Fig. 7.1
(A) Meniscus homologue. (B) Ulnar collateral ligament. (C) Radioulnar ligaments. (D) Articular disk. (E) Ulnocarpal ligaments
The articular disk is a triangular meniscus-shaped structure. It is thinner in its central portion and widens out in the more dorsal and palmar part, where it becomes in the radioulnar ligaments. Histologically speaking, in the union with the radius there exists a reinforcement of short collagenous fibers, oriented radially, with an extension of 1–2 mm., while the fibers of the rest of the disk have a greater tendency towards intertwining and are less organized. The area of the union of the short fibers with the rest of the articular disk is where there commonly take place the type ID tear [2].
The radioulnar ligaments stabilize the DRUJ joint. Ishii, in his anatomical study [3] shows how they have both a superficial and deep layer. The deep portion, called subcruentum ligament, is inserted in the fovea of the ulna, whereas the superficial part envelops the articular disk and becomes united to it in the more ulnar part. Nowadays it is known that the deeper part has greater importance in maintaining the stability of the distal radioulnar joint [4, 5].
The so-called meniscus homologue refers to the tissue, which is to be found between the superficial insertion of the radioulnar ligaments and the articular capsule [3]. In a certain anatomical study it has been postulated that it consists of the remains of a large apophysis of the ulnar styloid which, in primates, is joined to the pisiform and pyramidal [6].
The ulnar collateral ligament is a thick structure, which is inserted proximally into the base of the ulnar styloid and distally in the pisiform and triquetrum. It is in close contact with the ECU and distally its fibers converge with the meniscus homologue [7].
The last structure that forms the TFCC is the tendon sheath of the ECU. It is connected to the head of the ulna and the ulnar fovea by means of Sharpey fibers.
From a didactic viewpoint the TFCC has been compared to a tridimensional structure with two walls and a floor. The floor of this structure would be the articular disk and the volar and dorsal radioulnar ligaments; the palmar wall, would be formed by the ulnocarpal ligaments and the dorsal wall would be formed by the tendon sheath of the ECU.
The integrity of the TFCC is fundamental for two functions. The first of these maintains the stability of the distal radioulnar joint that, as has already been commented, is carried out fundamentally by the radioulnar ligament [4, 5, 8]. The second function refers to the correct transmission of the load. It is known that approximately 20 % of the wrist load is transferred through its ulnar border, that is to say, through the TFCC, so that any lesion may alter it [1].
Vascularization of the TFC
The ulnar artery is that which gives greater blood supply to the TFCC, above all in its ulnar portion. The more radial part is irrigated by means of volar and dorsal branches of the anterior interosseous artery.
In histological studies, such as those carried out by Bednar [9] and Thiru [10], it has been seen that the blood vessels penetrate into the TFCC from the periphery and can be observed only in an external 10–40 % of their size. These vessels may be observed above all in the dorsal, ulnar, and palmar area of the TFCC. Thus, the “radial and central portion” is relatively avascular, unlike the volar radial and dorsal radial, that is to say, the radioulnar ligaments.
It has been considered that the central area, as it has lesser vascular supply, it lacks a healing capacity. But Cooney [11] in a series of 23 patients with peripheral tears of the radial margin treated by open surgery, obtained good or excellent results in 80 % of the cases. By the same token he verified that 2 years after surgery, there still existed continuity of the reparation in four out of five patients.
That is, the fact that in histological studies the central area of the radial portion of the TFCC should not have a large number of vessels, does not mean that the radioulnar ligaments do not have them and neither does it mean that the healing may not be obtained after a correct bone bed preparation for the anchoring. In the same way that a meniscal lesion of the knee is not sutured in the white–white area, in the TFCC, healing is not attained by suturing a tear of the most central part (1A lesion), but the healing can be attained of the “central radial” portion with the radius (this would be a red–white area) or of the radioulnar ligaments with the radius (it would be a red–red area).
Diagnosis
Physical Examination
Patients with a radial lesion usually recall a traumatic precedent, above all in a fall with the wrist in hyperextension and ulnar deviation or also a sharp twist of the wrist.
The patient complains of pain and swelling in the ulnar area of the wrist and discomfort with the movements of ulnar deviation and pronosupination. If the lesion is a significant one and involves radioulnar instability, the dorsal prominence of the ulna may be observed but it should always be compared with the contralateral wrist in order not to confuse it with a hypermobile wrist.
There exist several exploration tests of the TFCC but in our view, the most useful ones are the three following ones (Fig. 7.2)
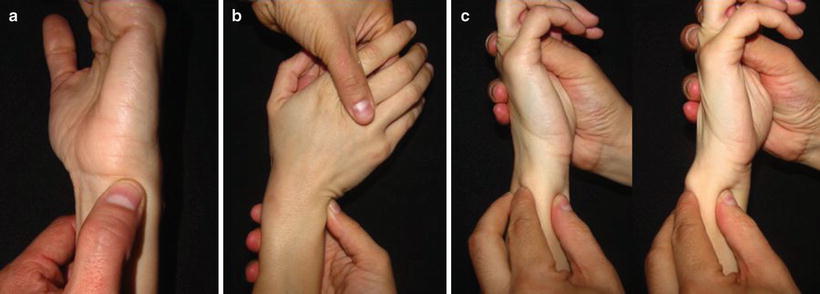
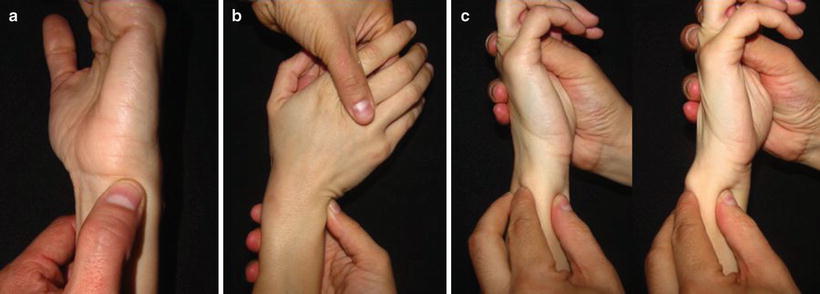
Fig. 7.2
(a) Ulnar fovea sign. (b) Ulnocarpal stress test. (c) Radioulnar instability exploration
Ulnar fovea sign [12]: with the elbow of the patient in a state of flexion, the thumb palpates the depression formed by the flexor carpi ulnaris, the ulnar styloid, the head of the ulna and the pisiform. It may be regarded as positive when pain appears compared with the contralateral. It is one of the most important signs in this kind of pathology, as it has a very high sensitivity and specificity (95 % and 87 % respectively).
Ulnocarpal stress test [13]: is carried out by the application of axial loading to the wrist in a state of maximal ulnar deviation while a movement of pronation and supination is applied. It is a very sensitive sign, but not a very specific one as it can be positive in a number of pathologies that affect the ulnar region of the wrist.
Radioulnar instability [5]: in order to evaluate the stability of the distal radioulnar joint, the ulna is displaced with respect to the radius in an anteroposterior plane with the wrist in a neutral position, in supination and pronation. These maneuvers should be carried out in both the affected side and the contralateral one, because instability should not be confused with articular laxness.
Diagnostic Modalities
Tears in the TFCC are not detected by simple radiographic examination, but they can reveal indirect data, which may indicate the possibility of a lesion. Thus, lateral and oblique and AP projections are useful to diagnose the presence of fractures-avulsions of the sigmoid notch and DRUJ instability as, with a complete radial desinsertion, the space of this joint will increase.
Tricompartmental arthrography has been the standard method used for the diagnosis of lesions of the intra-articular ligaments of the wrist [14]. It consists of a contrast injection under radiological control in the radiocarpal joint, midcarpal, and DRUJ. In presence of a radial tear there appears an extravasation of the contrast.
With the development of new technical advances in Magnetic Resonance Imaging (MRI), improvement has been achieved in the resolution and diagnosis of TFCC lesions, the former being the preferential technique of several authors [15, 16]. Arthro-MRI may add further information to the study and is shown to be superior to the standard MRI for the detection of complete tears of the TFCC [17].
The carrying out of helical computerized axial tomography (CT) together with arthrography combines the advantages of both techniques; the intra-articular structures and compartments remain distinctly defined in multiple planes. Thanks to this, the location of the tear may be determined with greater precision [18] and may be regarded as an alternative technique to that of Arthro-MRI [19].
But without any shade of doubt, the “gold standard” in the diagnosis of 1D-type lesions of the TFCC is still arthroscopy of the wrist, as it allows a direct visualization of the tear, determines the location and lesion type and detects other associated lesions.
Classification
In 1989, Palmer classified TFCC lesions in two large groups [1]. The first of these included traumatic lesions and he denominated them class 1, and the degenerative lesions class 2. Likewise, the traumatic lesions are subdivided according to their location, a central slit as 1A, ulnar tear as 1B, distal tear as 1C, and radial tear as 1D.
Radial tears are avulsions of the TFCC from the radial sigmoid notch and may or not include bone fragments.
Although controversy exists as to what a ID tear is and what it is not, one of the best classifications which define them is that of Nakamura [20] who subdivided the radial lesions of the TFCC into six groups (Fig. 7.3)
Fig. 7.3
(a) Fibrocartilage tear between the hyaline cartilage of the sigmoid notch of the radius and TFCC. (b) Dorsal edge tear between the dorsal edge of the sigmoid notch of the radius and dorsal portion of the radioulnar ligament. (c) Palmar edge tear between the palmar edge of the sigmoid notch of the radius and palmar portion of the radioulnar ligament. (d) Combination of (a) + (b). (e) Combination of (a) + (c). (f) Complete detachment of the TFCC from the sigmoid notch of the radius
(a)
Fibrocartilage tear between the hyaline cartilage of the sigmoid notch of the radius and TFCC.
(b)
Dorsal edge tear between the dorsal edge of the sigmoid notch of the radius and dorsal portion of the radioulnar ligament.
(c)
Palmar edge tear between the palmar edge of the sigmoid notch of the radius and palmar portion of the radioulnar ligament.
(d)
Combination of (a) + (b).
(e)
Combination of (a) + (c).
(f)
Complete detachment of the TFCC from the sigmoid notch of the radius.
As has already been seen, the stability of the DRUJ depends on the integrity of the radioulnar ligaments and thus a type 1D-a may not be associated with DRUJ instability, whereas a type 1D-b–f can induce DRUJ instability.
Further doubt may exist with regard to differentiating a 1D-a lesion (radial lesion) from a 1A lesion (central lesion), as the only difference is a few millimeters of fibrocartilage tissue. In our view, the most important thing is to determine the treatment to be carried out rather than an evaluation as to whether a fibrocartilage tissue exists or not between the tear and the radius.
We would advocate a debridement of the portion of the fibrocartilage united to the radius and an evaluation as to whether the articular disk can be approximated to the radius without tension. If this is the case, the reattaching of the lesion would be carried out and we would denominate it 1D-a. If the disk cannot be approximated without tension, only the debridement would be carried out and the lesion would be classified as 1A (Fig. 7.4)
Fig. 7.4
(a) After the debridement the articular disc can be approximated without tension to the radius sigmoid notch. We would classify the lesion as Ida and the reattachment back down to the bone could be made. (b) After the debridement the articular disc cannot major be approximated without tension to the radius sigmoid notch. We would classify the lesion as IA and only a debridement would be carried out
Treatment
Conservative Treatment
Treatment in the acute phase of lesions of the TFCC, not associated with clinical instability, includes immobilization for 3–4 weeks, nonsteroid anti-inflammatories, steroid injections and, physiotherapy.
Indication of Surgical Treatment
Both the failure of a conservative treatment, without improvement after 3 months and the existence of associated distal radioulnar instability, indicate the need for surgical treatment.
Surgical Treatment
Many classical papers advocate the treatment of most of the lesions of the TFCC by means of debridement or excision [21, 22]. This practice has been supported by a study, which concludes that the resectioning of at least two thirds of the articular disk does not influence in the DRUJ biomechanics [23]. However, in this study the peripheral margins of the TFCC were respected, that is to say, the radioulnar ligaments. More recent studies have highlighted the importance of the integrity of these ligaments in order to maintain DRUJ stability [4, 5]. This has increased the interest of many authors to repair the TFCC instead of a debridement.
In the case of radial side tears, there exists greater agreement on carrying out a repair when the radioulnar ligaments are affected. As we have seen supra, these ligaments are vascularized structures with potential healing. Greater doubt exists with regard to the repair of a central radial tear without affecting the radioulnar ligaments but, as we have already mentioned, our view is that, if after the debridement the articular disk can be approximated without tension, we would advocate its repair back to the bone. With this reparation we believe that there may be avoided a possible progression towards the radioulnar ligaments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








