Fig. 10.1
Dorsal scaphoid translation and cartilage loss on proximal scaphoid on sagittal plane MRI
Computed Tomography
Recently Kakar described a novel imaging technique for 4D CT imaging (3D + time) which has promising clinical utility in accurately diagnosing SL instability [21]. 4D CT allows dynamic image data (4D movies) to be recorded whilst the patient moves their wrist through various movements including radial-ulnar deviation, flexion-extension, and dart thrower’s motion.
Classification of SLL Pathology
This table summarizes the various methods of classifying SL ligament pathology and identifies what level of pathology each type of assessment can ascertain (Table 10.1). Various systems for classifying SLL pathology have been described, both temporally and structurally.
Table 10.1
Classification of SLL pathology
Classification type | Description | ||
|---|---|---|---|
Temporal | Acute | ||
Subacute | |||
Chronic | |||
Structural | Imaging | Radiographs | Static radiographs—complete static dissociation |
Dynamic radiographs/fluoroscopy—complete dynamic dissociation | |||
MRI | Incomplete and partial •Dorsal band •Membranous •Volar band | ||
Complete—dynamic or static | |||
Arthroscopic | Geissler classification | See Table 10.2 for detail | |
Operative | Incomplete | ||
Complete | Dynamic | ||
Static •Reducible •Irreducible | |||
Temporal Classification
There is no clear consensus on what constitutes acute, subacute, and chronic injuries. Whichever criteria are used, the principle aim is to define the potential for healing of the native ligament.
Larsen et al. classified carpal instability in a temporal way. Acute was defined as less than a week old, subacute was defined as between 1 and 6 weeks, and chronic was described as more than 6 weeks old [22].
Geissler and Haley defined an acute injury as up to 3–4 weeks old. Subacute was defined as an injury more than 3–4 weeks old and up to 6 months old. A chronic injury was defined as symptoms present greater than 6 months [23].
The current trend has been to consider injuries as “chronic” at an earlier time point due to the observed poorer outcomes in terms of radiographic maintenance of SL gap after direct ligament repair, at relatively early intervals after the apparent index injury.
This lack of consensus as to what constitutes an acute injury means that algorithms for management based on temporal classification remain inconsistent.
Clinical Examination Classification Systems
Clinically we can define four types of instability: (1) predynamic instability; (2) dynamic instability; (3) reducible static instability; (4) nonreducible instability [24]. Predynamic instability was initially termed by Kirk Watson [7] and applies to instability that may be observed clinically on physical examination but not by radiographic studies, and corresponds to a Geissler grade I or II instability [23]. Dynamic SL instability is applied to a complete SL ligament tear, but the secondary scaphoid stabilizers remain intact [25]. SL instability can be observed radiographically under loaded conditions or in specific wrist positions, “clenched fist” or loading the wrist in ulnar deviation. Static reducible SL dissociation occurs when the ligament tear is chronic and irreparable; the secondary stabilizers are insufficient and a DISI deformity results; carpal subluxation is reducible [24].
Structural Classification
A structural classification can be based on imaging studies, or arthroscopic or open operative evaluation. Imaging studies may be static X-ray films, stress/positional radiographs, fluoroscopy, ultrasound, or MRI.
Arthroscopic Structural Classification
The key to treatment of SL ligament complex pathology is recognition of what is normal and what is pathological anatomy. Both the radiocarpal and midcarpal spaces must be evaluated arthroscopically when carpal instability is suspected. Wrist arthroscopy is usually not considered complete if the midcarpal space has not been evaluated, particularly with a suspected diagnosis of carpal instability.
The SLL is best visualized with the arthroscope in the 3-4 portal. It should have a concave appearance as viewed from the radiocarpal space (Fig. 10.2). In the midcarpal space, the SL interval should be tight and congruent without any step-off (Fig. 10.3). This is in contrast to the lunotriquetral (LT) interval, in which a 1-mm step off occasionally is seen which is considered normal and slight motion is seen between the lunate and triquetrum. When it tears, the SLIL hangs down and blocks visualization with the arthroscope in the radiocarpal space from the 3-4 portal. The normal concave appearance between the carpal bones becomes convex. However, the degree of rotation of the carpal bones and any abnormal motion or separation is best appreciated from the unobstructed view available in the mid-carpal space.



Fig. 10.2
Arthroscopic view of the normal concave appearance of the SLIL as seen from the 3-4 portal in the radiocarpal space

Fig. 10.3
Arthroscopic view of the normal, tight, congruent SL interval as seen from the midcarpal space
A spectrum of injury to either the SL or LT interosseous ligament is possible. The interosseous ligament appears to attenuate and then tear from volar to dorsal. Geissler devised an arthroscopic classification of carpal instability and suggested management of acute lesions to the interosseous ligament (Table 10.2) [23, 25]. The management options as listed from this original article have evolved as the understanding of the compromise of ligament healing potential over time has changed.
Table 10.2
Geissler arthroscopic classification of carpal instability
Grade | Description | Management |
|---|---|---|
I | Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. No incongruency of carpal alignment in the midcarpal space | Immobilization |
II | Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. Incongruency/step-off as seen from the midcarpal space. A slight gap (less than width of probe) between carpals may be present | Arthroscopic reduction and pinning |
III | Incongruency/step-off of carpal alignment is seen in both the radiocarpal and mid carpal space. The probe may be passed through gap between carpals | Arthroscopic/open reduction and pinning |
IV | Incongruency/step-off of carpal alignment is seen in both the radiocarpal and mid carpal space. Gross instability with manipulation is noted. A 2.7 mm arthroscope may be passed through the gap between carpals | Open reduction and repair |
In Grade I injuries, there is loss of the normal concave appearance of the scaphoid and lunate as the interosseous ligament bulges with the convex appearance (Fig. 10.4). Evaluation of the SL interval from the midcarpal space shows the SL interval still to be tight and congruent. These mild Grade I injuries usually resolve with simple immobilization.
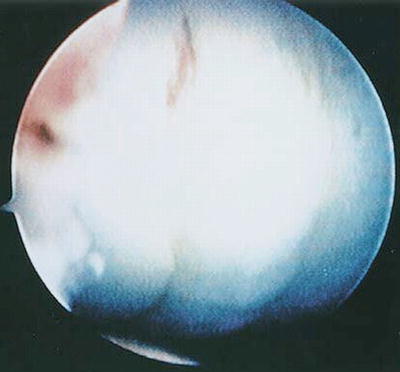
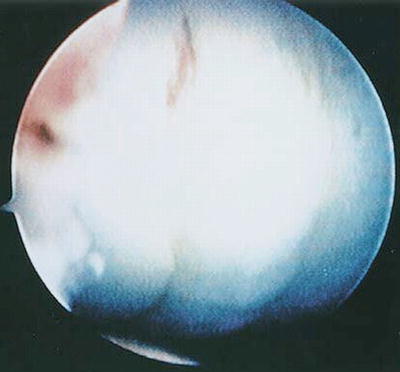
Fig. 10.4
Arthroscopic view of a Grade I interosseous ligament injury to the SLIL as seen from the 3-4 portal in the radiocarpal space. Note that the normal concave appearance at the SL interval has now become convex
In Grade II injuries, the interosseous ligament bulges similarly to grade I injuries as seen from the radiocarpal space. In the midcarpal space, the SL interval is no longer congruent. The scaphoid flexes and its dorsal lip is rotated distal to the lunate (Fig. 10.5). This can be better appreciated with the arthroscope placed in the ulnar midcarpal portal looking across the wrist to assess the wrist to assess the amount of flexion to the scaphoid. This is analogous to the dorsal translation of the proximal pole of the scaphoid that can be identified on sagittal plane MRI imaging (Fig. 10.1).
