, or obvious limb ischemia. Physical examination includes inspection of the injured limb for open wounds, obvious deformities, and signs of ischemia. Distal ischemia is manifested by the five Ps: pallor, paresthesia, paralysis, pain, pulselessness, and poikilothermia. A thorough sensory and motor examination and pulse examination should be noted. The presence of hematoma, pulsatile or not, bruit, and thrill must be documented. If distal pulses are diminished or absent, the ankle-brachial index should be determined using a hand-held Doppler device.
Signs of arterial injury have been traditionally classified into “hard” and “soft” signs (Table 6-2). These correlate with the presence of a hemodynamically significant arterial lesion. “Hard” signs include
absence of distal pulses, pulsatile bleeding, expanding hematoma, palpable thrill, and audible bruit. “Soft” signs include proximity to the vessel, peripheral nerve deficit, history of moderate hemorrhage, and diminished distal pulses.
absence of distal pulses, pulsatile bleeding, expanding hematoma, palpable thrill, and audible bruit. “Soft” signs include proximity to the vessel, peripheral nerve deficit, history of moderate hemorrhage, and diminished distal pulses.
Table 6-1. Factors Associated with Poor Functional Recovery or Need for Primary Amputation After Combined Vascular and Orthopaedic Extremity Trauma | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 6-2. Clinical Signs of Vascular Injury | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
The general recommendation is that patients with hard signs associated with uncomplicated penetrating trauma should undergo immediate operative exploration, without need for arteriography or duplex ultrasound. The indications for arteriography are summarized in Table 6-3. Patients with multiple penetrating injuries should be evaluated with arteriography to determine the exact location and extent of arterial lesions. Arteriography is also advised in patients with combined arterial and orthopaedic trauma, even in the presence of hard signs. While the presence of hard signs predicts major vascular injury in nearly 100% of patients with uncomplicated penetrating trauma, less than 15% of patients with complex blunt injuries will require vascular repair. The inaccuracy of hard signs in this subgroup is explained by a combination of multiple other factors that ultimately lead to diminished pulses, including fractures, soft tissue disruption, compartment syndrome, and extrinsic arterial compression. Therefore, we generally recommend arteriography in all patients with complex skeletal trauma and hard signs of vascular injury.
We generally prefer a one-shot intraoperative arteriography technique. This avoids the 1 to 3 hour time delay required to obtain a formal arteriography in the angiography suite. An antegrade or retrograde approach in the affected limb is used for most cases. The availability of a portable C-arm and fluoroscopy permits localization of bony landmarks, selective catheterization of arterial branches, and endovascular treatment of arterial lesions. However, because fluoroscopy is usually not readily available in the emergency setting, we usually use ultrasound guidance and a micro-puncture set for arterial access. The target artery (e.g., common femoral artery or brachial artery) is accessed with a micropuncture needle (18 gauge) in an antegrade or retrograde fashion. A 0.018 inch guidewire is advanced to allow placement of a sheath. The sheath can be used for contrast injection. Alternatively, the 0.018 inch wire is exchanged into a 0.035 inch wire and a 4 French sheath is advanced. The arterial inflow proximal to the access site should be manually compressed during contrast injection using digital pressure or a tourniquet. A single hand injection of 30 mL of diluted (50:50) iso-osmolar contrast allows adequate visualization of the area of concern and distal runoff vessels.
Other noninvasive imaging modalities are duplex ultrasound, computed tomography angiography (CTA), and magnetic resonance angiography (MRA). Computed tomography angiography is now available in most centers, is quite expeditious, and permits excellent image of the arterial circulation, soft tissue, and bone. This is particularly useful for planning operative approach in patients with centrally located lesions (e.g, aorta, subclavian, or iliac arteries). However, limitations are the relatively large contrast load (150 mL) in a patient who may potentially require additional angiography.
We recommend duplex arterial ultrasound in patients with “soft” signs of vascular injury, including those with an ankle-brachial index of less than 0.90. Arterial imaging is not required in patients
with normal pulses and no other sign of arterial injury. Physical examination excludes significant arterial injuries as reliably as arteriography or surgical exploration. This is also true for patients with posterior knee dislocations, in whom arteriography used to be obtained routinely in the 1980s. Results of contemporary series show that in the absence of hard signs, less than 5% of patients had abnormalities on the arteriography but none required operative treatment or had amputation. On the other hand, the incidence of significant vascular injuries is 70% in the presence of hard signs. In patients with normal pulse examination, nonocclusive lesions include small intimal flaps, dissections, contusions, or small pseudoaneurysms; these lesions should be treated with antiplatelet therapy only.
with normal pulses and no other sign of arterial injury. Physical examination excludes significant arterial injuries as reliably as arteriography or surgical exploration. This is also true for patients with posterior knee dislocations, in whom arteriography used to be obtained routinely in the 1980s. Results of contemporary series show that in the absence of hard signs, less than 5% of patients had abnormalities on the arteriography but none required operative treatment or had amputation. On the other hand, the incidence of significant vascular injuries is 70% in the presence of hard signs. In patients with normal pulse examination, nonocclusive lesions include small intimal flaps, dissections, contusions, or small pseudoaneurysms; these lesions should be treated with antiplatelet therapy only.
Table 6-3. Indications for Preoperative or Intraoperative Diagnostic Arteriography in Patients with Combined Extremity Trauma | ||
|---|---|---|
|
Surgery
Patient Positioning and General Approach
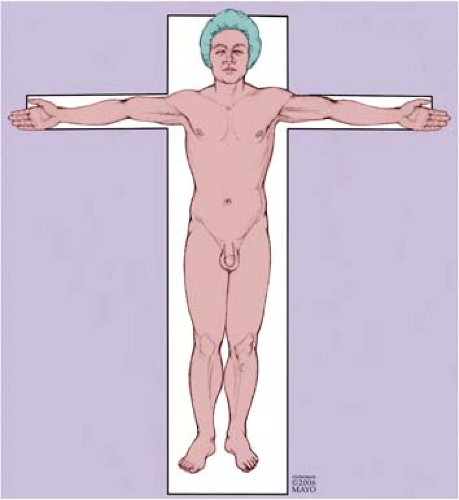
All vascular injuries can be accessed using the supine anatomic position (Fig. 6-1). Although prone position and a posterior approach may be used for isolated popliteal artery injuries which do not extend into the superficial femoral or tibioperoneal arteries, this approach limits access to the great saphenous vein if harvesting is necessary and may require excessive manipulation of the fractured limb. A generous sterile field should be prepared and draped to allow adequate exposure, proximal and distal control, and options of extra-anatomic reconstruction if indicated. The wise surgeon should always consider the “worst case scenario” (e.g., axillofemoral graft). A noninjured lower extremity should be prepped circumferentially for possible vein harvesting. The ideal conduit is an autologous great or small saphenous vein. Preoperative intravenous antibiotics (e.g., a first-generation cephalosporin) should be administered.
