Specific injuries encountered
It is surprisingly difficult to locate summary data on the incidences of specific injuries in sport. Apart from the epidemiological challenges previously outlined, there are some practical reasons for this. Countless articles offer reports about injuries in certain sports, but assessing these systematically is a monstrous task. In addition, the types of injuries sustained by children, adolescents, young adults, middle-aged adults and senior adults likely differ, as do injuries encountered in recreational sport, competitive sport and sport training. Combine these diversities with the variety in sports, rules, equipment, venues, training regimens and healthcare access across the globe and the task of assessing sport injury epidemiology appears overwhelming at best. The USA’s National Collegiate Athletic Association maintains excellent data for university athletes that offer some insight into those body regions that are most affected and those injuries that occur most commonly in certain sports (Hootman et al. 2007). Selected data are provided in Tables 10.2 and 10.3.
Table 10.2 Injury incidence by body region for university athletes from 1988 through 2004 (Hootman et al. 2007)
| Percent of all injuries | ||
| Body region | Matches | Training |
| Lower extremity | 53.8 | 53.7 |
| Upper extremity | 18.3 | 21.4 |
| Trunk/back | 13.2 | 10.0 |
| Head/neck | 9.8 | 12.8 |
| Other | 4.9 | 2.2 |
Table 10.3 Incidence of common injuries in university athletes, by sport, from 1988 through 2004 (Hootman et al. 2007)
Initial assessment of acute sport injury
Assessment of all injuries in sport participants should follow the standard history, inspection (observation), palpation, and special testing paradigm commonly applied by healthcare professionals. These steps can be summarised as follows (for greater detail read Chapter 11:Musculoskeletal Assessment).
History
This first step in injury evaluation is fundamental to success. It entails a series of questions directed to the athlete that are designed to elicit the factors surrounding the injury and any corollary findings (such as previous history of injury) that may be important in arriving at a diagnosis. The exact questions are modified depending on the situation, but some sample queries for athletes with acute injuries are given below.
- When did this happen?
- What were you doing at the time of the injury?
- How did the injury occur?
- Did you hear or feel a pop, crack, snap, or other unusual sensation?
- Have you injured this area previously?
- How does it feel now compared to when the injury first occurred?
- How is the injury limiting your activity?
Inspection (observation)
This step requires a careful visual analysis of the injured area and adjacent regions. Several pieces of information are collected before the examiner touches the injured area. The contralateral limb should be used for comparison as long as it does not exhibit atypical characteristics because of a prior injury or other reason. Examples of observational information to gather about the type and extent of injury include:
- Deformity (e.g. joint incongruity, limb angulations, anatomical landmark displacement)
- Swelling
- Discolouration (e.g. pallor, ecchymosis, erythaema)
- Gait discrepancies or difficulties
- Difficulties climbing to the examination couch
- Reduction in joint range of motion.
Palpation
This is the first instance when the examiner actually touches the injured athlete. A systematic probing of the injured area and surrounding tissues gain important details and may help the clinician identify pathologies that accompany the primary injury. Once again the contralateral limb is used as a reference. Examples of findings from effective palpation include:
- Localisation of pain and tenderness (including deciding which structures are painful and which are not as part of a differential diagnostic process)
- Atypical anatomical contours
- Crepitus
- Effusion and oedema.
Special testing
Following completion of the history, inspection and palpation steps the examiner conducts a series of assessments to gather further insight into the nature and severity of the injury. These vary widely depending on the body region being evaluated and the diagnostic clues gained in the first portion of the examination. (Magee (2008) provides an excellent and comprehensive handbook of musculoskeletal examination that the sport rehabilitator will find invaluable as a reference in addition to the present text.) They may include manual tests performed by the examiner to identify joint instability or certain functional activities that the examiner asks the athlete to perform. The results of this analysis add to the diagnostic process and help broaden the information on which clinical decision making is based.
Once again, testing the contralateral extremity is important as a comparison. However, there are three important caveats for the examiner. First, the uninjured limb should be tested before the injured one in order to familiarise the athlete with the evaluation procedures and to allay their apprehensions. If the athlete cannot relax, muscle guarding will compromise the testing. Second, a previously injured contralateral joint may not be a suitable “normal” standard against which to judge the currently injured joint. Third, a systematic method for evaluating each region of the body is most effective and efficient for completing the examination process without missing important diagnostic details.
Serving as one common example that will be encountered by virtually all sport rehabilitators, the evaluation of an acute knee injury includes special tests such as:
- Apprehension sign for patellar dislocation/ subluxation
- Lachman’s test for anterior cruciate ligament integrity
- Anterior drawer test for anterior cruciate ligament integrity
- Posterior gravity sign for posterior cruciate ligament integrity
- Pivot shift test for anterolateral rotary instability
- McMurray’s test for meniscal damage
- Apley’s grind test for meniscal damage
- Ottawa Knee Rules (Stiell et al. 1995, 1996; Tigges et al. 1999) to rule out fracture.
Assessment case study: ankle sprain
One of the most common injuries in sport is ankle sprain (Garrick 1977; Yeung et al. 1994; Fong et al. 2007; Hootman et al, 2007), so it will serve as an example of how acute injury evaluation is applied. The sport rehabilitator confronted with this type of ankle injury will assign a severity grade to the sprain based on the results of the clinical examination (see Table 10.4). A partially torn ligament – categorised as a grade 2 sprain – can encompass a wide range of damage, whilst a grade 3 sprain is a complete rupture of a ligament. The determination by the examiner of a limit – or an endpoint – to their stress exam of the joint is important. The endpoint is created by any remaining intact ligament restricting the movement. A grade 3 sprain does not exhibit such a limit; rather, an indistinct, soft endpoint is present because the torn ligament cannot oppose the stress the examiner places on the ankle.
Table 10.4 Summary of ligament injury severity grading
However, the examiner must remember that many subjective subtleties exist in evaluating ligament damage because there are virtually infinite ways that ligaments supporting a joint can be injured. The amount of joint instability may be graded instead of the degree of injury to a specific ligament (Hildebrand et al., 2007). For instance, a grade 2 instability may be present when one ligament is completely torn and the others around a joint are not. But, partial tears to two or more ligaments about the joint may also result in the same type of instability. This underscores the need for the sport rehabilitator to practise a systematic method of ligament injury evaluation.
The following section outlines the stages of injury assessment carried out by a sport rehabilitator. An injured basketball player presents to the sport injury clinic to be evaluated by a member of staff. He is wearing shorts and walks with a limp. He climbs onto the examination couch and the sport rehabilitator begins the assessment.
Acute ankle injury: history
There are certain customary questions to ask an injured athlete, and some of these depend on the body region involved. A framework of “What, When, Where, How?” may be helpful. It is ideal to develop a routine examination methodology in order to facilitate the process and ensure one does not miss important diagnostic clues.
Examiner: What happened to your ankle?
Player: I jumped up for a rebound and when I came down, my foot landed on top of Ian’s and it rolled over.
Examiner: When did this occur?
Player: Yesterday afternoon during training.
Examiner: What did you feel when it happened?
Player: It hurt a lot, and I felt it pop.
Examiner: Has it been painful since the injury occurred?
Player: It hurt loads when it happened, but I just walked it off. Later it felt better and I’ve been able to carry on with life OK.
Examiner: How does it feel now?
Player: It still hurts, but not as much.
Examiner: Have you ever hurt this ankle before?
Player: No.
Examiner: How about the other one?
Player: No, not at all.
Examiner: OK, I’m going to examine it now.
Acute ankle injury: inspection
At this point the examiner looks carefully at both the injured and uninjured ankles to assess swelling, ecchymosis (bluish discolouration), and other visible signs that may add information to the assessment. The athlete’s ankle exhibits an area of swelling anterior to the lateral malleolus that is approximately the size of a table tennis ball.
Examiner: Where would you say it hurts the most? Can you place one finger at that spot?
The player points to a location about 1.5 cm anterior to the lateral malleolus; this is an area over the anterior talofibular ligament and the spot where the swelling is located. There are no other areas of swelling nor are there other outward signs of injury.
Examiner: Can you show me the way your ankle and foot turned when you landed on Ian’s foot?
The player demonstrates an inversion movement of the foot with slight plantar flexion.
Acute ankle injury: palpation
First the examiner palpates the uninjured extremity in order, again, to familiarise the player with the process and to reduce his apprehension. Then the examiner begins to gently palpate various places about the foot, ankle and leg of the player’s injured limb, starting with areas that are not likely to be painful in order to keep the player at ease. It is crucial that the clinician be well versed in clinical anatomy for this portion of the injury examination. Locations and structures the examiner palpates are:
- Ligaments (to investigate possible sprains)
- deltoid ligament
- anterior talofibular ligament
- calcaneofibular ligament
- anterior tibiofibular ligament
- calcaneocuboid ligament
- deltoid ligament
- Bones (to investigate the possibility of associated fractures)
- base of the 5th metatarsal, to assess an avulsion fracture
- metaphysis and diaphysis of the 5th metatarsal, to assess a shaft fracture or Jones (proximal diaphyseal/metaphyseal) fracture
- lateral malleolus
- fibula, extending up the leg to the fibular neck in order to assess a Maisonneuve fracture
- dorsal talus
- navicular
- calcaneus
- base of the 5th metatarsal, to assess an avulsion fracture
- Tendons and muscles (to investigate possible strains)
- Achilles tendon
- peroneal tendons, extending up the leg to their muscles
- tibialis anterior tendon
- tibialis posterior tendon.
- Achilles tendon
The examiner does not note any pain or crepitus on bony structures, so the suspicion for fracture is low. Palpating the soft tissue structures does not elicit pain except for the anterior talofibular ligament; this is accompanied by a sensation of ballottement as the examiner presses over the swollen tissue.
Acute ankle injury: special testing
Now the examiner proceeds to the final phase of the injury evaluation. Once again, the contralateral side receives attention first; the player reported no history of injury to this side so it will serve as “normal” for comparison purposes. The following tests are performed there and then repeated on the injured limb. (For more specific detail regarding special testing for the ankle please see Chapter 22)
- Eversion (varus) stress test to evaluate the deltoid ligament
- Forcing the foot into dorsiflexion to evaluate the anterior tibiofibular ligament (this forces slight separation of the tibiofibular syndesmosis)
- Twisting the foot in the ankle mortise to evaluate the anterior tibiofibular ligament (this also separates the syndesmosis)
- Inversion (valgus) stress test in anatomical position (ankle neutral) to evaluate the calcaneofibular ligament
- Inversion stress test in plantar flexion to evaluate the anterior talofibular ligament
- Anterior drawer test with the ankle in neutral position to evaluate the anterior talofibular ligament.
The examiner must be careful to not fall into the trap of finalising an injury diagnosis without gathering all potentially useful information with a thorough history, inspection, palpation and special testing protocol. Many inexperienced clinicians have been distracted from a proper diagnostic conclusion because they did not assess an injury carefully enough. That being said, however, there are certainly natural tendencies that are anticipated when the mechanism of an injury is known. In the case of our basketball player here, we are aware that he inverted and plantar flexed his ankle when he landed on another player’s foot. This mechanism is very typical of an anterior talofibular ligament sprain (Garrick 1977), but completing the battery of tests listed above will help identify other potentially injured structures.
Our basketball player exhibits the following results of ligament testing:
- Eversion stress: not painful and no instability (firm endpoint) compared to contralateral
- Impression: deltoid ligament intact
- Forced dorsiflexion: no pain elicited
- Impression: anterior tibiofibular ligament intact
- Twisting foot in the mortise: no pain elicited
- Impression: anterior tibiofibular ligament intact
- Inversion stress test in anatomical position: very slightly painful anterior to the lateral malleolus at end of range and no instability compared to contralateral
- Impression: calcaneofibular ligament intact; based on its location, the mild pain is likely emanating from the anterior talofibular ligament
- Inversion stress test in plantar flexion: moderate pain that worsens at end of range of movement and questionable slight instability compared to contralateral
- Impression: grade 1 or 2 anterior talofibular ligament sprain
- Anterior drawer test: moderate pain that worsens at end of range of movement and slight instability compared to contralateral
- Impression: grade 2 anterior talofibular ligament sprain.
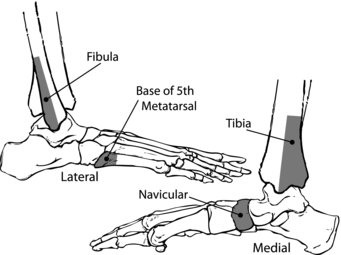
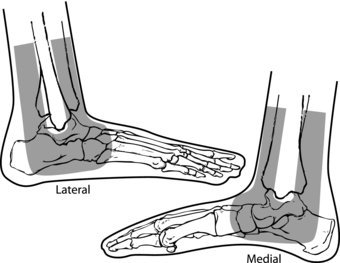
Parenthetically, as part of an acute ankle assessment the Ottawa Ankle Rules (Stiell et al. 1992, 1994) should be applied. These rules (Table 10.5 and Figure 10.1) have greatly reduced the unnecessary X-rays previously associated with ankle injury management in the A&E department and other healthcare settings (Milne 1996; Leddy et al., 1998; Bachmann et al., 2003; Nugent 2004). The rules provide guidance for clinical personnel in determining when ankle injuries require radiography for suspected fracture, and they are appropriate and effective for sport medicine settings (Leddy et al., 1998; Papacostas et al., 2001; Leddy et al., 2002). Implementing the rules for sport ankle injuries prevented missed fractures, decreased X-ray exposure, saved unnecessary healthcare expenditures and fostered patient satisfaction (Leddy et al., 2002). The Ottawa Ankle Rules appear to be most useful when applied by healthcare workers, as patients may not be able to apply them accurately to their own ankle injuries (Blackham et al., 2008). Sport rehabilitators and other allied health professionals should familiarise themselves with these important adjuncts to ankle injury evaluation.
Table 10.5 Ottawa Ankle Rules (see Figure 10.1 also) (Stiell et al. 1992, 1994; Leddy et al., 2002; Nugent 2004)
Figure 10.1 Pictorial representation of the Ottawa Ankle Rules showing the locations – the shaded areas – where bony tenderness indicates the advisability of obtaining ankle X-rays. Reproduced, with permission, from Figure 1 from Russell, J.A., ‘Acute Ankle Sprain in Dancers’ Journal of Dance Medicine and Science, 14, 2010 © J. Michael Ryan Publishing, Inc.
Acute ankle injury: information collating and decision making
After executing the history, inspection, palpation and special testing steps, the sport rehabilitator arrives at the clinical impression of a grade 2 sprain of the anterior talofibular ligament. Following is a summary of the examination details that led to this decision.
- Mechanism of injury: inversion with plantar flexion, a movement that places the anterior talofibular ligament under tension
- Location of swelling and pain: anterior to the lateral malleolus, which is the anatomical location of the anterior talofibular ligament
- Pain and slight laxity in the ankle: occurs during inversion and plantar flexion testing that place tension on the injured ligament, suggesting that a portion of the ligament is disrupted; note that in this case there is an equivocal impression when considering only the inversion exam with plantar flexion – the anterior drawer test result adds clinical information
- Associated fracture likelihood: not likely, as the player arrived at the clinic with full weight bearing ambulation and palpation of the bony structures did not reveal pain; thus, the Ottawa Ankle Rules suggest no fracture.
Certainly injury examination is very subjective, although a systematic evaluation scheme helps reduce variability in the assessment process. Nonetheless, there is no substitute for the experience of examining as many injuries as possible in order to gain the ability to discern subtleties present in the wide variety of cases. Both proper clinical education and clinical experience are essential for effective injury care.
First aid and initial therapeutic measures
The acronym PRICE is the standard for acute care of sport injury. This is a reminder of five steps: application of Protection, Rest, Ice, Compression and Elevation (Flegel 2008). An alternative, RICES – Rest, Ice, Compression, Elevation, Stabilisation – has been proposed (Knight 2008; Knight and Draper 2008), but portrays the same basic meaning. The generally accepted period for the acute treatment described below is the first 48–72 hours after the injury. Knight (2008) suggests for clarity’s sake that acute care be subdivided into three phases: emergency (encompassing CPR or urgent transport to A&E), immediate (from time of injury to 12 hours post-injury) and transition care (from 12 hours to 4 days post-injury). No matter how the initial period of time following an injury is apportioned, the success of follow-up treatment depends substantially on the initial treatment that is applied.
Protection by bracing, splinting, or non-weight bearing transport of an injured athlete is undertaken when necessary to minimise the risk of further trauma to an injured area. Proper first aid techniques at this initial stage are crucial to the athlete’s well-being. Rest from the activity that caused the injury, or similar activities, is warranted when the opportunity exists for reinjury or further injury.
In the last several years, the “gold standard” of cold – or cryotherapy – as an injury treatment has been analysed for its efficacy in evidence-based practice (Ernst and Fialka 1994; Lessard et al. 1997; Bleakley et al. 2004; Hubbard and Denegar 2004; Collins 2008). In spite of questions raised about the therapeutic effects of cold treatment, it is helpful for pain reduction (Hubbard and Denegar 2004; Algafly and George 2007). Other reasons for applying cold to acute sport injuries include minimising oedema and effusion (Merrick 2007) and controlling secondary cellular hypoxia (Dale et al., 2004) and the broader secondary metabolic injury (Merrick et al. 1999; Knight and Draper 2008) in the injured region. Whilst cold slows oedema formation, it does not reduce oedema that is already present (Knight and Draper 2008).
A typical application of therapeutic cold should last no longer than 20 minutes (Bleakley et al. 2006; Flegel 2008); approximately one hour should elapse before another cold treatment in order to allow the tissue to rewarm. As with all treatment procedures there are important caveats. More body tissue heat is given off (resulting in lower tissue temperature) to a 10° cold pack than to a 20° cold pack (Knight and Draper 2008) and by body regions with a thinner insulating fat layer (Otte et al. 2002) or a larger surface area covered by the treatment modality (Knight and Draper 2008). Therefore, longer treatment times or more intense forms of treatment further increase heat loss and can instigate tissue damage (Knight 1995; Knight and Draper 2008). Moreover, research suggests that muscular power and functional performance are reduced even after a 10 minute ice application (Fischer et al. 2009).
Circumferential compression in an injured extremity enhances control of oedema by increasing the external tissue pressure to promote lymphatic drainage in the region of the injury and by assisting venous return (Wilkerson 1991; Wilkerson and Horn-Kingery 1993; Delis et al. 2000; Mora et al. 2002; Vanscheidt et al. 2009). Application of an elastic or crepe bandage provides some compression and a general reassurance to the athlete, although a pneumatic stirrup-type of brace has been shown to be more effective in treating ankle sprains (Boyce et al. 2005). Intermittently applied compression may be beneficial, as well, especially when applied in conjunction with cryotherapy (Starkey 1976; Quillen and Rouillier 1982; Mora et al. 2002). Research in this area related to patients with chronic oedematous pathology is instructive (Delis et al. 2000; Vanscheidt et al. 2009) as significant improvements in swelling have been shown and a dose-response relationship has been reported (Vanscheidt et al. 2009).
Of concern in the common sport injury of ankle sprain are the contours of the medial and lateral malleoli. This topology about the ankle may prevent the areas anterior and posterior to the malleoli from receiving adequate compression by an elastic or crepe bandage. This is because the bandage bridges across from the anterior and posterior ankle surfaces to the malleoli, thus leaving the spaces adjacent to the malleoli without sufficient external pressure. Horseshoe shaped pads cut from 1 cm (3/8 inch) foam or chiropody felt and positioned underneath the bandage during wrapping – as shown in Figure 10.2 – may improve elimination of oedema in these areas (Wilkerson and Horn-Kingery 1993; Merrick 2004).
Figure 10.2 The shaded areas denote the shape and location for placement of a foam or chiropody felt horseshoe pad as a compressive element in treating acute ankle sprain. Reproduced, with permission, from Figure 1 from Russell, J.A., ‘Acute Ankle Sprain in Dancers’ Journal of Dance Medicine and Science, 14, 2010 © J. Michael Ryan Publishing, Inc.
Elevation of the injured extremity so the ankle is positioned above the level of the heart is another technique that promotes a decrease in swelling (Rucinkski et al. 1991). Gravity assists venous return, as well as lymphatic drainage of fluid collected in the interstitial spaces (Dale et al. 2004). However, a return of the limb to the non-elevated, or gravity-dependent, position may reverse the oedema reduction gained by elevation (Tsang et al. 2003). Thus, elevation for as much time as possible is important during the period of acute injury management.
Pain management in acute musculoskeletal sport injury
A number of therapeutic modalities are available today for treatment of various aspects of sport injury. The presentation of these will be confined to those categorised as physical agents (Merrick 2007) or pharmacological agents that are designed to control pain in the acute stage of injury. It is important in applying any type of modality to a patient or client that the clinician has an appropriate aim for such application as well as an understanding about the physiology of the modality and its effects on the body.
Physical agents
The two traditional physical agents best suited to successful management of acute injury pain are cryotherapy and electrotherapy (Merrick 2004). There are many methods of cryotherapy (Swenson et al. 1996; Bleakley, et al. 2004), though not all are equivalent in their efficacy (Bleakley et al. 2004). As previously mentioned, cold treatment is effective for ameliorating pain among other therapeutic effects like slowing development of haematoma and oedema, decreasing nerve conduction velocity, reducing muscle spasm (Swenson et al. 1996), reducing local blood flow in the injured area (Knight and Londeree 1980) and minimising secondary metabolic injury (Merrick et al. 1999; Knight and Draper 2008).
In terms of method of application, it is somewhat difficult to make a recommendation because techniques and published findings are so varied (Bleakley et al. 2004, 2007). A simple ice bag is usually the most expeditious and inexpensive means of applying cold. It has many proponents (McMaster et al. 1978; Merrick 2004; Bleakley, et al. 2006; Knight and Draper 2008), although it has been shown that a 20 minute cold whirlpool bath procured a longer tissue temperature reduction than did a 20 minute crushed ice pack treatment for the leg (Myrer et al. 1998). A protocol of a 10 minute ice pack application, 10 minutes without ice and then another 10 minutes of ice pack lowered tissue temperature better than a single 20 minute ice pack treatment (Bleakley et al. 2006). The effective cooling by ice is related to the phase change that it undergoes from a solid to a liquid as it melts (Merrick et al. 2003). The combination of therapeutic cold and exercise, or cryokinetics (Hayden 1964; Knight 1995; Bleakley et al. 2007; Knight and Draper 2008), is especially beneficial because of the way early motion promotes subsequent rehabilitation. In this technique pain is managed by the cold treatment and then the athlete undertakes a controlled exercise regimen, followed by another cycle of cold.
Transcutaneous electrical nerve stimulation (TENS) is an electrotherapy modality shown to be effective for musculoskeletal pain (Hsueh et al. 1997; Bertalanffy et al. 2005). It electrically stimulates sensory nerves around an injured body region to interfere with pain stimuli. The gate control theory (Melzack and Wall 1965; Dickenson 2002) defines how high-frequency TENS mediates the sensation of pain. Pain impulses on α-δ and C nerve fibres in the spinal cord are interrupted by sensory information transmitted via α-β afferent nerves (Merrick 2004). Thus, if the TENS signal stimulates the α-β fibres to a great enough degree, those nerve signals will close a “gate” in the spinal cord for the pain stimuli and be perceived instead of the pain.
Although it has been applied to acute musculoskeletal pain scenarios, systematic review of the research is inconclusive about the efficacy of TENS (Walsh et al. 2009), and a lack of randomisation in clinical trials leads to over-estimation of the positive effects of the treatment (Carroll et al. 1996). In acute low back pain patients, therapeutic exercise with TENS was not assistive to patient recovery in comparison to exercise alone (Herman et al. 1994). Neither was it a benefit for patients with acute postoperative pain following lumbar surgery (McCallum et al. 1988). However, in a randomised, double-blind study of trauma patients at A&E TENS was as effective as oral medication for analgesia (Ordog 1987). There are several different TENS units on the market, a myriad of musculoskeletal injuries and numerous protocols with which TENS can be applied to these injuries. Discussing all of these variations is beyond the scope of this chapter; but, because TENS is a relatively safe modality, there is minimal risk to utilising it for management of acute pain in sport injuries and discontinuing it if it proves ineffective for a given athlete.
High-voltage, low-frequency electrical stimulation also can be useful for managing acute pain (Merrick 2004). The intention for this modality is to elicit release of an opioid substance called beta-endorphin that naturally occurs in the body (Hughes et al. 1984; Bender et al. 2007); beta-endorphin is a powerful mediator of pain (Bender et al. 2007). The treatment may be somewhat uncomfortable to the patient because of the waveform and frequency, but this stimulation is what makes the technique effective in bringing forth release of beta-endorphin and consequent pain relief after treatment (Merrick 2004).
A final type of electrotherapy that often is effective for acute pain management is interferential current (Merrick 2004; Jorge et al. 2006). This technique’s name is derived from its two electromagnetic fields that cross each other; at their point of intersection is a localised field of interference caused by their competing current phases. The current in this field continually changes, a property that precludes accommodation by the nerves in the treatment area and which yields analgesia via the gate control mechanism (Merrick 2004). Whilst interferential current has been shown to be similarly effective compared to TENS, research about it is scant (Johnson and Tabasam 2003). Certainly its usage is confined to a clinical setting, perhaps making TENS preferable simply because of easier device portability and the ability of patients to operate the equipment.
Pharmacological agents
Topical analgesics
Topical methods of analgesia are enjoying renewed interest in healthcare because of the challenges inherent with administering pain medications via other routes (Stanos 2007). Among the non-prescription compounds available, counterirritants are one of the oldest and most widely used. They are marketed under such brand names as Sports Muscle Rub, Muellergesic, BioFreeze, Tiger Balm and Deep Heat Cream. These preparations contain capsaicin, menthol, camphor, garlic and other ingredients that possess both distinct aromatic properties and an ability to act on the nociceptors of the skin. Their characteristic “counterirritation” reduces the perception of the musculoskeletal pain “irritation.”
NSAID topical ointments, especially those containing ibuprofen or diclofenac, show promise as satisfactory alternatives to oral NSAIDs. A double-blind study of the effects of oral versus topical gel ibuprofen reported no difference between the two delivery methods for all therapeutic measures (Whitefield et al. 2002). Other studies corroborate the efficacy of topical NSAIDs (Dominkus et al. 1996; Rovenský et al. 2001; Banning 2008); but, this depends on the relative depth (e.g. superficial versus intra-articular) of the pain’s origin (Dominkus et al. 1996; Miyatake et al. 2009).
Over-the-counter oral analgesics
Paracetamol (acetominophen) is the most widely used analgesic compound in the world (Jalan et al. 2007). It is generally thought to be a safe and effective medication (Graham et al. 2003; Kehlet and Werner 2003), although some concern exists that liver toxicity is possible even at commonly used non-prescription doses (Jalan et al. 2007). Paracetamol also has been shown to be as efficacious in acute musculoskeletal pain as non-steroidal anti-inflammatory drugs (Woo et al. 2005; Gøtzsche 2006). Nonetheless the drug is not without side-effects and controversy (Moynihan 2002; Ahmad 2007); and, assuredly it must not be offered nor ingested indiscriminately. The sport rehabilitator has a role and responsibility in properly advising athletes, patients and clients in the approved use of this and other medicinal preparations.
Compared to Paracetamol, NSAIDs are much more likely to elicit unfavourable reactions. They are well known for adversely affecting the gastrointestinal system (McCarthy 2001), and more recent evidence has associated adverse cardiovascular effects with cyclo-oxygenase 2 (COX-2) inhibitor NSAIDs (Jüni et al. 2004; Vardeny and Solomon 2008). Assessing the risks and benefits of this class of pharmaceuticals can be complex (Patrono and Rocca 2009). As mentioned above, some studies suggest that for typical pain from acute musculoskeletal injury, NSAIDs and Paracetamol are similarly effective. Unquestionably, administration of prescription NSAIDs or over-the-counter NSAIDs (e.g. ibuprofen) at prescription strength doses is unethical without the care of a GP or consultant. The sport rehabilitator must adhere to approved applications of NSAIDs and discourage improper NSAID use when advising individuals under their care.
Concussion
An understanding of concussion as an acute injury is crucial to the sport rehabilitator. Whilst it is not the typical musculoskeletal injury, it can be considerably more serious and troublesome to manage. Concussion is defined as “a trauma-induced alteration in mental status that may or may not involve loss of consciousness” (American Academy of Neurology 1997, p. 582). It has gained increasing attention in recent years because – in addition to its trauma-induced metabolic compromise of the brain (Katayama et al. 1990; Giza and Hovda 2001) – insidious sequelae often are associated with it in the form of associated pathologies such as subdural hematoma (Kersey 1998; Mori et al. 2006) or post-concussion syndrome (Fazio et al. 2007; Yang et al. 2009).
Whilst the basic steps of acute injury evaluation presented earlier apply to concussion, this injury is being treated separately herein because of its importance and the special techniques necessary for successfully handling it. Several medical associations have published position papers outlining proper management of concussion (American Academy of Neurology 1997; Guskiewicz et al. 2004; American College of Sports Medicine 2006; McCrory et al., 2009) in order to help decrease the morbidity and mortality of this injury. The sport rehabilitator who attends pitchside must be well versed in management of concussion and related conditions as catastrophic injury can be more alarming and potentially deadly than most other situations that confront sport medicine workers.
Toth (2008) comprehensively reviewed the literature to identify neurological injury rates sustained in sport and recreation. Table 10.6 summarises his analysis. Collision sports (e.g. rugby, North American football), sports where the participants or projectiles move at high velocity (e.g. alpine skiing, motorsports, skateboarding, cricket, baseball, ice hockey) and pugilistic sports (e.g. boxing, martial arts) are particularly prone to injuries of the head and neck. Certainly protective headgear are helpful against direct blows in some sports, but they do not prevent all head injuries and concussion can occur with or without helmets (American College of Sports Medicine 2006). In football, headgear does not offer protection against ball contact head injuries, but it does appear to reduce the severity of head-to-head contact injuries (Withnall et al. 2005). Of particular consequence in sport-related brain injuries are rapid acceleration or deceleration of the head or high velocity angular head motion (Holbourn 1945; Ommaya and Gennarelli 1974). Concussions are usually graded 1 through 3 according to severity (American Academy of Neurology 1997; Randolph 2001), as outlined in Table 10.7.
Table 10.6 Neurological injuries to participants in a variety of sports (NA = not available) (adapted from Toth 2008)
| Sport | Acute neurological injury rate per 100 athlete-exposures | Incidence of mild traumatic brain injury per 1,000 athlete-exposures |
| Basketball, males 18–23 yrs | 1.0 | 0.3 |
| Basketball, males 22–39 yrs | 1.9–6.4 | NA |
| Basketball, females 18–23 yrs | 0.4 | 0.5 |
| Basketball, females 22–39 yrs | 2.5–6.7 | NA |
| Boxing, amateur | 14–20 | 11–77 |
| Boxing, professional | 21–45 | 186–251 |
| Cricket | <0.1 | <0.1 |
| Football, males 18–23 yrs | 18.8 | 1.1 |
| Football, males 22–35 yrs | 105 | NA |
| Football, females 18–23 yrs | 16.4 | 1.4 |
| Football, females 22–35 yrs | 109 | NA |
| Football, North American, 18–23 yrs | 1.5–4.0 | 2.3–6.1 |
| Hockey, males 17–23 yrs | 12.6 | 1.1 |
| Hockey, females 17–23 yrs | 7.9 | 0.5–0.7 |
| Ice hockey, males 18–23 yrs | 0.5 | 1.5–4.2 |
| Ice hockey, females 18–23 yrs | 1.3 | 2.7 |
| Ice hockey, males 20–36 yrs | 11.9 | 6.6 |
| Snowboarding | 0.4 | 6.1 |
| Taekwondo | 6.3 | NA |
| Wrestling, males 17–23 yrs | 7.3 | 1.3 |
Table 10.7 Characteristics of concussion grades (American Academy of Neurology 1997; Randolph 2001)
| Concussion grade | Identifying characteristics |
| 1 | Transient confusion No loss of consciousness Concussion symptoms or mental status abnormalities resolve in less than 15 minutes |
| 2 | Transient confusion No loss of consciousness Concussion symptoms or mental status abnormalities last more than 15 minutes |
| 3 | Any loss of consciousness |
Athletes who experience concussion can safely resume sport participation if the return to play decisions are carefully made by healthcare professionals using appropriate individualised clinical guidelines (Randolph 2001; Lovell et al. 2004; American College of Sports Medicine 2006; Alla et al. 2009; Makdissi et al. 2009). However, such evaluations are complex. Evidence suggests that athletes who sustain multiple concussions exhibit cumulative neurological effects (Collins et al. 2002; Iverson et al. 2004), experience a substantial reduction in memory ability (Iverson et al. 2004) and demonstrate several pitchside neurological examination abnormalities (Collins et al. 2002) when compared to athletes with no history of concussion. Moreover, return to participation prior to resolution of head injury symptoms heightens susceptibility to further concussive episodes, even if the subsequent trauma is relatively minor (Kersey 1998; Lovell et al. 2004; Mori et al. 2006).
Acute evaluation of concussion
Concussion is not an easy diagnosis in the sport environment. The precipitating event may be associated with neither direct head trauma nor loss of consciousness (Lovell et al. 2004). Players usually are anxious to return to the match/competition; thus, they may not report a head injury or they may attempt to evade examination in favour of resuming play. A wide variety of signs and symptoms must be assessed, many of which are presented in Tables 10.8 and 10.9. A consultant neurologist is invaluable in this instance, and conservative management is paramount at all times. When in doubt, exclude the athlete from participation until concussion is disproven or completely resolved because there is a risk of cumulative neurological deficits in athletes who sustain subsequent concussions, especially before resolution of the antecedent episode (Cantu 1988; McCrory and Berkovic 1998). Prudence indicates that the sport rehabilitator and other healthcare professionals maintain an emergency action plan that can be implemented as required when they are confronted with a head injured athlete. Consciousness, airway integrity, breathing and circulation are fundamental diagnostic signs to assess and act on.