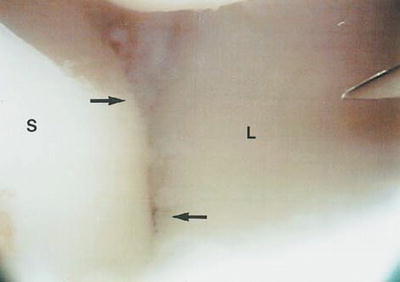
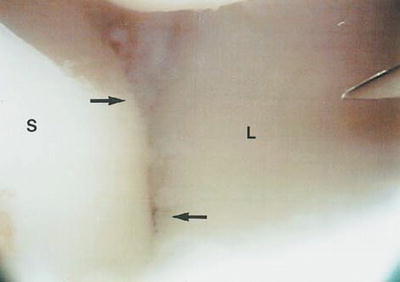
Fig. 10.5
Arthroscopic view of a Type II SLIL injury as seen from the radial midcarpal space. The dorsal lip of the scaphoid is no longer congruent with the lunate as it is palmar flexed. (S scaphoid, L lunate)
In Grade III injuries, the interossesous ligament starts to separate, and a gap is seen between the scaphoid and lunate from both the radiocarpal and midcarpal space. A 1 mm probe may be passed through the gap and twisted between the scaphoid and lunate from both the radiocarpal and midcarpal spaces (Fig. 10.6). Sometimes the gap between the scaphoid and lunate is not visible until the probe is used to push the scaphoid away from the lunate. A portion of the dorsal SLIL may still be attached.
Fig. 10.6
Arthroscopic view of a Type III SLIL tear as seen from the radial midcarpal space. Note the gap between the scaphoid and lunate (S scaphoid, L lunate)
In Grade IV injuries, the interosseous is completely torn, and a 2.7 mm arthroscope may be passed freely from the midcarpal space to the radiocarpal space between the scaphoid and lunate (the drive-through sign) (Fig. 10.7). This corresponds to the widened SL gap seen on plain radiographs with a complete SL dissociation.
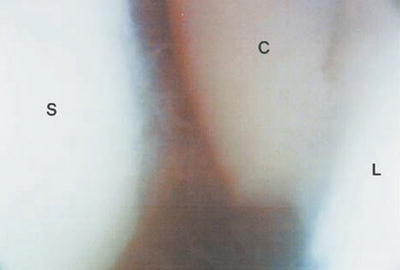
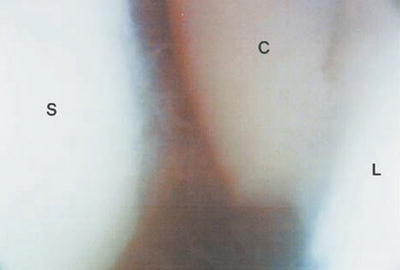
Fig. 10.7
Arthroscopic view of a Type IV SLIL tear. The scaphoid and lunate are completed separated, and the arthroscope may pass freely between the radiocarpal and midcarpal spaces. The capitate is seen between the SL intervals (S scaphoid, L lunate, C capitate)
Radiographic Structural Classification
Incomplete/Partial Rupture: Dorsal, Membranous, Volar Band
Partial rupture—usually only the palmar band of ligament is ruptured or occasionally only the dorsal segment is ruptured.
Static and dynamic radiographs are usually normal. Chronicity of the injury and partial healing may also be identified with high-resolution MRI scanning. Dorsal translation of the proximal pole relative to the facet of the radius may be identified on sagittal plane MRI images in spite of normal static plain radiographic alignment and may be an early indicator of functionally more significant partial injury. Early chondral loss on the proximal pole may also be identified on MRI before plain radiographic abnormality.
Complete Rupture: Static vs. Dynamic
Static vs. Dynamic dissociation is best identified by comparing static vs. stress radiographs, or by fluoroscopy.