Technique
Repair of vascular injuries can be one of the most challenging aspects of trauma management. Some basic principles of vascular repair are applicable to all vascular injuries (Table 6-4). The operative sequence consists of access, exposure, control, and repair. Initial control of external hemorrhage is usually obtained with simple digital or manual pressure. Use of surgical instruments such as hemostats is not only ineffective but risks iatrogenic injury of adjacent nerves or veins. Manual compression is maintained by a member of the surgical team until definitive proximal and distal control of the injured vessel is obtained. The hematoma should not be entered without first obtaining proximal
and distal control away from the site of injury. Access is gained using the standard exposure techniques described in the following discussion. Vascular clamps should not be applied forcefully and blindly; instead, the artery should be completely dissected, looped with a silastic vessel loop, and clamped under direct vision. One important adjunct is the use of balloon occlusion catheters. This facilitates control in areas of difficult access and avoids excessive dissection. In addition, pressure cuff tourniquets may be used in the extremities to achieve prompt vascular control. Once control is gained, the hematoma is explored with careful attention to avoid injury to adjacent structures. The extent of vascular injury is assessed and clamps are moved closer to the vascular wound. The injured vessel should be debrided and cleaned using tenotomy scissors. The extent of debridement should take into consideration the mechanism of injury, with more extensive debridements for high-velocity gunshot wounds, and blast or crush injuries. One should avoid excising the adventitia of the vessel while dissecting or debriding the artery. Distal and proximal thrombectomy using a Fogarty balloon thromboembolectomy catheter should be performed even in the presence of relatively good prograde or retrograde bleeding. The size of the catheter is generally a 4 or 5 for the iliacs, 4 for the superficial femoral, 3 or 4 for the deep femoral, 2 or 3 for the tibials, and 2 for the pedal and smaller arteries of the forearm. Passage of thromboembolectomy catheters into the deep femoral, tibials, and smaller arteries should be done gently because of risk of arterial rupture, dissection, or intimal injury due to excessive balloon inflation. At least two “clean” passes should be made before considering the artery free of thrombus. Preoperative and intraoperative systemic heparinization (80 mg/kg bolus) should be used unless there is a contraindication (e.g., head injury). An activated clotting time (ACT) above 250 seconds is considered optimal. Liberal regional heparinization should be used with flushes of heparinized saline proximally and distally to prevent propagation of any thrombus.
and distal control away from the site of injury. Access is gained using the standard exposure techniques described in the following discussion. Vascular clamps should not be applied forcefully and blindly; instead, the artery should be completely dissected, looped with a silastic vessel loop, and clamped under direct vision. One important adjunct is the use of balloon occlusion catheters. This facilitates control in areas of difficult access and avoids excessive dissection. In addition, pressure cuff tourniquets may be used in the extremities to achieve prompt vascular control. Once control is gained, the hematoma is explored with careful attention to avoid injury to adjacent structures. The extent of vascular injury is assessed and clamps are moved closer to the vascular wound. The injured vessel should be debrided and cleaned using tenotomy scissors. The extent of debridement should take into consideration the mechanism of injury, with more extensive debridements for high-velocity gunshot wounds, and blast or crush injuries. One should avoid excising the adventitia of the vessel while dissecting or debriding the artery. Distal and proximal thrombectomy using a Fogarty balloon thromboembolectomy catheter should be performed even in the presence of relatively good prograde or retrograde bleeding. The size of the catheter is generally a 4 or 5 for the iliacs, 4 for the superficial femoral, 3 or 4 for the deep femoral, 2 or 3 for the tibials, and 2 for the pedal and smaller arteries of the forearm. Passage of thromboembolectomy catheters into the deep femoral, tibials, and smaller arteries should be done gently because of risk of arterial rupture, dissection, or intimal injury due to excessive balloon inflation. At least two “clean” passes should be made before considering the artery free of thrombus. Preoperative and intraoperative systemic heparinization (80 mg/kg bolus) should be used unless there is a contraindication (e.g., head injury). An activated clotting time (ACT) above 250 seconds is considered optimal. Liberal regional heparinization should be used with flushes of heparinized saline proximally and distally to prevent propagation of any thrombus.
Table 6-4. Basic Principles of Repair of Vascular Injuries | ||
|---|---|---|
|
Restoration of extremity perfusion does not always require definitive arterial reconstruction. Another important adjunct is a temporary arterial shunt placed in the proximal and distal arterial ends. This promptly controls hemorrhage and re-establishes inflow. Our preference is to use either a short or long Sundt intraluminal arterial shunt (Fig. 6-2). The shunt is secured to the artery using silk suture or a Rummel tourniquet. Although systemic heparinization is preferred, this is not an absolute requirement for shunt placement. The main advantage of temporary shunts is the avoidance of damage to a fresh arterial repair during subsequent orthopaedic manipulations in cases of comminuted, unstable skeletal injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree