21.1 Anatomy
William M. Falls
Gail A. Shafer-Crane
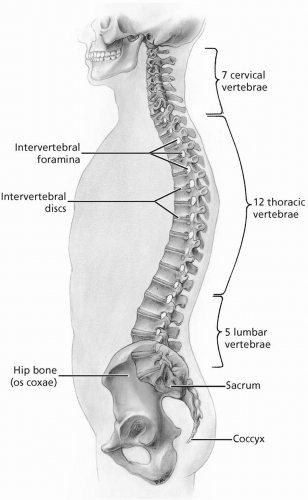
The lumbosacral spine, consisting of the five lumbar vertebrae, the sacrum, and the coccyx, contains the cauda equina (lumbar, sacral, and coccygeal nerve roots) whose branches supply the lower limb, gluteal region, and perineum. This region of the vertebral column also provides mobility for the back and support for the upper body, and transmits the weight of the upper body to the pelvis and the lower limb (
Fig. 21.1.1). The lumbar spine is convex anteriorly, while the sacrum has an anterior concavity. Anatomy of the lumbosacral spine is presented in detail in major anatomic textbooks (
1,
2,
3,
4,
5,
6).
The lumbar vertebrae (L1-L5) are larger and heavier than those in other regions of the vertebral column. The vertebral body is considered massive and displays a kidney shape when viewed superiorly. The body, together with the strong pedicles and laminae that form the neural arch, surrounds the triangle-shaped vertebral foramen. This foramen is larger than in the thoracic spine and smaller than in the cervical region. The laterally projecting transverse processes are long and slender and are situated anterior to the articular processes. The superior articular process has a facet directed posteromedially and a mamillary process on its posterior surface. An anterolaterally directed facet characterizes the inferior articular process. Approximately halfway between the superior and inferior articular process is the pars interarticularis. A bony defect at this location is referred to as a spondylolysis. The spinous processes are short and sturdy and are often referred to as looking “hatchet-shaped.” The interspace between the L4 and L5 spinous processes serves as an excellent reference point from which to identify the other lumbar vertebrae and the sacrum. This interface is situated at the same level as the most superior aspects of the iliac crests.
The large wedge-shaped sacrum is composed of the five fused sacral vertebrae. The sacrum provides stability and strength to the pelvis and transmits the weight of the body to the pelvic girdle and the lower limbs through the sacroiliac joints. The superior surface of the S1 vertebra forms the base of the sacrum. It has superior articular processes whose facets articulate with the facets of the inferior articular processes of the L5 vertebra. The anterior edge of the body of the S1 vertebra is called the sacral promontory. On the pelvic and posterior surfaces of the sacrum are four sacral foramina for the exit of the anterior and posterior primary rami of the first four sacral spinal nerves and accompanying vessels. The pelvic surface of the sacrum is smooth and concave with four transverse ridges indicating the points of fusion of the sacral vertebrae. The posterior surface of the sacrum is rough and convex and has a median sacral crest formed by the fusion of the first three sacral spinous processes. Inferior to the median crest is the sacral hiatus, which results from the absence of the laminae and spinous processes of the S4 and S5 sacral vertebrae. The hiatus leads into the inferior end of the vertebral canal. The sacral cornua (horns) project inferiorly on each side of the sacral hiatus. The lateral surface of the sacrum
presents an articular surface that participates in the formation of the sacroiliac joint. At the inferior end of the lateral surface, at the point where the sacrum tapers toward its apex at the coccyx, is the inferior lateral angle. The coccyx is a remnant of three fused coccygeal vertebrae.
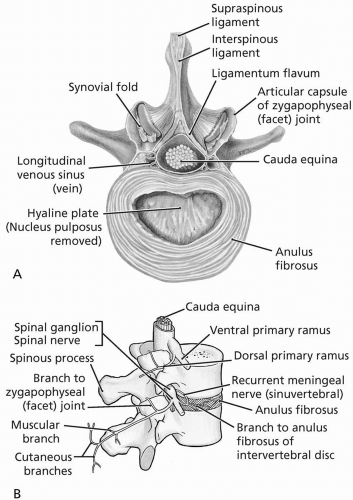
The lumbosacral spine is composed of two types of joints, which work together to provide mobility. These include the facet joints (zygapophyseal joints) and the intervertebral body joints (intervertebral discs). The vertebral bodies and intervertebral discs (anterior segment) are designed for support, weight bearing, and shock absorption. The arch and facet joints (posterior segment) are designed to protect the spinal cord and provide for movement. Branches arising from the posterior primary rami of the spinal nerves innervate these joints.
The intervertebral discs are fibrocartilaginous joints, designed for weight bearing and strength, situated between the bodies of adjacent vertebrae (
Fig. 21.1.2). Each intervertebral disc consists of an outer anulus fibrosus, composed of concentric lamellae of fibrocartilage, which surrounds a gelatinous nucleus pulposus. The anuli insert into the rounded rims on the articular
surfaces of adjacent vertebral bodies. The most inferior functional intervertebral disc is between L5 and the sacrum. In the lumbar region the discs are the thickest, particularly the anterior portions, when compared with those in other regions of the vertebral column. Branches arising from the anterior primary rami of the spinal nerves innervate the intervertebral discs. The intervertebral discs are avascular structures that receive their blood supply by diffusion from the vertebral bodies (
Fig. 21.1.3).
Movements in the lumbar spine consist of lateral bending, flexion, and extension. Extension is most marked in the lumbar region, when compared with other regions of the vertebral column, and is usually more pronounced than flexion in this region of the vertebral column.
Ligaments stabilize the facet joints and intervertebral body joints and support the lumbosacral spine. The anterior longitudinal ligament is a strong, broad fibrous band that covers and connects the anterior aspects of the vertebral bodies and the intervertebral discs. It extends onto the pelvic surface of the sacrum. This ligament maintains stability of the intervertebral body joints and helps to prevent hyperextension of the vertebral column. The posterior longitudinal ligament is narrower and somewhat weaker than the anterior longitudinal ligament. It extends along the posterior aspects of the vertebral bodies inside the vertebral canal. It is attached to the intervertebral discs and the vertebral bodies and extends to the sacrum. This ligament helps to prevent hyperflexion of the vertebral column and posterior protrusion of the intervertebral discs. The laminae of adjacent vertebrae are connected by broad elastic bands called the ligamenta flava. These ligaments help to preserve the normal curvature of the vertebral column and straighten the vertebral column after it has been flexed. Short and strong interspinous ligaments and a strong cordlike supraspinous ligament join adjacent spinous processes. The supraspinous ligament is at its broadest in the lumbar region and can be palpated. The intertransverse ligaments connect adjacent transverse processes and in the lumbar spine they are membranous and more substantial when compared with those in other regions of the vertebral column.
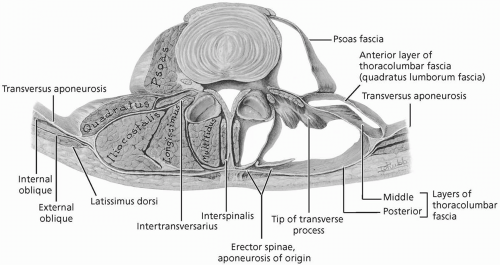
Because most of the body weight is situated anterior to the vertebral column, many strong muscles are attached to the transverse and spinous processes to support the vertebral column. This is particularly true in the lumbosacral
spine. Three groups of muscles are situated in the back: superficial, intermediate, and deep. The superficial and intermediate groups are extrinsic back muscles that control limb movements and respiration, respectively. The most prominent of these extrinsic muscles in the lumbosacral region is the latissimus dorsi, which connects the trunk and pelvis to the upper limb. The deep group of back muscles comprises the intrinsic back muscles that act on the vertebral column to produce movements and control posture. These muscles are enclosed in fascia (thoracolumbar), which in the lumbosacral region is strong and thick and attaches to the tips of the spinous processes, supraspinous ligament, median sacral crest, and transverse processes.
The intrinsic back muscles are divided into three layers: superficial, intermediate, and deep. Muscles in the intermediate and deep layers attach to the lumbosacral spine. The intermediate layer consists of the massive erector spinae, which lies in the trough on each side of the spinous processes and forms a prominent bulge on each side of the midline. The erector spinae is the chief extensor of the vertebral column. Deep to the erector spinae is the deep layer consisting of the transversospinal muscles running obliquely between the transverse and spinous processes. In the lumbosacral spine these muscles include the well-developed multifidus and the rotatores. The multifidus is involved in extension, lateral bending, and rotation while the rotatores act in rotation of the lumbar spine. Branches of the posterior primary rami of the lumbosacral spinal nerves innervate the intrinsic back muscles segmentally.
There are three paired muscles on the posterior abdominal wall that attach to and act on the lumbosacral spine: psoas, iliacus, and quadratus lumborum. The psoas muscle laterally flexes the lumbar spine, is used to balance the trunk when sitting, and when acting with the iliacus, flexes the lumbar spine. The quadratus lumborum extends and is the chief lateral flexor of the lumbar spine. Branches of the anterior primary rami of the L1-L4 spinal nerves innervate these muscles, for the most part. The anterior abdominal wall muscles are key to normal lumbar spine support. Weakness of these muscles results in an abnormal increase in lumbar lordosis and low back pain. These muscles receive segmental innervation from branches of the anterior primary rami of the spinal nerves.
Blood supply to the lumbosacral spine, associated muscles, and nerve roots is derived from four pairs of lumbar arteries and the median sacral artery arising from the posterior aspect of the abdominal aorta. Sometimes the median sacral artery gives off a fifth pair of lumbar arteries. Each lumbar artery gives off a posterior branch that turns posteriorly to supply the musculature of the back and overlying skin and, in turn, gives off a spinal branch to the vertebral column, nerve roots, and meningeal coverings. An anterior branch runs deep to the psoas and quadratus lumborum muscles and supplies the anterolateral abdominal wall.
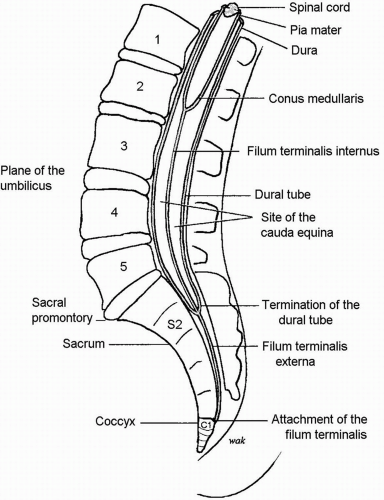
The spinal cord and its coverings (meninges) are located in the vertebral canal. In the adult lumbar spine the spinal cord, containing L5, sacral (
5) and coccygeal (
1) segments, usually terminates at the level of the intervertebral disc between the L1 and L2 vertebrae. From this point to the S2 segment of the sacrum, the vertebral canal of the lumbosacral spine contains the dural sac, underlying arachnoid mater, and
the cauda equina bathed in the cerebrospinal fluid of the lumbar cistern (
Fig. 21.1.4). The cauda equina are dorsal and ventral roots arising from lumbar, sacral, and coccygeal spinal cord segments which are descending to exit the vertebral column through the appropriate intervertebral foramina and form spinal nerves. The dura mater extends into the intervertebral foramina as dural root (meningeal) sleeves covering the dorsal and ventral roots and ends by blending with the epineurium of the spinal nerve. The inferior end of the spinal cord is called the conus medullaris. From the conus medullaris, a slender strand of pia mater, the filum terminalis, descends among the nerve roots of the cauda equina. At the level of S2 the filum acquires a layer of dura mater as it leaves the inferior end of the dural sac and becomes the coccygeal ligament. This ligament passes through the sacral hiatus and attaches to the coccyx. Each spinal nerve is formed immediately outside the intervertebral foramen and divides almost immediately into an anterior and posterior primary ramus. The posterior primary rami segmentally supply skin and muscles of the back and skin over the gluteal region. Anterior primary rami (L2-S3) form the lumbosacral plexus, which innervates the lower limb, gluteal region, and the perineum. The lumbar portion of the lumbosacral plexus (L2-L4) is formed within the psoas muscle. Emerging from this muscle laterally is the femoral nerve, which descends deep to the inguinal ligament to enter the anterior thigh. Emerging from the psoas muscle medially is the obturator nerve, which courses forward on the lateral pelvic wall and enters the medial thigh through the obturator foramen. A portion of the L4 anterior primary ramus along with the L5 anterior primary ramus forms the lumbosacral trunk, which descends into the pelvis and joins the sacral portion of the lumbosacral plexus. The sacral portion of the lumbosacral plexus (L4-S3) arises from the anterior primary rami of the S1-S3 spinal nerves, which emerge from the pelvic sacral foramina and join the lumbosacral trunk on the posterior wall of the pelvis anterior to the piriformis muscle. The large sciatic nerve leaves the lumbosacral plexus through the greater sciatic foramen, inferior to the piriformis muscle, enters the gluteal region, and descends into the posterior thigh. In the gluteal region the sciatic nerve is located halfway between the greater trochanter of the femur and the ischial tuberosity. In addition to the three major branches, there are several small lumbar and sacral branches given off by the lumbosacral plexus; they supply skin and muscle in the lower limb, gluteal region, and the perineum.
REFERENCES
1. Basmajian JV, Slonecker CE. Grant’s Method of Anatomy, 11th ed. Baltimore: Williams & Wilkins, 1989.
2. Clemente CD. Gray’s Anatomy of the Human Body, American 30th ed. Philadelphia: Lea & Febiger, 1985.
3. Moore KL, Agur AM. Essential Clinical Anatomy. Baltimore: Williams & Wilkins, 1996.
4. Rosse C, Gaddum-Rosse P. Hollinshead’s Textbook of Anatomy, 5th ed. Philadelphia: Lippincott-Raven, 1997.
5. Williams PL, Warwick R, Dyson M, Bannister LH. Gray’s Anatomy, British 37th ed. London: Churchill Livingstone, 1989.
6. Woodburne RT, Burkel WE. Essentials of Human Anatomy, 9th ed. New York: Oxford University Press, 1994.
21.2 Physical Examination
Michael A. Campbell
Charles W. Webb
Lumbosacral pain can have many sources and etiology (
1,
2). The physical examination works with the history to narrow down the differential diagnoses, so both must be done comprehensively. The history and physical should be thorough to avoid missing a grave diagnosis.
OBSERVATION
The athlete should be standing as the examiner first evaluates posture. This should be examined from the anterior, posterior, and lateral positions to observe any asymmetry or gross deformity. An imaginary line is placed through the midline of the body. From the anterior view, the line should run from the nose, through the sternum, umbilicus, and genitalia. Posteriorly, the spine should serve as the imaginary line. Laterally, the imaginary line extends from the external auditory canal over the greater trochanter to the lateral malleolus. Note any flattening or exaggeration of lumbar lordosis as well as scoliotic curvatures. Excessive stooping or leaning to a particular side could signal an acute process. Uneven innominate heights could suggest a possible leg-length discrepancy or a contralateral lumbar dysfunction. Always look at the knees and feet for the presence of misalignments such as pes planus or cavus, and genu varum or valgum.
Measure symmetry by placing the fingertips on the acromia, anterior superior iliac spines (ASIS), posterior superior iliac spines (PSIS), gluteal folds, patella, and lateral malleoli, and note which ones are higher (
Fig. 21.2.1). This is incorporated in the overall musculoskeletal examination, but it is pertinent for the lumbar spine.
GAIT
Gait observation can yield a wealth of information. The analysis should be conducted with a barefoot athlete walking on a flat surface. The examiner should be looking for alterations such as a footdrop, lack of a push-off, restricted hip extension, or overpronation. Observe the motion in the lumbosacral region as the athlete walks. Note any restriction in motion, in particular, the sacroiliac joints and the lumbosacral junction. More information can be found in
Chapter 25 on gait analysis.
RANGE OF MOTION
Gross range of motion has nearly as much variability as there are personalities. Despite these vast differences in athletes, knowing the normal ranges of motion aids in identifying the source of the problem and later aids the clinician in checking the response to treatment (
3).
Assessment of gross motion of the lumbosacral spine is performed with the athlete standing. Make sure the flexion is coming from the lumbar spine and not in the pelvis, knees, or thoracic spine. The range of active motion for the lumbar spine is 40 to 60 degrees for forward flexion, 20 to 35 degrees for extension, 15 to 20 degrees for side bending, and 3 to 18 degrees for rotation (
4).
Lumbar flexion can be restricted but appear to be normal due to compensatory mechanisms. The examiner should see the normal lordotic curve of the lumbar spine disappear as the athlete flexes. He or she can further confirm true lumbar flexion by placing one thumb on
the spinous process of L1 and the other on the base of the sacrum, and then see if the thumbs separate (
Fig. 21.2.2). The same technique applies to the other planes of motion.
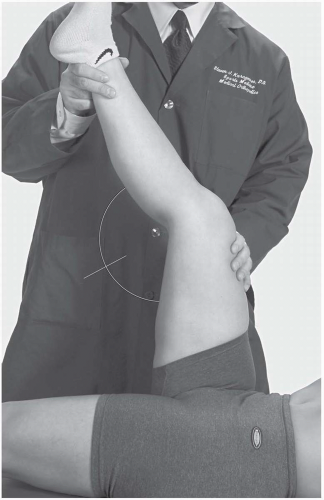
Hamstring flexibility should always be assessed during every athletic lumbosacral examination. With their origin on the pelvis, the hamstrings are a direct link between the lower extremity and pelvis as well as a primary propulsive force in the gait cycle. Hamstrings with reduced flexibility create an abnormal vector force on the ipsilateral innominate bone, resulting in a tendency toward posterior rotation. This has a direct effect on the sacroiliac joint and the lumbar musculature connected to the pelvis (quadratus lumborum, erector spinae).
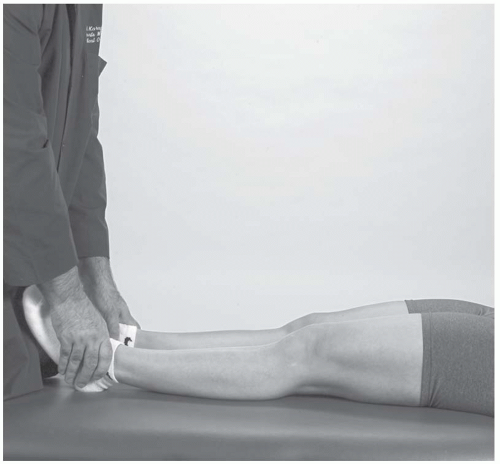
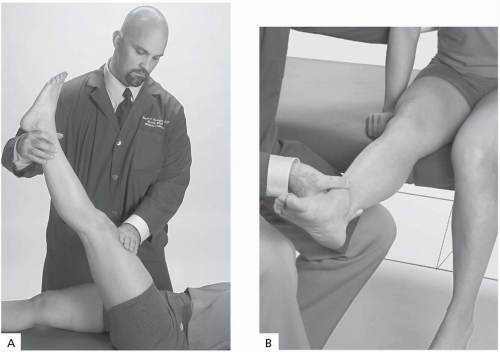
The popliteal angle is an objective way to measure hamstring flexibility (
4). With the athlete supine, the examiner flexes the hip to 90 degrees. The examiner then passively extends the leg to the physiologic barrier. The angle formed at the knee is the popliteal angle (
Fig. 21.2.3). The normal range is 120 to 180 degrees, depending on the athlete’s age, sex, fitness, and genetics.