1.
Complete rupture—dynamic—All components of SLIL are ruptured but the extrinsic ligaments/secondary stabilizers are usually intact. Static plain radiographs may be normal but there is disruption of normal relationships on stress radiographs.
2.
Complete rupture—static—Complete SL ligament rupture and extrinsics also injured and static plain radiographs demonstrate widened SL interval on PA radiographs and increased SL angle on the lateral radiographs (modified by Watson) [26].
Static Reducible vs. Static Irreducible
This is determined intraoperatively. Static deformity is present on resting plain radiographs. It may be easily reducible during surgery to repair or reconstruct the SLIL. When deformity is not reducible intraoperatively salvage options should be utilized. This usually follows a temporal relationship with the more chronic ruptures leading to a static deformity, which may then become irreducible.
Treatment
Correct classification of the injury can assist in selection of appropriate treatment options. Nonetheless the greatest challenge is that there is no consensus on which surgical treatment option should be undertaken. Various options exist including pinning, repair, capsulodesis, and reconstruction and each have been applied to virtually all grades of injury. Moreover, surgical interventions can be either open or arthroscopic.
The authors have defined a unified classification system for treatment options of SL ligament complex pathology (Table 10.3).
Table 10.3
Classification system for treatment options for SL pathology
Treatment options | ||
|---|---|---|
Closed pinning | Fluoroscopic guided | |
Arthroscopic guided | ||
Open repair and pinning | ||
Capsulodesis, capsulorrhaphy and partial repair | Arthroscopic—volar or dorsal | “Abrasion” capsulorrhaphy |
Shrinkage | ||
Suture | ||
Open | Dorsal—Blatt/reverse Blatt (often adjunct to open repair or reconstruction) | |
Reconstruction: defined as an attempt to re-establish a soft tissue relationship between scaphoid and lunate ± stabilisation through other soft tissue augmentation) | Local tissue | Dorsal intercarpal ligament |
RASL (arthroscopic or open) | ||
Free tissue grafts—“Bone–Tissue–Bone” | Bone–Retinaculum–Bone | |
Hand/wrist graft options | ||
Foot/tarsal graft options | ||
Other tissue | ||
Tendon grafts | Brunelli | |
Three ligament tenodesis | ||
Scapholunate axis method | ||
Scapho-luno-triquetral tenodesis | ||
Salvage | PRC [59] | |
Partial fusion (arthroscopic or open) | Four-corner fusion ±e/o scaphoid | |
Radio-scapho-lunate fusion | ||
Capitolunate fusion | ||
STT fusion | ||
Total wrist fusion | ||
Closed Pinning: Image Intensifier or Arthroscopically Guided
This surgery may be appropriate for acute lower grade injuries.
The wrist is evaluated arthroscopically for direct visualization of SLL injury and indirect evidence of disordered intercarpal mechanics. Arthroscopic assessment is achieved through the preferred means of arthroscopy and traction. The wrist may be suspended at approximately 10 lbs of traction in a traction tower [27, 28]. Alternately traction may be applied with the forearm horizontal using a variety of traction devices [28, 29]. The 3-4 portal is the most ideal viewing portal for visualization of the SLL. A working 4-5 or 6-R portal is also used. The wrist is systematically evaluated from radial to ulnar. The SL interval is probed. The degree of injury may not be fully appreciated until the tear is palpated with a probe (Fig. 10.8). Torn fibers of the SLL, if present, are then debrided with the arthroscope in the 6-R portal, and a shaver inserted into the 3-4 portal. A probe is inserted into the SL interval to note particularly any gap between the scaphoid and lunate. Following arthroscopic debridement of a torn SLL from the radiocarpal space, the midcarpal space is then evaluated. The arthroscope is initially placed in the radial midcarpal space. Close attention is paid to any rotational displacement of the scaphoid with the dorsal lip being rotated distal to that of the lunate. This may be best visualized with the arthroscope placed in the ulnar midcarpal portal. Also, any gap where the probe or arthroscope itself can be passed between the scaphoid and lunate is identified. If this is achieved easily then there are serious doubts as to whether closed pinning is appropriate [28].