Table 10.8 University of Pittsburgh’s signs and symptoms of concussion (Lovell et al. 2004)
| Signs observed by medical staff | Appears to be dazed or stunned Is confused about assignment Forgets plays Is unsure of game, score, or opponent Moves clumsily Answers questions slowly Loses consciousness Shows behaviour or personality change Forgets events prior to play (retrograde) Forgets events after hit (post-traumatic) |
| Symptoms reported by athlete | Headache Nausea Balance problems or dizziness Double or fuzzy/blurry vision Sensitivity to light or noise Feeling sluggish or slowed down Feeling “foggy” or groggy Concentration or memory problems Change in sleep pattern (appears later) Feeling fatigued |
Table 10.9 American Academy of Neurology’s (1997) signs and symptoms of concussion. Reproduced, with permission, from Table 1 and 2 from ‘Practice Parameter: the management of concussion in sports’ © American Academy of Neurology
| Features of concussion frequently observed | Vacant stare (befuddled facial expression) Delayed verbal and motor responses (slow to answer questions or follow instructions) Confusion and inability to focus attention (easily distracted and unable to follow through with normal activities) Disorientation (walking in the wrong direction, unaware of time, date and place) Slurred or incoherent speech (making disjointed or incomprehensible statements) Gross observable incoordination (stumbling, inability to walk tandem/straight line) Emotions out of proportion to circumstances (distraught, crying for no apparent reason) Memory deficits (exhibited by the athlete repeatedly asking the same question that has already been answered, or inability to memorise and recall 3 of 3 words or 3 of 3 objects in 5 minutes) Any period of loss of consciousness (paralytic coma, unresponsiveness to arousal) |
| Symptoms of concussion | Early (minutes to hours): Headache Dizziness or vertigo Lack of awareness of surroundings Nausea or vomiting Late (days to weeks): Persistent low grade headache Light-headedness Poor attention and concentration Memory dysfunction Easy fatigability Irritability and low frustration tolerance Intolerance of bright lights or difficulty focusing vision Intolerance of loud noises, sometimes ringing in the ears Anxiety and/or depressed mood Sleep disturbance |
Presuming a non-emergency episode of potential concussion, the sport rehabilitator should embark on the history, inspection, palpation and special testing paradigm described previously. Appropriate modification of these is warranted. For example, an athlete’s mental status may preclude their ability to offer satisfactory answers to injury history questions. (This substantiates the value of qualified pitchside healthcare practitioners for firsthand observation of an injury episode that provides key information to the evaluation.) The observation step coincides heavily with the special testing phase of the examination because so many of the special tests require visual interpretation by the examiner. Palpation in this instance is usually utilised to determine cranial or facial tenderness associated directly with the offending blow or muscular tenderness that results from reflexive contraction of the neck musculature when the head is struck. Table 10.10 outlines diagnostic criteria for assessing concussion; this information provides an excellent pitchside guide for the sport rehabilitator.
Table 10.10 Pitch side evaluation of suspected concussion (adapted from the American Academy of Neurology 1997)
| Mental status testing | Orientation | Report time, place, person and situation (circumstances of injury) |
| Concentration | Count presented digits backward (e.g. 3-1-7, 4-6-8-2, 5-3-0-7-4) | |
| Name months of the year in reverse order | ||
| Memory | Name the teams in prior match | |
| Recall 3 words and 3 objects at 0 and 5 minutes | ||
| Recall recent newsworthy events | ||
| Recall details of the match (plays, moves, strategies, etc.) | ||
| External provocative tests | Any appearance of associated symptoms is abnormal, e.g. headaches, dizziness, nausea, unsteadiness, photophobia, blurred or double vision, emotional liability or mental status changes | Complete 35 metre sprint Complete 5 push-ups Complete 5 sit-ups Complete 5 knee bends |
| Neurologic tests | Pupils | Observe symmetry and reaction |
| Coordination | Touch finger to nose | |
| Touch right finger to left finger | ||
| Observe tandem gait | ||
| Sensation | Touch finger to nose (eyes closed) | |
| Balance in Romberg test |
There are important cautions for the sport rehabilitator when evaluating the athlete with a closed head injury. In his report of neuropsychological testing algorithms for suspected concussion in high school, university and professional athletes, Randolph (2001) identifies the increased sophistication necessary for each subsequent sport proficiency level because of the higher stakes for participants (e.g. stature, salary, importance of a given competition). He offers a model for neuropsychological evaluation that is customised for each level and also recommends baseline evaluations be collected from every player, something which is clearly more feasible for the professional clubs.
Concussion case study
An 18-year-old North American football player arrived at his university for the beginning of pre-season training. A typical training schedule was followed with the players wearing only T-shirts, shorts and headgear for two days and then wearing headgear and shoulder pads for the next few days in order to acclimatise to the workload and environmental conditions. On the second day of training with the full complement of equipment the player participated in a tackling drill and received a blow to the head that was hard, but not extreme. He was obviously shaken by the play, and he came off the field to be evaluated by the medical staff.
Concussion: history
The player denied loss of consciousness – which was corroborated by the medical staff who witnessed his collision and the events immediately subsequent – but he did report a mild instance of “seeing stars.” He was oriented to his surroundings and able to accurately relate the circumstances of the injury. On questioning he indicated that his head felt “a little foggy.” He was slightly disoriented and his vision was unfocused for a few seconds. These symptoms resolved in less than five minutes. A mild headache was the player’s one enduring symptom.
Concussion: inspection
The player’s pupils were of appropriate and equal size and responsive to light. He did not exhibit any abnormal signs; otorrhea, rhinorrhea and Battle’s sign were all absent. No signs of serious injury were outwardly apparent.
Concussion: palpation
The player’s skull, cervical spine and neck musculature were systematically palpated for areas of point tenderness that could indicate pathology. There was some tenderness in his right trapezius muscle along the neck, but all other areas were non-tender.
Concussion: special testing
The player’s vital signs were within normal limits at baseline and continued so. Evaluations of the cranial nerves were normal. Ocular tracking was normal, although the player mentioned needing to concentrate to complete the task. His visual acuity was normal. He completed the Romberg test for balance successfully with his eyes closed. Motor coordination testing was normal. The player’s neck soreness was accentuated slightly by active resistive muscle testing for right lateral flexion and hyperextension of the cervical spine.
Concussion: information collating and decision making
Based on the above described information that was gathered during the acute injury examination the player was diagnosed with a mild grade 2 concussion. This was due primarily to his descriptions of how he felt during and immediately following the injury. Although his symptoms generally resolved quickly, he continued to report a headache that lasted beyond 15 minutes and slight neck musculature tenderness. Thus, the player was excluded from further participation pending complete symptom resolution. The player’s headgear was collected in order to prevent an attempt to return to training without medical clearance. The coach was informed that the player would be ineligible for participation until his symptoms subsided. The player was instructed about the signs and symptoms of head injuries and their follow-up care and was dismissed with a plan for his teammates to monitor him during the next 24 hours. Specific directions about reporting new or worsening symptoms were provided, and the medical staff made arrangements for his follow-up care.
Concussion: follow-up for return to sport
The player presented himself to the sport medicine clinic on a daily basis. In close communication with the team physician, the sport rehabilitator evaluated the player at each visit using standard concussion evaluation techniques. A fortnight later the player’s headache was completely resolved and all other concussion tests were normal. However, he continued to exhibit mild myofascial neck pain with resisted cervical motions. This was presumed to be a residual sign of reflexive contraction of the neck musculature during the injury episode.
At two weeks post-injury the player was referred to the radiology department for a CT scan of his neck in order to investigate the persistent pain. Review of the CT images revealed the player suffered from a previously undetected congenital tripartite C1 vertebra. On the basis of this finding the player was excluded from further participation in collision sports and counselled about alternative sporting outlets that would not expose his cervical spine to catastrophic risk. It was obviously fortunate that during his preceding several years of North American football involvement he did not sustain a disastrous neck injury. This case exemplifies the need for alertness to symptoms that may be unrelated to the primary pathology. A conservative approach is particularly appropriate for injuries to the central nervous system.
Conclusion
Acute management entails evaluation of the injury and application of appropriate treatments based on decisions informed by the evaluation’s results. This process, especially the evaluation, is enhanced by the clinician’s presence at training sessions and competitions where they can witness the mechanism of injuries. Following the injury evaluation and categorisation of the injury’s nature and severity, prompt administration of proper on-site care should ensue. In non-emergent cases this will include judicious application of the PRICE method: protection, rest, ice, compression and elevation.
Success in managing the acute stage of injury generally leads to success in the post-acute stage and onward as the athlete is prepared by healthcare professionals and others on the sport healthcare team for re-entry to participation. Insofar as possible, it is incumbent on the sport rehabilitator to ensure this process goes smoothly, to offer physical and psychological support and to keep the athlete’s best interests foremost during the progression back to full activity.
References
Ahmad, S.R. (2007) Safety of recommended doses of paracetamol. Lancet, 369 (9560), 462–463.
Algafly, A.A. and George, K.P. (2007) The effect of cryotherapy on nerve conduction velocity, pain threshold and pain tolerance. British Journal of Sports Medicine, 41 (6), 365–369.
Alla, S., Sullivan, S.J., Hale, L. and McCrory, P. (2009) Self-report scales/checklists for the measurement of concussion symptoms: a systematic review. British Journal of Sports Medicine, 43 (Suppl I), i3–i12.
American Academy of Neurology (1997) Practice parameter: the management of concussion in sports (summary statement). Neurology, 48, 581–585.
American College of Sports Medicine (2006) Concussion (mild traumatic brain injury) and the team physician: a consensus statement. Medicine and Science in Sports and Exercise, 38 (2), 395–399.
Anonymous. (2005) Stedman’s Medical Dictionary for the Health Professions and Nursing. Philadelphia, PA: Lippincott Williams and Wilkins.
Bachmann, L.M., Kolb, E., Koller, M.T., Steurer, J. and ter Riet, G. (2003) Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. British Medical Journal, 326 (7386), 417–423.
Banning, M. (2008) Topical diclofenac: clinical effectiveness and current uses in osteoarthritis of the knee and soft tissue injuries. Expert Opinion on Pharmacotherapy, 9 (16), 2921–2929.
Bender, T., Nagy, G., Barna, I., Tefner, I., Kádas, É. and Géher, P. (2007) The effect of physical therapy on beta-endorphin levels. European Journal of Applied Physiology, 100 (4), 371–382.
Bertalanffy, A., Kober, A., Bertalanffy, P., Gustorff, B., Gore, O., Adel, S. and Hoerauf, K. (2005) Transcutaneous electrical nerve stimulation reduces acute low back pain during emergency transport. Academic Emergency Medicine, 12 (7), 607–611.
Blackham, J.E.J., Claridge, T. and Benger, J.R. (2008) Can patients apply the Ottawa ankle rules to themselves? Emergency Medicine Journal, 25 (11), 750–751.
Bleakley, C., McDonough, S. and MacAuley, D. (2004) The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. American Journal of Sports Medicine, 32 (1), 251–261.
Bleakley, C.M., McDonough, S.M., MacAuley, D.C. and Bjordal, J. (2006) Cryotherapy for acute ankle sprains: a randomised controlled study of two different icing protocols. British Journal of Sports Medicine, 40 (8), 700–705.
Bleakley, C., O’Connor, S., Tully, M., Rocke, L., MacAuley, D. and McDonough, S. (2007) The PRICE study (Protection Rest Ice Compression Elevation): design of a randomised controlled trial comparing standard versus cryokinetic ice applications in the management of acute ankle sprain [ISRCTN13903946]. BMC Musculoskeletal Disorders, 8 (1), 125.
Boyce, S.H., Quigley, M.A. and Campbell, S. (2005) Management of ankle sprains: a randomised controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. British Journal of Sports Medicine, 39 (2), 91–96.
Brooks, J.H.M. and Fuller, C.W. (2006) The influence of methodological issues on the results and conclusions from epidemiological studies of sports injuries: illustrative examples. Sports Medicine, 36 (6), 459–472.
Brooks, J.H.M., Fuller, C.W., Kemp, S.P.T. and Reddin, D.B. (2005) A prospective study of injuries and training amongst the England 2003 Rugby World Cup squad. British Journal of Sports Medicine, 39 (5), 288–293.
Brooks, J.H.M., Fuller, C.W., Kemp, S.P.T. and Reddin, D.B. (2008) An assessment of training volume in professional rugby union and its impact on the incidence, severity, and nature of match and training injuries. Journal of Sports Sciences, 26 (8), 863–873.
Caine, D., Caine, C. and Maffulli, N. (2006) Incidence and distribution of pediatric sport-related injuries. Clinical Journal of Sport Medicine, 16 (6), 500–513.
Cantu, R.C. (1988) Second-impact syndrome. Clinics in Sports Medicine, 17, 37–44.
Carroll, D., Tramer, M., McQuay, H., Nye, B. and Moore, A. (1996) Randomization is important in studies with pain outcomes: systematic review of transcutaneous electrical nerve stimulation in acute postoperative pain. British Journal of Anaesthesia, (6), 798–803.
Collins, M.W., Lovell, M.R., Iverson, G.L., Cantu, R.C., Maroon, J.C. and Field, M. (2002) Cumulative effects of concussion in high school athletes. Neurosurgery, 51 (5), 1175–1181.
Collins, N.C. (2008) Is ice right? Does cryotherapy improve outcome for acute soft tissue injury? Emergency Medicine Journal, 25 (2), 65–68.
Dale, R.B., Harrelson, G.L. and Leaver-Dunn, D. (2004) Principles of rehabilitation. In Andrews, J.R., Harrelson, G.L. and Wilk, K.E. (Eds) Physical Rehabilitation of the Injured Athlete, 3rd edn. Philadelphia, PA: Saunders, pp. 157–188.
Delis, K.T., Azizi, Z.A., Stevens, R.J.G., Wolfe, J.H.N. and Nicolaides, A.N. (2000) Optimum intermittent pneumatic compression stimulus for lower-limb venous emptying. European Journal of Vascular and Endovascular Surgery, 19 (3), 261–269.
Department of Trade and Industry (2003) 24th (Final) Report of the Home and Leisure Accident Surveillance System, London: Department of Trade and Industry.
Dickenson, A.H. (2002) Gate Control Theory of pain stands the test of time. British Journal of Anaesthesia, 88 (6), 755–757.
Dominkus, M., Nicolakis, M., Kotz, R., Wilkinson, F.E., Kaiser, R.R. and Chlud, K. (1996) Comparison of tissue and plasma levels of ibuprofen after oral and topical administration. Arzneimittel-Forschung, 46 (12), 1138–1143.
Ekstrand, J. and Karlsson, J. (2003) The risk for injury in football. There is a need for a consensus about definition of the injury and the design of studies. Scandinavian Journal of Medicine and Science in Sports, 13 (3), 147–149.
Ernst, E. and Fialka, V. (1994) Ice freezes pain? A review of the clinical effectiveness of analgesic cold therapy. Journal of Pain and Symptom Management, 9 (1), 56–59.
Fazio, V.C., Lovell, M.R., Pardini, J.E. and Collins, M.W. (2007) The relation between post concussion symptoms and neurocognitive performance in concussed athletes. NeuroRehabilitation, 22 (3), 207–216.
Fischer, J., Van Lunen, B.L., Branch, J.D. and Pirone, J.L. (2009) Functional performance following an ice bag application to the hamstrings. Journal of Strength and Conditioning Research, 23 (1), 44–50.
Flegel, M.J. (2008) Sport First Aid, Champaign, IL: Human Kinetics.
Fong, D.T.-P., Hong, Y., Chan, L.-K., Yung, P.S.-H. and Chan, K.-M. (2007) A systematic review on ankle injury and ankle sprain in sports. Sports Medicine, 37 (1), 73–94.
Fuller, C.W., Laborde, F., Leather, R.J. and Molloy, M.G. (2008) International Rugby Board Rugby World Cup 2007 injury surveillance study. British Journal of Sports Medicine, 42 (6), 452–459.
Gabbett, T.J. (2004) Incidence of injury in junior and senior Rugby League players. Sports Medicine, 34 (12), 849–859.
Garrick, J.G. (1977) The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. American Journal of Sports Medicine, 5 (6), 241–242.
Giza, C.C. and Hovda, D.A. (2001) The neurometabolic cascade of concussion. Journal of Athletic Training, 36 (3), 228–235.
Gøtzsche, P.C. (2006) [Paracetamol has the same effect as non-steroidal anti-inflammatory agents in acute musculoskeletal injuries]. Ugeskrift for Laeger, 168 (20), 1981–1982.
Graham, G.G., Scott, K.F. and Day, R.O. (2003) [Tolerability of paracetamol]. Drugs, 63 (Spec. No. 2), 43–46.
Guskiewicz, K.M., Bruce, S.L., Cantu, R.C., Ferrara, M.S., Kelly, J.P., McCrea, M., Putukian, M. and Valovich McLeod, T.C. (2004) National Athletic Trainers’ Association position statement: management of sport-related concussion. Journal of Athletic Training, 39 (3), 280–297.
Hawkins, R.D. and Fuller, C.W. (1999) A prospective epidemiological study of injuries in four English professional football clubs. British Journal of Sports Medicine, 33 (3), 196–203.
