Madelung Deformity
CASE PRESENTATION
A 13-year-old female presents for evaluation of wrist pain and deformity. Patient reports noting “ugly bony bumps” on the ulnar aspects of the bilateral wrists, associated with diminished range of motion (ROM) and right wrist pain with activities of daily living and sports (Figure 15-1). Initial attempts at splinting and activity modification have not resulted in symptomatic improvement.
CLINICAL QUESTIONS
What is Madelung deformity?
Who was Madelung?
What causes the deformity? Is it hereditary? Are there associated conditions?
What is Vicker ligament?
What are the indications for surgical treatment?
What are the surgical procedures that are performed for Madelung’s?
What are the expected outcomes and possible complications from surgery?
THE FUNDAMENTALS
There are two theories on hitting the knuckleball. Unfortunately, neither of them work.
—Charlie Lau
Etiology and Epidemiology
While previously described by Dupuytren, Malgaigne, and others, Otto W. Madelung was the first to provide a comprehensive description—including discussion regarding causality and treatment—on the condition that now bears his name.1, 2, 3 and 4
Madelung’s is a relatively uncommon condition. In Flatt series of 1,476 patients with congenital hand and upper limb differences, only 1.7% of cases had Madelung’s.5 Females are more commonly affected than males, and there is often bilateral wrist involvement. Madelung’s is thought to be transmitted in an autosomal dominant fashion with variable expressivity and incomplete penetrance. This is clearly true in cases of dyschondrosteosis, or mesomelic dwarfism, with associated lower limb involvement.
The etiology of Madelung’s is unknown. Historically, identification of a thickened, fibrous volar ligament between the lunate and volar distal radius (the socalled Vicker ligament) raised the question of whether the deformity may be secondary to a soft tissue tether between the carpus and forearm.6 More recent study has elucidated that Vicker ligament is indeed an abnormally thick, short radiolunate ligament.7 We believe, as do most others, that Vicker ligament is secondary to, not the cause of, Madelung deformity. This is supported by the observation that if the tethering soft tissue structure was present at birth, greater deformity would be seen early in life, due to the hand doubling that occurs by the age of 3 years.8
More recent investigation has revealed that the classic Madelung deformity seen in females is likely due to a mutation in the SHOX homeobox gene on the X chromosome.9, 10, 11 and 12
A number of associated syndromes or genetic conditions have been identified. Most notable is Leri-Weill mesomelic dwarfism, also known as dyschondrosteosis.13, 14 and 15 This genetic association is often undiagnosed, as the short-statured patient has many relatives of similar height, and the only other obvious manifestation is the Madelung deformity (see Coach’s Corner). Other reports have cited an association with Turner syndrome.10,16 It is apparent, however, that the clinical presentation may be quite varied, and many cases may not have an obvious genetic or hereditary association.17, 18 and 19
In addition to the classic Madelung deformity discussed here, any number of other conditions may result in similar changes in the distal radius and wrist, mimicking a Madelung-like deformity. These include post-traumatic distal radial physeal arrest, sickle cell disease, post-infectious wrist deformity, and a host of skeletal dysplasias, such as multiple hereditary exostoses, Ollier disease, and post-infectious mucopolysaccharidosis.20
Clinical Evaluation
Madelung deformity is characterized by shortening and accentuated articular volar-ulnar tilt of the distal radius, due to abnormalities of the volar-ulnar distal radial physis. As the ulna is unaffected, it grows normally and adopts a seemingly elongated and dorsally prominent position (even though it is the radius that relatively shortens and grows abnormally volarly). In advanced or severe cases, the distal radioulnar joint (DRUJ) may be incongruent and widened, and the carpus will migrate proximally and volarly. Ultimately, this results in pain, decreased ROM (most notably supination and extension), and aesthetic differences of the wrist.
Patients will typically present between the ages of 8 and 14 years. While the typical complaint is of pain and difficulty with activities of daily living and/or sports, it is the visible aesthetic deformity that troubles many patients the most. Without a tinge of gender bias, this is what drives many adolescent females in to see us.
Physical examination will demonstrate the prominent distal ulna and relative volar subluxation of the carpus compared with the forearm. When observed closely, the hand sits out of plane of the forearm. Forearm supination and wrist extension may be limited according to the severity of the structural changes. The DRUJ may be lax or unstable. Distal hand function and elbow motion are preserved. In rare situations, patients may present with spontaneous ruptures of the extensor tendons, which may lead to the diagnosis.21,22
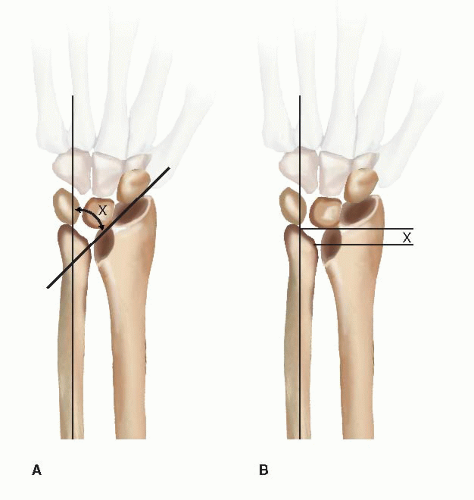
Radiographs will confirm the diagnosis (Figure 15-2). A number of radiographic measures have been proposed to quantify and categorize Madelung deformity.23,24 One of the challenges in radiographic evaluation is that traditional parameters or landmarks used in other traumatic or acquired wrist conditions cannot be utilized owing to the abnormal skeletal anatomy. McCarroll et al. have proposed radiographic measures based upon the ulnar axis, given that the ulna may be the only unaffected structure of the wrist. Ulnar tilt, lunate subsidence, lunate fossa angle, palmar tilt, and palmar carpal displacement have been described, but only ulnar tilt and lunate subsidence were found to be reliable and reproducible, with unknown correlation to wrist function or patient-rated outcomes.
Surgical Indications
Surgical treatment is recommended for persistent pain and functional limitations or progressive bony deformity in the skeletally immature patient. Patients without symptoms or with mild deformity may be observed. While aesthetics are not a primary indication for surgery, many adolescent female patients find the visible deformity troubling and may wish to proceed with surgical
correction, though they do not yet have pain or functional issues. Many of these patients have sufficient enough deformity and joint incongruity that they are at risk for ulnocarpal impaction syndrome. A thorough preoperative discussion is needed regarding the relative risks and benefits of any surgical intervention, particularly if a strong motivation is the desire for a more normal-appearing wrist. If it is subtle and pain free, most will not trade the scar and surgical grief to be rid of a small bump. If it is severe, they may be better off having surgery before carpal cartilage or triangular fibrocartilage complex injuries occur.
correction, though they do not yet have pain or functional issues. Many of these patients have sufficient enough deformity and joint incongruity that they are at risk for ulnocarpal impaction syndrome. A thorough preoperative discussion is needed regarding the relative risks and benefits of any surgical intervention, particularly if a strong motivation is the desire for a more normal-appearing wrist. If it is subtle and pain free, most will not trade the scar and surgical grief to be rid of a small bump. If it is severe, they may be better off having surgery before carpal cartilage or triangular fibrocartilage complex injuries occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree