Table 56.1
Classification system according to Clatworthy and Gross
Type | Severity of bone deficiency | Treatment/restoration of joint line |
|---|---|---|
I | Contained with intact metaphyseal bone | No bone grafting or augmentation |
II | Contained with metaphyseal damage | Bone grafting, cement fill, or augments |
III | Uncontained, noncircumferential defect | Partial distal femur/proximal tibia or femoral head structural allograft |
IV | Uncontained, circumferential defect | Segmental distal femoral/proximal tibial graft |
56.2 Treatment
The management of bone loss in revision TKR depends on location, type, and extent of bony deficiencies as well as on the patient’s age and expectation for further future revisions. Treatment strategies for bone defects include cement filling, bone grafting, augmentation, and custom-made or hinged implants.
Treatment strategies for bone defects include cement filling, bone grafting, augmentation using cones, wedges or sleeves, and custom-made or hinged implants.
Cement filling provides inferior biomechanical properties in terms of load transfer and stability [7]. For the reduction of potential shear forces and the enlargement of bone-cement contact, the step-cut technique should be performed as shown in Fig. 56.2. Tibial resection should not include the entire bone surface down to the level of the bony defect, and attention should be paid to Gerdy’s tubercule (Fig. 56.3). Isolated cement filling should be restricted to contained or uncontained AORI Type 1 defects of less than 5 mm [8–11].
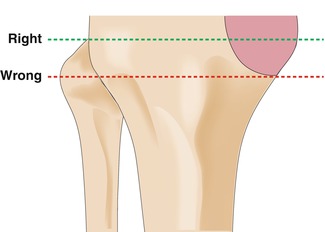
Fig. 56.2
Step-cut technique for tibial resection
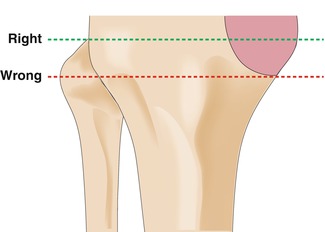
Fig. 56.3
Deep tibial resection
Isolated cement filling should be restricted to contained or uncontained AORI Type 1 defects of less than 5 mm.
Bone grafting can be performed using autografts or allografts, in either morselized or structural forms. Allografts provide inferior osteoinduction properties and bear the risk for viral, bacterial, and prion diseases. Therefore, autografts should be preferred in case of availability. Periprosthetic infections, neuropathic arthropathies, metabolic bone disorders, immunosuppression, and local radiation necrosis represent contraindications for the use of allografts [12]. Morselized bone grafting could be used for contained defects larger than 10 mm [13] and uncontained AORI Type 1 to Type 3 deficiencies in terms of “impaction grafting”.
Morselized bone grafting could be used for contained defects larger than 10 mm and uncontained AORI Type 1 to Type 3 deficiencies in terms of “impaction grafting”. Structural allografts are applied in uncontained AORI Type 2 and Type 3 bone defects larger than 15 mm.
