Fig. 30.1
MRI of 75-year-old woman after posterior stabilized TKR with a zirconium femoral component. The sagittal MR image shows very little metal susceptibility artifact. The soft tissues including the extensor mechanism can easily be evaluated. The bone-prosthesis interface of all components is clearly visualized. There is cement protrusion along several drill holes in femur and tibia. There are no gaps between the components and the bone. There is minor effusion
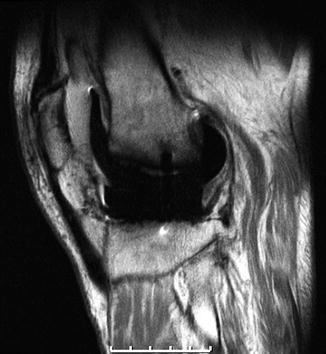
Fig. 30.2
Loosening of a femoral zirconium prosthesis in a 54-year-old patient with complete detachment as documented by the wide gaps between implant and bone
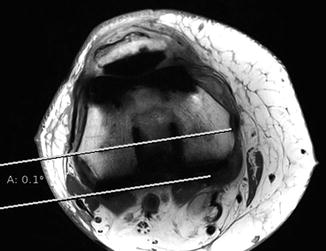
Fig. 30.3
Axial MRI of the same patient as in Fig. 30.1 (right knee): Neutral rotational alignment is displayed without any major overlying artifacts

Fig. 30.4
Artifacts with femoral CoCr components remain a challenge in MRI following knee arthroplasty. This image shows significant periprosthetic metallic susceptibility artifact interfering with the evaluation of the bone-cement interface. The soft tissue envelope and the patellar and tibial components are not affected by these artifacts. Newer protocols will help to overcome this problem
CoCr components interfere more with MRI than those made of titanium alloys or OxZr.
30.2 Clinical Evidence
In 2003, MRI proved clinically useful in the evaluation of patients with painful TKR [25, 23]. Optimized pulse sequence parameters that are available on most commercial MR units were designed to reduce metallic artifact susceptibility and added to traditional imaging techniques. Potter et al. described several cases where MRI helped diagnose arthrofibrosis, synovitis, loosening, chronic infection, osteolysis, particle disease, and peroneal nerve palsy in a series of painful or nonfunctional TKR [23].
Until today, publications in this field remain relatively scarce. The understanding of indications and interpretation of MRI after knee replacement is evolving. Several studies reported on evaluation of periprosthetic osteolysis [20, 27, 26]. MRI allowed for good reproducibility of analysis of the implant-bone interface at the tibia and patella following TKR. The femoral interface was visualized for components made of zirconium. Conventional CoCr femoral components caused considerable artifact and interfered with the evaluation of the femoral interface (Figs. 30.1, 30.2, and 30.3) [11]. MRI has also been shown to be helpful for the analysis of rotational component alignment (Fig. 30.4) [12, 17, 21]. The soft tissue envelope around a TKR is usually well visualized on MRI [24], which can help to detect ruptures of tendons or distention of the capsule (Fig. 30.5). In one study, the patellar clunk syndrome, which today is rare, was diagnosed with MRI, and MRI helped choose treatment options [13]. In a case series of patients presenting with unexplained hemarthrosis, MRI characterized the vascular joint anatomy and identified hypervascular synovium. Subsequent embolization or synovectomy was curative in most of these patients [7].


Fig. 30.5
A quadriceps tendon rupture in a 50-year-old female following revision knee replacement is displayed (arrow). There are relatively large artifacts due to the hinged and stemmed revision implant that do not interfere with evaluation of the extensor mechanism
An experimental approach advocated the use of MRI for assessment of in vivo kinematics after TKR [2, 19]. In a technical report, Kamishima et al. compared imaging with 1.5 and 3 T magnets following TKR. They concluded that zirconium implants could safely be scanned and that superior quality was obtained with the 3 T MRI [18].
In partial knee replacement such as patellofemoral replacement (PFR) or unicondylar knee replacement (UKR), the metallic burden for imaging is lower. On the other hand, preserved compartments can deteriorate with time, and cartilage damage and meniscal tears can easily be assessed via MRI. MRI proved effective in evaluation of all preserved soft tissue structures following both UKR and PFR [15, 16]. MRI also allows for evaluation of component positioning of partial knee replacement [14, 10].
30.3 Challenges and Opportunities
Until now, the knowledge about effective protocols for MRI after knee replacement and their scientific evaluation has been limited to few centers. This is not an issue of infrastructure, as the MRI protocols necessary to reduce metal artifact are available on most commercial MRI units [25]. It is the surgeon’s responsibility to indicate MRI for painful joints after arthroplasty. The appropriate protocols and close communication between surgeon, radiologist, and patient will overcome an initial learning curve.
MRI is a sensitive tool. As in the natural knee, MRI findings such as cartilage damage, gaps at the interface, or component malposition have to be related to a clinical symptom. MRI adds significant costs to the workup of a painful joint and must be indicated responsibly.
CoCr components remain a challenge in MRI imaging. Newer protocols may be particularly helpful in the evaluation of CoCr implants in the future. Protocols such as MAVRIC or SEMAC that involve multiple acquisitions slightly offset from the dominant frequency with a recombinant image have been described to decrease artifact with these alloys [8, 3].
Specific metal artifact reduction protocols such as SEMAC or MAVRIC reduce metal artifacts.
MRI has already proven to be a helpful tool. Board approval of study protocols that require multiplanar imaging may be facilitated, as there is no need for ionizing radiation with MRI. There are attempts to use MRI in the diagnosis of arthroplasty infection [22] and in kinematic studies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