Fig. 10.8
Arthroscopic view of a Type II SLIL tear as seen from the 3-4 portal in the radiocarpal space. A probe is used to palpate the interosseous ligament and the separation which was not initially noted, is identified
Patients with a Grade II lesion may be most ideally suited for arthroscopic-assisted reduction and pinning although efficacy of this treatment must me be interpreted in the context of the interval since injury, which will affect the healing potential. Alternate treatment options with arthroscopic capsular abrasion or shrinkage have also been advocated for Grade II pathology particularly in more chronic injury and will be discussed later. Use of closed pinning for Grade III injuries is difficult to justify based on current literature.
For arthroscopic pinning the arthroscope is placed in the 3-4 portal after the midcarpal space has been evaluated in patients who have an acute or perhaps subacute Grade II SLIL injury. A 0.045 Kirschner wire (k-wire) is inserted through a soft tissue protector or through a 14-G needle placed dorsally in the anatomic snuff-box to the scaphoid. A soft tissue protector may be used in order to avoid injury to the sensory branches of the radial nerve. A small incision is made, and blunt dissection is continued down with a hemostat; a soft tissue protector may be placed directly on the scaphoid.
The k-wire can then be seen as it enters the scaphoid with the surgeon looking down the radial gutter with the arthroscope. In an easier alternative technique, the wrist is taken out of traction and the k-wires can be positioned under fluoroscopic control. If there is concern regarding the reduction then placing the arthroscope in the ulnar mid-carpal portal during stabilization allows the surgeon to look across the wrist to better judge the rotation of the scaphoid in relation to the lunate.
Additionally, a probe may be inserted through the radial midcarpal space to control the palmar flexion of the scaphoid. The wrist may be extended and ulnar deviated to help further reduce the palmar flexion of the scaphoid. After the first wire is placed controlling the reduction, an additional wire may be placed in the SL interval. Placement of wires between scaphoid and capitate remains controversial. A scapho-capitate wire gives excellent control of scaphoid rotation but some authors have questioned the advisability of violating the uninjured scapho-capitate articulation. In addition, immobilization of the midcarpal joint through scapho-capitate wires may be considered undesirable in the context of renewed interest in the “Dart throwing” plane of motion.
The k-wires are best buried under the skin as this avoids secondary infection and need for premature removal. The wrist is immobilized in a below elbow thermoplastic splint. Gentle inner range radiocarpal flexion-extension range of motion exercise is usually possible, as restricted by the wires. The k-wires are then removed in theater after 6–8 weeks. Grip strength exercises for the wrist are initiated at 3 months.
Treatment for patients with Grade III and Grade IV injuries to the SLL, either acute, subacute, or chronic remains unclear. Results of closed treatment for higher-grade injuries have largely been unsatisfactory [30] and the dichotomy between repair and reconstruction has remained difficult to clarify. There has undoubtedly been a trend toward earlier adoption of reconstruction for higher-grade injuries.
Whipple reviewed the results of arthroscopic management of SL instability, utilizing the previously described techniques in patients who were followed for 1–3 years [31]. In his series, patients were classified into two distinct groups of 40 patients each, according to the duration of symptoms and the radiographic SL gap. Thirty-three patients (83 %) who had a history of instability for 3 months or less and had less than 3 mm side-to-side difference in the SL gap had maintenance of the reduction and symptomatic relief. When symptoms were present for greater than 3 months and there was more than a 3 mm side-to-side SL gap only 21 patients (53 %) had symptomatic relief following arthroscopic reduction and pinning. Patients with less than 3 months symptoms duration and 3 mm side-to-side SL gap were followed for 2–7 years. Whipple found that 85 % continued to maintain their stability and comfort in his series. This report emphasized the need for early diagnosis and intervention prior to the onset of fixed carpal alignment and diminished capacity for ligamentous healing.
Open Repair and Pinning
Patients with acute Grade III and Grade IV injuries to the SLIL are best treated with open repair or reconstruction. The efficacy of direct repair remains controversial; however, there is little doubt that the trend is toward earlier adoption of reconstructive techniques rather than direct repair due to the strong impression that complete ruptures lose the capacity for primary healing very soon after injury. The critical interval has not been defined and indeed it may be that once a complete rupture of the SLIL has occurred the potential for healing may be compromised. Furthermore the tear morphology may influence the healing potential. When the ligament is avulsed from either the scaphoid or lunate, it may have a greater capacity to heal than a midsubstance rupture. Prior to arthrotomy, the wrist is evaluated arthroscopically for any additional injuries, including potential cartilaginous loose bodies, triangular fibrocartilage complex tears, and possible injury to the LT interosseous ligament. Open repair is undertaken through a dorsal 3-4 extensor compartment approach. A Berger ligament sparing arthrotomy [32] is preferred by the authors. It is essential that an intraoperative assessment is made as to the healing potential of the residual ligament and alternate reconstructive or salvage procedures undertaken if the residual ligament is of poor quality or there is concern regarding the cartilage surfaces of the carpus and radius.
Capsulodesis, Capsuloraphy, and Partial Repair
Restraint of scaphoid flexion has long been identified as a desirable intervention in the treatment of SL pathology [33–35]. The dorsal subluxation of the proximal scaphoid and loss of congruence of the distal pole in relation to the radial styloid have long been considered the principal initial biomechanical abnormalities requiring intervention. Procedures that restrict scaphoid flexion have been advocated as an alternative to repair or reconstruction. There is no consensus as to when such alternate stabilizing procedures should be undertaken in preference to repair or other reconstructive options.
Arthroscopic Techniques for Capsulodesis, Capsuloraphy, and Partial Repair
Abrasion Capsulodesis
Although not previously reported in the literature, a new surgical technique receiving attention is abrasion capsulodesis. Although alternative arthroscopic capsular tightening has been reported with thermal shrinkage there are some concerns given the adverse experience of thermal techniques in the shoulder. Although there have not been reports of similar problems in the wrist, abrasion of the dorsoradial capsule has been considered as a safer alternative. In lower grade injuries this may improve stability by inciting a scar reaction with an increase in the extrinsic restraint to scaphoid flexion. The dorsal radial capsule is abraided with a chondrotome blade to stimulate a scar reaction. Consideration may be given to temporary k-wire pinning (either SL or scapho-capitate) to prevent scaphoid flexion, and flexion is usually restricted for 4–6 weeks with a thermoplastic splint. This technique is currently being studied in a prospective cohort by Ross and colleagues in Brisbane.
Arthroscopic Dorsal Capsular Thermal Shrinkage
Thermal capsular shrinkage using a thermal probe has been suggested in the treatment of Grade 2 injuries [36]. Although this technique demonstrated a number of unsatisfactory results in treatment of anterior shoulder instability, it has been argued that the wrist capsule behaves differently and that it is easier to immobilize the wrist and allow adequate healing.
In Geissler grade 1 and 2 SL instability, Danoff et al. in a small series have used arthroscopic thermal capsular shrinkage [37]. Using the fact that collagen shrinks with heat, nonablative thermal energy was also applied to the palmar SLIL in predynamic instability to effectively tighten up the ligament. Seven of eight patients had improved pain and preserved mobility, one patient failed this treatment and progressed to fusion.
