Management of the Stiff Total Knee Arthroplasty
Raymond H. Kim
Douglas A. Dennis
INTRODUCTION
Although total knee arthroplasty (TKA) has been a successful procedure with excellent survivorship and functional outcomes (1, 2, 3, 4), it is not without complications. One of these possible complications is postoperative stiffness. One analysis of knee motion demonstrated a requirement of 67 degrees of flexion for the swing phase of gait, 83 degrees to ascend stairs, 84 degrees to descend stairs, and at least 93 degrees to rise from a chair (5). It is reasonable to describe a stiff TKA as a knee that limits activities of daily living secondary to lack of motion. In a study on stiffness following TKA, Kim and Lotke et al reviewed 1,000 consecutive knees (6). At 32 months postoperatively, there was a 1.3% prevalence of stiffness, defined as a flexion contracture of greater than or equal to 15 degrees or maximal flexion less than 75 degrees.
This chapter to reviews the etiologies, evaluation strategies, and management options for patients who develop stiffness after undergoing a TKA.
ETIOLOGY
The etiology of stiffness after TKA is multifactorial and can be attributed to three general causes: patient factors, technical errors, and surgical complications. Although technical errors and surgical complications may be treatable causes of stiffness by manipulation, scar excision, or revision total knee arthroplasty, patient-related factors are less effectively treated with revision surgery and should most often be avoided.
Patient Factors
Numerous patient factors can contribute to postoperative restriction of knee motion. Multiple studies have shown that the primary determinant of postoperative ROM is preoperative ROM (7, 8, 9, 10, 11). This is likely because of patients’ individual anatomy, particularly their soft tissues, as well as the severity and chronicity of their arthritic disease. Ritter and Stringer reviewed 145 consecutive TKA patients and found that the degree of postoperative flexion was determined by the preoperative flexion, particularly if the degree of flexion was less than 75 degrees (7,8). Obesity often limits postoperative knee motion because of increased lower extremity girth, resulting in earlier calf-thigh impingement (12). Cutaneous factors include scarring from multiple incisions, burns, and previous radiation therapy, which can all lead to superficial restriction of flexion (Fig. 32-1).
 FIGURE 32-1 Photograph demonstrating excessive cutaneous scarring of the anterior aspect of the knee. |
Another significant patient factor involves inadequate postoperative rehabilitation. The patient’s understanding of the postoperative recovery should be cultivated preoperatively by providing detailed education preoperatively (“prehabilitation”). Emphasis on early mobilization, diligence in attending physical therapy sessions, and goal setting is critical.
Adequate pain control perioperatively also influences patient compliance with therapy participation. Pre-emptive analgesics, regional nerve blocks, and postoperative pain control should be optimized to maximize the patient’s efforts when performing knee ROM exercises (13,14). Diligence with anticoagulation monitoring is critical to prevent hemarthroses that can result in painful swelling and significantly delay gains in knee motion during the postoperative rehabilitation period.
Technical Errors Limiting Extension
Good surgical technique is the most critical factor in the surgeon’s ability to minimize the incidence of postoperative stiffness. Intraoperative technical errors can result in either decreased extension (flexion contracture) and/or decreased flexion. Decreased extension can result from poor balancing of the flexion-extension gaps, failure to remove posterior osteophytes, or failure to release a tight posterior capsule.
An excessively tight extension gap will often result in lack of full extension. Assuming the level of resection for the tibial cut was appropriate, one cause of a tight extension gap is an inadequate distal femoral resection. For patients with a preoperative flexion contracture, the surgeon can anticipate the need to resect an additional couple of millimeters of distal femur when setting the distal femoral cutting block to ensure an adequate extension gap. After the distal femur and proximal tibial cuts are made, the extension gap should be assessed for the gap height as well as the symmetry of the gap medially and laterally. This can be performed using spacer blocks, laminar spreaders, or other tensioning device. If the extension gap is asymmetric medially compared to laterally, appropriate releases should be performed at this time to obtain a balanced extension gap.
Large, posterior osteophytes on the femoral condyles can tent the posterior capsule and mechanically inhibit full extension. Osteophytes are most simply removed after making the anterior and posterior condylar resections on the distal femur. To remove the osteophytes, the knee can be placed at 90 degrees of flexion with a laminar spreader in the lateral compartment. A three-quarter-inch curved or angled osteotome can then be used to sharply chisel off the medial posterior osteophyte at the osteochondral junction (Fig. 32-2). This can then be repeated in the lateral compartment after switching the laminar spreader to the opposite side. The flexion and extension gaps can then be reassessed to determine if further balancing is required. In cases with massive posterior compartment osteophytes, it is often wise to attempt to remove them before extensive soft tissue releases are
performed, because removal of large osteophytes can have a dramatic effect on both the coronal and sagittal plane balance.
performed, because removal of large osteophytes can have a dramatic effect on both the coronal and sagittal plane balance.
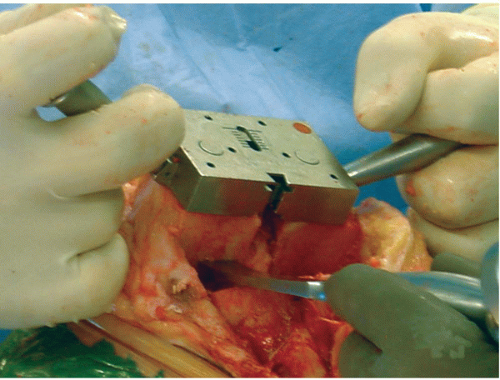 FIGURE 32-2 Intraoperative photograph demonstrating removal of posterior femoral osteophytes using a curved osteotome. |
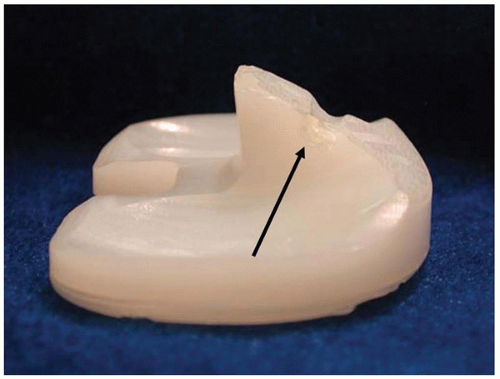 FIGURE 32-3 Photograph demonstrating anterior postimpingement secondary to excessive femoral component flexion in conjunction with increased posterior tibial slope. |
Premature extension impingement of the femoral and tibial components can occur if components of a posterior stabilized knee are malpositioned in the sagittal plane. Excessive flexion of the femoral component or a tibia prepared with too much posterior slope will result in prosthetic mechanical impingement of the intercondylar portion of the femoral component against the anterior aspect of the tibial stabilizing post that will inhibit extension and could potentially result in accelerated post wear (Fig. 32-3). Care should be taken to avoid flexing the distal femoral cut by ensuring that the entry hole for the intramedullary distal femoral cutting guide is not placed too posteriorly. Slope of the extramedullary tibial cutting guide should be carefully checked before making the proximal tibial cut to make sure excessive posterior slope is avoided.
In patients with long-standing significant preoperative flexion contractures, the posterior capsule of the knee is often significantly contracted. If adequate distal femoral resection has been performed, yet a tight extension gap persists, a posterior capsular release should be performed. The authors prefer to perform this bluntly with a Cobb elevator, gently elevating the posterior capsule directly off of the posterior femur. Care should be taken not to stray off of the bone with instruments to minimize the risk of harming neurovascular structures. Assistants should also avoid holding the leg behind the knee to prevent ballottement of the neurovascular bundle anteriorly as the posterior capsular release is performed.
Technical Errors Limiting Flexion
Technical errors known to limit flexion after TKA include flexion-extension gap imbalance, retention of posterior femoral condylar osteophytes, failure to restore posterior femoral condylar offset, and substantial elevation of the joint line. Excessive flexion gap tension typically leads to limited motion and can result from multiple errors such as insufficient bone resection, use of oversized components (18), inadequate ligamentous release, or component malposition. Conversely, leaving a flexion gap too loose in a posterior cruciate ligament (PCL)-retaining TKA often results in paradoxical femoral translation, which anteriorizes the axis of knee flexion, results in earlier posterior impingement of the femur on the tibial component, and decreased weight-bearing flexion (19, 20, 21).
If a knee is unbalanced with an excessively tight flexion gap relative to the extension gap, and a tibial insert is selected to accommodate the extension gap, then the knee will resist flexion because of an overstuffed flexion space. Excessive flexion gap tightness can also result from placement of the tibial component with an anterior slope or from errors associated with femoral component position or size. Placing the femoral component too posteriorly tightens the flexion gap and may limit flexion. If the femoral component is placed in excessive flexion, the anterior flange tightens
the extensor mechanism and can cause chronic tendinous irritation. Finally, if the femoral component is placed in internal rotation, arthrofibrosis has been shown to occur, possibly by asymmetrically tightening the medial aspect of the flexion gap. Boldt et al identified and analyzed 38 TKA subjects with postoperative arthrofibrosis from a cohort of 3,058 consecutive mobile-bearing patients (22). They compared these stiff TKA patients with a matched control group of 38 asymptomatic, mobile-bearing TKA subjects without arthrofibrosis. Computerized axial tomography scans were obtained in both groups. The surgical epicondylar axis was compared with the posterior condylar axis of the femoral prosthesis. Femoral components in the arthrofibrosis group were significantly internally rotated relative to the transepicondylar axis by a mean of 4.7 degrees (SD, 2.2 degrees; range, 10 degrees internal to 1 degree external rotation). In the control group, the femoral components were positioned at a mean of 0.3 degrees internal rotation relative to the transepicondylar axis (SD, 2.3 degrees; range, 4 degrees internal to 6 degrees external rotation).
the extensor mechanism and can cause chronic tendinous irritation. Finally, if the femoral component is placed in internal rotation, arthrofibrosis has been shown to occur, possibly by asymmetrically tightening the medial aspect of the flexion gap. Boldt et al identified and analyzed 38 TKA subjects with postoperative arthrofibrosis from a cohort of 3,058 consecutive mobile-bearing patients (22). They compared these stiff TKA patients with a matched control group of 38 asymptomatic, mobile-bearing TKA subjects without arthrofibrosis. Computerized axial tomography scans were obtained in both groups. The surgical epicondylar axis was compared with the posterior condylar axis of the femoral prosthesis. Femoral components in the arthrofibrosis group were significantly internally rotated relative to the transepicondylar axis by a mean of 4.7 degrees (SD, 2.2 degrees; range, 10 degrees internal to 1 degree external rotation). In the control group, the femoral components were positioned at a mean of 0.3 degrees internal rotation relative to the transepicondylar axis (SD, 2.3 degrees; range, 4 degrees internal to 6 degrees external rotation).
Excessive femoral component flexion can be avoided by ensuring that the entry hole for the intramedullary distal femoral cutting guide is not placed too posteriorly. To avoid oversizing the femoral component, preoperative templating is helpful to estimate the femoral component size on appropriately scaled lateral radiographs. Most TKA systems determine femoral component sizing based on a guide referencing the anterior cortex of the femur and the posterior condyles. When using the sizing guide, care should be taken to clearly identify the anterior cortex. Failure to identify the anterior cortex because of overlying hypertrophic synovium can lead to oversizing the femoral component.
In addition to varus-valgus ligamentous balance, balance of the PCL has been shown to be an important determinant of knee flexion following PCL-retaining TKA. Leaving a PCL too tight will inhibit flexion by creation of an overly tight flexion gap. Conversely, overreleasing of the PCL, particularly in minimally constrained PCL-retaining TKA designs, may result in paradoxical anterior femoral translation during deep, weight-bearing flexion resulting in a reduction in knee flexion as previously discussed (19,23). Because of the paradoxical anterior sliding, posterior femoral rollback is inhibited, which is necessary to avoid posterior impingement and to allow higher magnitudes of knee flexion.
Technical errors resulting in failure to obtain symmetry (rectangular gap) of either the flexion or extension gap can similarly result in diminished flexion. Matsuda et al evaluated coronal plane (varus-valgus) stability following TKA by applying a 150 Newton load using a Telos arthrometer (Fa Telos; Medizinisch-Technische GmbH, Griesheim, Germany) (24). Knees were judged to be balanced if the difference in varus and valgus laxity was less than 2 degrees. In the balanced TKA group (n = 69 TKA), mean flexion improved 10 degrees postoperatively (p < .0001), whereas in the unbalanced TKA group (n = 11 TKA), mean postoperative flexion was reduced by 8.3 degrees (p = .0061), emphasizing the importance of having a balanced extension gap.
A well-balanced flexion gap is one that is not only equivalent in height to the extension gap, but one that is also symmetric medially and laterally, thus creating a rectangular flexion gap. Because of the association of femoral component malrotation with arthrofibrosis previously discussed, the authors prefer to use a gap-balancing technique as opposed to the measured-resection technique to ensure proper balancing of the flexion and extension gaps. The critical step in this technique involves placement of the anterior-posterior cutting block, which determines the rotation of the femoral component. The anterior-posterior distal femoral cutting block is positioned anteriorly or posteriorly to ensure the flexion gap height is equal to the extension gap height with the collateral ligaments equally tensioned with laminar spreaders or another tensioning device. The rotation of the anterior-posterior cutting block is then appropriately adjusted rotationally to also ensure that the flexion gap space itself is symmetric medially and laterally and parallel to the tibial cut with each collateral ligament equally tensioned (Fig. 32-4). Secondary checks are then performed to ensure reasonable rotational orientation relative to the transepicondylar and anteroposterior axes. Using this technique facilitates obtaining balanced flexion and extension gap heights as well as a rectangular flexion gap that is symmetric medially and laterally.
Although retention of large posterior femoral osteophytes can result in postoperative flexion contracture as previously discussed, numerous reports have documented that retention of these osteophytes reduces knee flexion as well (25, 26, 27




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