The technique for tibial and femoral impaction grafting is shown in Figs. 56.4 and 56.5. A midterm implant survivorship of 85–98 % has been reported in revision TKR using morselized bone grafting [14–16]. Structural allografts are applied in uncontained AORI Type 2 and Type 3 bone defects larger than 15 mm [13]. Midterm results show a survival rate of 79–92 % at almost 5 years and 72 % at 10 years [17–20].
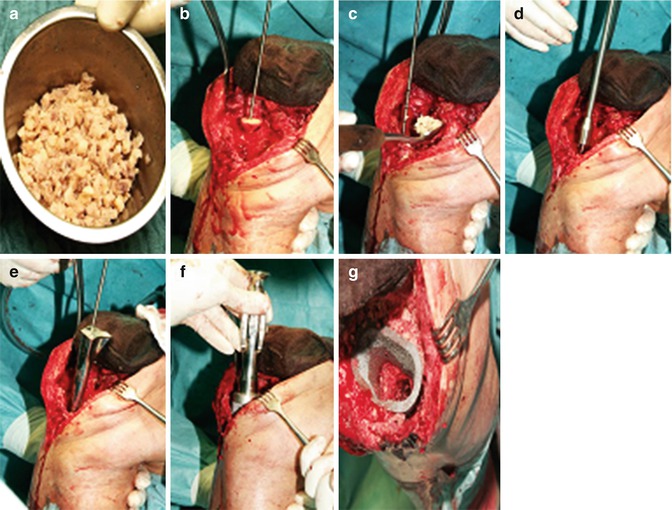
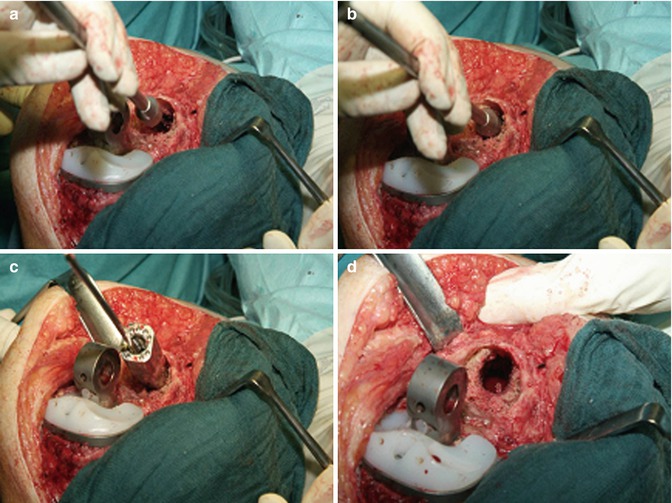
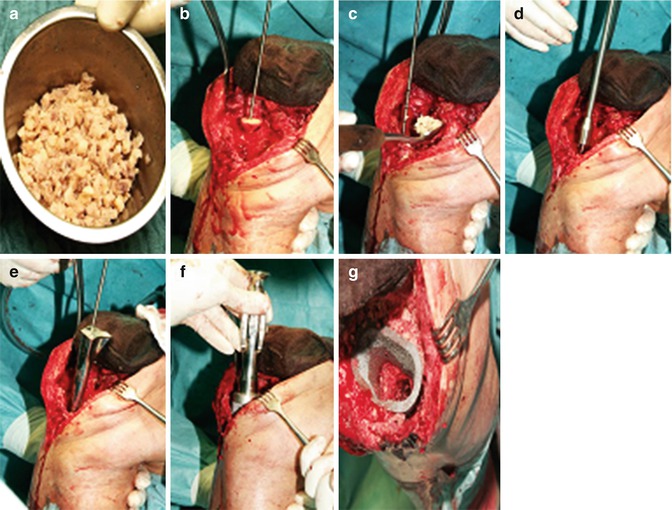
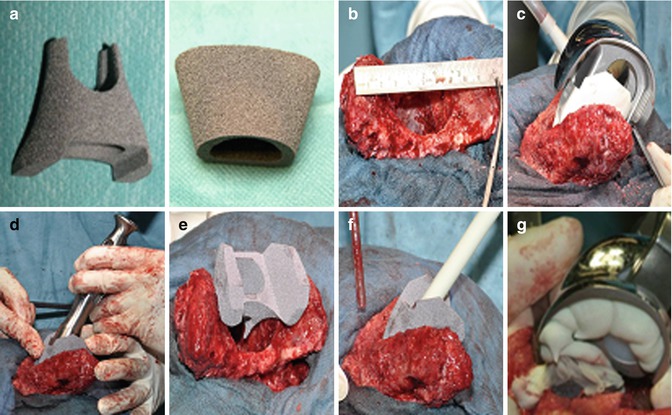
Fig. 56.4
Tibial impaction grafting. (a) Morselized allograft. (b) Insertion of structural allograft (cement barrier) with central liner. (c) Insertion of morselized allograft. (d, e) Stepwise impaction of morselized allograft with central stem and dummy. (f) Implantation of metaphyseal tantalum cone. (g) Impacted allograft plus tantalum cone
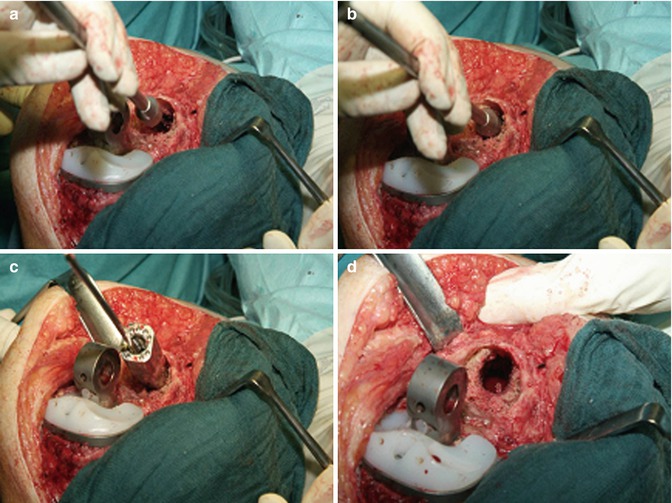
Fig. 56.5
Femoral impaction grafting. (a, b) Impaction of morselized allograft with central stem. (c) Central liner plus dummy. (d) Impacted allograft
For uncontained AORI Type 2 bone defects (5–15 mm and >50 % femoral or tibial plateau), the use of prosthetic augments with supplemental stems is recommended [13].
For uncontained AORI Type 2 bone defects (5–15 mm and >50 % femoral or tibial plateau), the use of prosthetic augments with supplemental stems is recommended.
Fretting corrosion, further bone resection for the augment’s accommodation, potential cement augmentation or bone grafting, as well as additional shear and compression forces in case of angled or step wedge augments represent disadvantages of these devices. Despite short- and midterm implant survival rates of 92–100 % [21–25], Hockman et al. described a revision rate of 42.9 % 5 years after wedge augmentation without additional structural allografting [26]. Porous tantalum as a metaphyseal filling implant mimics bony characteristics by combining high strength and low stiffness. Femoral and tibial tantalum cones as well as the implantation technique are presented in Fig. 56.6. Furthermore, it provides corrosion resistance and high porosity allowing bone ingrowth. Therefore, porous tantalum could be used in severe bone loss as an alternative to structural allografts. The lack of bone stock restoration and the required cement fixation to the prosthesis represent potential disadvantages. Short-term outcome revealed 100 % implant survival and osseous integration of porous tantalum [27–29]. Mid- and long-term results of these devices have to be clarified in further studies. A treatment algorithm for the management of bone loss in revision TKR is shown in Fig. 56.7.