Hayden, C.A. (1964) Cryokinetics in an early treatment program. Physical Therapy, 44, 990–993.
Herman, E., Williams, R., Stratford, P., Fargas-Babjak, A. and Trott, M. (1994) A randomized controlled trial of transcutaneous electrical nerve stimulation (CODETRON) to determine its benefits in a rehabilitation program for acute occupational low back pain. Spine, 19 (5), 561–568.
Hildebrand, K.A., Hart, D.A., Rattner, J.B., Marchuk, L.L. and Frank, C.B. (2007) Ligament injuries: pathophysiology, healing, and treatment considerations. in Magee, D.J., Zachazewski, J.E. and Quillen, W.S. (Eds) Scientific Foundations and Principles of Practice in Musculoskeletal Rehabilitation. St. Louis, MO: Saunders, pp. 23–47.
Hodgson, L., Gissane, C., Gabbett, T.J. and King, D.A. (2007) For debate: consensus injury definitions in team sports should focus on encompassing all injuries. Clinical Journal of Sport Medicine, 17 (3), 188–191.
Holbourn, A.H.S. (1945) The mechanics of brain injuries. British Medical Bulletin, 3 (6), 147–149.
Hootman, J.M., Dick, R. and Agel, J. (2007) Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. Journal of Athletic Training, 42 (2), 311–319.
Hsueh, T.-C., Cheng, P.-T., Kuan, T.-S. and Hong, C.-Z. (1997) The immediate effectiveness of electrical nerve stimulation and electrical muscle stimulation on myofascial trigger points. American Journal of Physical Medicine and Rehabilitation, 76 (6), 471–476.
Hubbard, T.J. and Denegar, C.R. (2004) Does cryotherapy improve outcomes with soft tissue injury? Journal of Athletic Training, 39 (3), 278–279.
Hughes, G.S., Lichstein, P.R., Whitlock, D. and Harker, C. (1984) Response of plasma beta-endorphins to transcutaneous electrical nerve stimulation in healthy subjects. Physical Therapy, 64 (7), 1062–1066.
Iverson, G.L., Gaetz, M., Lovell, M.R. and Collins, M.W. (2004) Cumulative effects of concussion in amateur athletes. Brain Injury, 18 (5), 433–443.
Jalan, R., Williams, R. and Bernuau, J. (2007) Paracetamol: are therapeutic doses entirely safe? Lancet, 368 (9554), 2195–2196.
Johnson, M.I. and Tabasam, G. (2003) An investigation into the analgesic effects of interferential currents and transcutaneous electrical nerve stimulation on experimentally induced ischemic pain in otherwise pain-free volunteers. Physical Therapy, 83 (3), 208–223.
Jorge, S., Parada, C.A., Ferreira, S.H. and Tambeli, C.H. (2006) Interferential therapy produces antinociception during application in various models of inflammatory pain. Physical Therapy, 86 (6), 800–808.
Jüni, P., Nartey, L., Reichenbach, S., Sterchi, R., Dieppe, P.A. and Egger, M. (2004) Risk of cardiovascular events and rofecoxib: cumulative meta-analysis. The Lancet, 364 (9450), 2021–2029.
Katayama, Y., Becker, D.P., Tamura, T. and Hovda, D.A. (1990) Massive increases in extracellular potassium and the indiscriminate release of glutamate following concussive brain injury. Journal of Neurosurgery, 73 (6), 889–900.
Kehlet, H. and Werner, M.U. (2003) [Role of paracetamol in the acute pain management]. Drugs, 63 (Spec. No. 2), 15–22.
Kersey, R.D. (1998) Acute subdural hematoma after a reported mild concussion: a case report. Journal of Athletic Training, 33 (3), 264–268.
King, D.A., Gabbett, T.J., Gissane, C. and Hodgson, L. (2009) Epidemiological studies of injuries in rugby league: suggestions for definitions, data collection and reporting methods. Journal of Science and Medicine in Sport, 12 (1), 12–19.
Knight, K.L. (1995) Cryotherapy in Sport Injury Management. Champaign, IL: Human Kinetics.
Knight, K.L. (2008) More precise classification of orthopaedic injury types and treatment will improve patient care. Journal of Athletic Training, 43 (2), 117–118.
Knight, K.L. and Draper, D.O. (2008) Therapeutic Modalities: The Art and Science. Baltimore, MD: Lippincott Williams and Wilkins.
Knight, K.L. and Londeree, B.R. (1980) Comparison of blood flow in the ankle of uninjured subjects during therapeutic applications of heat, cold, and exercise. Medicine and Science in Sports and Exercise, 12 (1), 76–80.
Knowles, S.B., Marshall, S.W. and Guskiewicz, K.M. (2006) Issues in estimating risks and rates in sports injury research. Journal of Athletic Training, 41 (2), 207–215.
Leddy, J.J., Smolinski, R.J., Lawrence, J., Snyder, J.L. and Priore, R.L. (1998) Prospective evaluation of the Ottawa Ankle Rules in a university sports medicine center: with a modification to increase specificity for identifying malleolar fractures. American Journal of Sports Medicine, 26 (2), 158–165.
Leddy, J.J., Kesari, A. and Smolinski, R.J. (2002) Implementation of the Ottawa ankle rule in a university sports medicine center. Medicine and Science in Sports and Exercise, 34 (1), 57–62.
Lessard, L.A., Scudds, R.A., Amendola, A. and Vaz, M.D. (1997) The efficacy of cryotherapy following arthroscopic knee surgery. Journal of Orthopaedic and Sports Physical Therapy, 26 (1), 14–22.
Lovell, M.R., Collins, M. and Bradley, J. (2004) Return to play following sports-related concussion. Clinics in Sports Medicine, 23 (3), 421–441.
Magee, D.J. (2008) Orthopedic Physical Assessment. Philadelphia, PA: Saunders Elsevier.
Makdissi, M., McCrory, P., Ugoni, A., Darby, D. and Brukner, P. (2009) A prospective study of postconcussive outcomes after return to play in Australian football. American Journal of Sports Medicine, 37 (5), 877–883.
McCallum, M.I.D., Glynn, C.J., Moore, R.A., Lammer, P. and Phillips, A.M. (1988) Transcutaneous electrical nerve stimulation in the management of acute postoperative pain. British Journal of Anaesthesia, 61 (3), 308–312.
McCarthy, D.M. (2001) Prevention and treatment of gastrointestinal symptoms and complications due to NSAIDs. Best Practice and Research Clinical Gastroenterology, 15 (5), 755–773.
McCrory, P.R. and Berkovic, S.F. (1998) Second impact syndrome. Neurology, 50, 677–683.
McCrory, P., Meeuwisse, W., Johnston, K., Dvorak, J., Aubry, M., Molloy, M. and Cantu, R. (2009) Consensus Statement on Concussion in Sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Journal of Athletic Training, 44 (4), 434–448.
McMaster, W.C., Liddle, S. and Waugh, T.R. (1978) Laboratory evaluation of various cold therapy modalities. American Journal of Sports Medicine, 6 (5), 291–294.
Melzack, R. and Wall, P.D. (1965) Pain mechanisms: a new theory. Science, 150 (3699), 971–979.
Merrick, M.A. (2004) Therapeutic modalities as an adjunct to rehabilitation. in Andrews, J.R., Harrelson, G.L. and Wilk, K.E. (Eds) Physical Rehabilitation of the Injured Athlete, 3rd edn. Philadelphia, PA: Saunders, pp. 51–98.
Merrick, M.A. (2007) Physiological bases of physical agents. In Magee, D.J., Zachazewski, J.E. and Quillen, W.S. (Eds) Scientific Foundations and Principles of Practice in Musculoskeletal Rehabilitation. St. Louis, MO: Saunders, pp. 237–254.
Merrick, M.A., Rankin, J.M., Andres, F.A. and Hinman, C.L. (1999) A preliminary examination of cryotherapy and secondary injury in skeletal muscle. Medicine and Science in Sports and Exercise, 31 (11), 1516–1521.
Merrick, M.A., Jutte, L.S. and Smith, M.E. (2003) Cold modalities with different thermodynamic properties produce different surface and intramuscular temperatures. Journal of Athletic Training, 38 (1), 28–33.
Milne, L. (1996) Ottawa ankle decision rules. Western Journal of Medicine, 164 (1), p. 67.
Miyatake, S., Ichiyama, H., Kondo, E. and Yasuda, K. (2009) Randomized clinical comparisons of diclofenac concentration in the soft tissues and blood plasma between topical and oral applications. British Journal of Clinical Pharmacology, 67 (1), 125–129.