Darlis et al. performed arthroscopic debridement and capsular shrinkage on 16 patients with 14 reported good to excellent results (8 of those pain free) and 2 failures [38]. Similarly, Hirsh et al. reported on a cohort of ten patients with 90 % pain free at an average follow-up of 28 months [39]. In contrast, Geissler reported on his findings in the management of 19 patients with chronic partial tears of the SLL (Geissler Grade II or III) or LT tears [36]. He reported variable results from poor to excellent using the Mayo wrist score at 6–22 months post-operation. Grade II tears appeared to have better results than Grade III injuries. However, as these are preliminary studies with small samples, no firm conclusions can be drawn.
Arthroscopic Suture Capsulorrhaphy, Capsulodesis, or Partial Repair
In the circumstance where complex open reconstruction is considered undesirable then arthroscopic reconstruction of chronic tears may be considered.
Mathoulin et al. describe an arthroscopic dorsal capsule-ligamentous repair for chronic reducible SL ligament tears [40, 41]. The technique involves passing a 3/0 PDS suture through a needle visualized arthroscopically and passed into the remnants of ligament and capsule between the scaphoid and lunate at the distal capsular reflection of the SLL and then tied to form a capsuloplasty. In his series of 36 patients with a mean 13-month follow-up, the results of the technique were generally excellent. The main advantage of the technique appeared to be the reduction in postoperative stiffness related to minimizing the dorsal capsular dissection needed during conventional surgical exposure with open techniques and hence the minimizing of scar tissue. Patient’s pain scores were generally excellent, they regained 96 % grip strength compared to the contralateral side and seven of the sports persons were able to return to the same level of sport postoperatively.
Del Pinal et al. [42] describe an all inside technique for arthroscopic suturing of the volar SL ligament. This technique used sutures introduced volarly via a Tuohy needle to plicate the volar ligament remnants and the long radiolunate ligament. Although this appears a favorable procedure, the technique had been applied to four patients with minimal follow-up reported, hence no meaningful conclusions for this technique can be made.
Recently, van Kampen and Moran reported on a new technique of a volar capsulodesis used to reconstruct the volar SLL using a portion of the long radiolunate ligament [43]. Although only results from a preliminary cadaveric study are published, they found that this approach allowed a strong repair with no compromise to the vascularity of the scaphoid or lunate.
Open Capsulodesis
Blatt’s original description [33] in 1987 used a dorsal radial flap of wrist capsule to differentially restrict scaphoid flexion. He left the flap of capsule attached to the radius and advanced it dorsally on the scaphoid. In his original series of 12 patients of late rotatory subluxation, he reported excellent recovery of range of movement, average grip strength recovered to 80 % and the majority returning to the preinjury work. Later Muermans and colleagues reported on 17 cases (11 cases of preradiographic instability; 3 dynamic; 3 static) with an average age of 30 years [44]. Patients had previously undergone conservative management and were on average 23 months post injury at the time of surgery. On blinded examination, they reported ten patients with excellent to good outcomes (pain and ADL) and six had fair to poor results. Sixteen patients had a negative Watson test. However, X-rays failed to reveal any significant improvement in SL gap or angle.
The reverse Blatt procedure leaves the capsule attached to the scaphoid and advances it proximally on the dorsal radius. It has been employed as an adjunct to various other open repairs and reconstructions [32]. Megerle et al. followed up 59 patients for an average of 8 years following dorsal capsulodesis [45]. A Berger flap was performed and a slip of the proximal aspect of the dorsal intercarpal ligament left attached distally onto the scaphoid and either sutured to the lunate (36 untethered cases) or distal radius (16 tethered cases) periosteum or attached with an anchor. K-wires were used to transfix the reduced SL interval while the capsulodesis healed. The k-wires were removed at 12 weeks. Carpal reduction was not maintained over time and 78 % went on to have radiographic evidence of Arthritis and an average SL angle of 70°.
Reconstruction
We have defined this as an attempt to reestablish a soft tissue connection between scaphoid and lunate that may be augmented by other secondary stabilizing soft tissues to provide additional stability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