Mora, S., Zalavras, C.G., Wang, L. and Thordarson, D.B. (2002) The role of pulsatile cold compression in edema resolution following ankle fractures: a randomized clinical trial. Foot and Ankle International, 23 (11), 999–1002.
Mori, T., Katayama, Y. and Kawamata, T. (2006) Acute hemispheric swelling associated with thin subdural hematomas: pathophysiology of repetitive head injury in sports. Acta Neurochirurgica. Supplement, 96, 40–43.
Moynihan, R. (2002) FDA fails to reduce accessibility of paracetamol despite 450 deaths a year. British Medical Journal, 325 (7366), p. 678.
Myrer, J.W., Measom, G. and Fellingham, G.W. (1998) Temperature changes in the human leg during and after two methods of cryotherapy. Journal of Athletic Training, 33 (1), 25–29.
National Athletic Trainers’ Association (2007) Recommendations and Guidelines for Appropriate Medical Coverage of Intercollegiate Athletics. Dallas, TX: National Athletic Trainers’ Association.
National Collegiate Athletic Association (2008) 2008–09 NCAA Sports Medicine Handbook, Indianapolis, IA: National Collegiate Athletic Association.
Nugent, P.L. (2004) Ottawa ankle rules accurately assess injuries and reduce reliance on radiographs. Journal of Family Practice, 53 (10), 785–788.
Ommaya, A.K. and Gennarelli, T.A. (1974) Cerebral concussion and traumatic unconsciousness: correlation of experimental and clinical observations on blunt head injuries. Brain, 97 (1), 633–654.
Ordog, G.J. (1987) Transcutaneous electrical nerve stimulation versus oral analgesic: A randomized double-blind controlled study in acute traumatic pain. American Journal of Emergency Medicine, 5 (1), 6–10.
Otte, J.W., Merrick, M.A., Ingersoll, C.D. and Cordova, M.L. (2002) Subcutaneous adipose tissue thickness alters cooling time during cryotherapy. Archives of Physical Medicine and Rehabilitation, 83 (11), 1501–1505.
Papacostas, E., Malliaropoulos, N., Papadopoulos, A. and Liouliakis, C. (2001) Validation of Ottawa ankle rules protocol in Greek athletes: study in the emergency departments of a district general hospital and a sports injuries clinic. British Journal of Sports Medicine, 35 (6), 445–447.
Patrono, C. and Rocca, B. (2009) Nonsteroidal antiinflammatory drugs: past, present and future. Pharmacological Research, 59 (5), 285–289.
Powell, J.W. and Dompier, T.P. (2004) Analysis of injury rates and treatment patterns for time-loss and non-time-loss injuries among collegiate student-athletes. Journal of Athletic Training, 39 (1), 56–70.
Quillen, W.S. and Rouillier, L.H. (1982) Initial management of acute ankle sprains with rapid pulsed pneumatic compression and cold. Journal of Orthopaedic and Sports Physical Therapy, 4 (1), 39–43.
Randolph, C. (2001) Implementation of neuropsychological testing models for the high school, collegiate, and professional sport settings. Journal of Athletic Training, 36 (3), 288–296.
Rovenský, J., Miceková, D., Gubzová, Z., Fimmers, R., Lenhard, G., Vögtle-Junkert, U. and Screyger, F. (2001) Treatment of knee osteoarthritis with a topical non-steroidal antiinflammatory drug: results of a randomized, double-blind, placebo-controlled study on the efficacy and safety of a 5% ibuprofen cream. Drugs Under Experimental and Clinical Research, 27 (5–6), 209–221.
Royal Society for the Prevention of Accidents. (2009) Home and leisure accident statistics. [online]. Birmingham, UK. [accessed 14th March 2009]. <http://www.hassandlass.org.uk/query/index.htm>.
Rucinkski, T.J., Hooker, D.N., Prentice, W.E., Shields, E.W. and Cote-Murray, D.J. (1991) The effects of intermittent compression on edema in postacute ankle sprains. Journal of Orthopaedic and Sports Physical Therapy, 14 (2), 65–69.
Stanos, S.P. (2007) Topical agents for the management of musculoskeletal pain. Journal of Pain and Symptom Management, 33 (3), 342–355.
Starkey, J.A. (1976) Treatment of ankle sprains by simultaneous use of intermittent compression and ice packs. American Journal of Sports Medicine, 4 (4), 142–144.
Stiell, I.G., Greenberg, G.H., McKnight, R.D., Nair, R.C., McDowell, I. and Worthington, J.R. (1992) A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Annals of Emergency Medicine, 21 (4), 384–390.
Stiell, I.G., McKnight, R.D., Greenberg, G.H., McDowell, I., Nair, R.C., Wells, G.A., Johns, C. and Worthington, J.R. (1994) Implementation of the Ottawa ankle rules. Journal of the American Medical Association, 271 (11), 827–832.
Stiell, I.G., Greenberg, G.H., Wells, G.A., McKnight, R.D., Cwinn, A.A., Cacciotti, T., McDowell, I. and Smith, N.A. (1995) Derivation of a decision rule for the use of radiography in acute knee injuries. Annals of Emergency Medicine, 26 (4), 405–413.
Stiell, I.G., Greenberg, G.H., Wells, G.A., McDowell, I., Cwinn, A.A., Smith, N.A., Cacciotti, T. and Sivilotti, M.L. (1996) Prospective validation of a decision rule for the use of radiography in acute knee injuries. Journal of the American Medical Association, 275 (8), 611–615.
Swenson, C., Swärd, L. and Karlsson, J. (1996) Cryotherapy in sports medicine. Scandinavian Journal of Medicine and Science in Sports, 6 (4), 193–200.
Tigges, S., Pitts, S., Mukundan, S., Jr., Morrison, D., Olson, M. and Shahriara, A. (1999) External validation of the Ottawa knee rules in an urban trauma center in the United States. American Journal of Roentgenology, 172 (4), 1069–1071.
Toth, C. (2008) The epidemiology of injuries to the nervous system resulting from sport and recreation. Neurologic Clinics, 26 (1), 1–31.
Tsang, K.K., Hertel, J. and Denegar, C.R. (2003) Volume decreases after elevation and intermittent compression of postacute ankle sprains are negated by gravity-dependent positioning. Journal of Athletic Training, 38 (4), 320–324.
van Mechelen, W., Hlobil, H. and Kemper, H.C. (1996) Incidence, severity, aetiology and prevention of sports injuries: a review of concepts. Sports Medicine, 14 (2), 82–99.
Vanscheidt, W., Ukat, A. and Partsch, H. (2009) Dose-response of compression therapy for chronic venous edema – higher pressures are associated with greater volume reduction: Two randomized clinical studies. Journal of Vascular Surgery, 49 (2), 395–402.
Vardeny, O. and Solomon, S.D. (2008) Cyclooxygenase-2 inhibitors, nonsteroidal anti-inflammatory drugs, and cardiovascular risk. Cardiology Clinics, 26 (4), 589–601.
Walsh, D.M., Howe, T.E., Johnson, M.I. and Sluka, K.A. (2009) Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database of Systematic Reviews, 15 (2), p.CD006142.
Whitefield, M., O’Kane, C.J.A. and Anderson, S. (2002) Comparative efficacy of a proprietary topical ibuprofen gel and oral ibuprofen in acute soft tissue injuries: a randomized, double-blind study. Journal of Clinical Pharmacy and Therapeutics, 27 (6), 409–417.
Wilkerson, G.B. (1991) Treatment of the inversion ankle sprain through synchronous application of focal compression and cold. Journal of Athletic Training, 26, 220–237.
Wilkerson, G.B. and Horn-Kingery, H.M. (1993) Treatment of the inversion ankle sprain: comparison of different modes of compression and cryotherapy. Journal of Orthopaedic and Sports Physical Therapy, 17 (5), 240–246.
Withnall, C., Shewchenko, N., Wonnacott, M. and Dvorak, J. (2005) Effectiveness of headgear in football. British Journal of Sports Medicine, 39 (Suppl 1), i40–i48.
Woo, W.W.K., Man, S.-Y., Lam, P.K.W. and Rainer, T.H. (2005) Randomized double-blind trial comparing oral paracetamol and oral nonsteroidal antiinflammatory drugs for treating pain after musculoskeletal injury. Annals of Emergency Medicine, 46 (4), 352–361.
Yang, C.-C., Hua, M.-S., Tu, Y.-K. and Huang, S.-J. (2009) Early clinical characteristics of patients with persistent post-concussion symptoms: A prospective study. Brain Injury, 23 (4), 299–306.
Yeung, M.S., Chan, K.M., So, C.H. and Yuan, W.Y. (1994) An epidemiological survey on ankle sprain. British Journal of Sports Medicine, 28 (2), 112–116.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