The symmetry of motion is just as important as its range. If an athlete is able to side-bend the lumbosacral spine 20 degrees to the right and only 10 degrees to the left, this may indicate focal dysfunction and restriction, which can lead to breakdown along the kinetic chain. The examiner can more closely assess symmetry by comparing the range of a vertebral segment on both the involved and uninvolved sides.
PALPATION
Using the TART system (
tissue texture changes;
asymmetry of landmarks;
restriction of motion;
tenderness to palpation), the examiner should
begin by excluding nonmusculoskeletal ailments (
6,
7,
8). Palpating the costoverterbral angles and suprapubic region for tenderness can help exclude infections of the genitourinary tract. Percussion of the spinous processes helps to exclude infections of the vertebrae or discs, such as discitis or osteomyelitis. Palpate the abdomen to look for an aortic aneurysm, pancreatitis, or cholecystitis.
Palpating the tissue gives the examiner a feel for the turgor and tone of the tissue. Regions with increased turgor and tone often have tender points. By palpating these tender points, the examiner can assess the severity of strain patterns and dysfunctions. The fascia can thicken or scar over time, restricting its motion. To palpate the fascia, the examiner puts just enough pressure on the skin so that the fingers can glide the subcutaneous tissue over the smooth fascial surface. The glide should be smooth and nontender; any findings to the contrary should be noted and investigated.
Palpatory findings typically confirm the acute or chronic processes elicited in the history. Acute processes generally have a warm, boggy feel with focal tender points. The tender points in acute processes are usually sharp and severe. In contrast, chronic tender points are firmer, cooler, and more diffuse (
6,
7).
After assessing the superficial tissue, the examination proceeds beneath the muscle and fascia to the lumbar vertebrae, sacrum, and ligaments. The examiner presses the transverse vertebrae and assesses the ease of motion with right and left rotation. A dysfunction is named for the anterior body of the vertebra in relation to the vertebra inferior and in the direction of ease to which a vertebra moves (
7). For example, if L4 rotates to the right more easily (pressing down on the left transverse vertebra) than to the left, it is described as being rotated right.
By palpating the spinous processes of the individual vertebrae, the examiner can identify such conditions as spina bifida occulta or spondylolisthesis, in which the involved spinous process lies more anterior than the remaining vertebrae and spinous processes. Tenderness on the interspinous ligaments may indicate sprain or significant dysfunction. A tender spinous process requires radiographic evaluation, which can demonstrate spina bifida and spondylolisthesis.
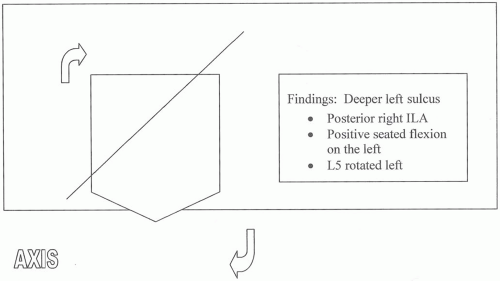
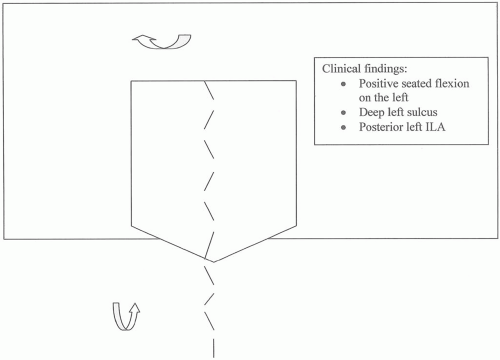
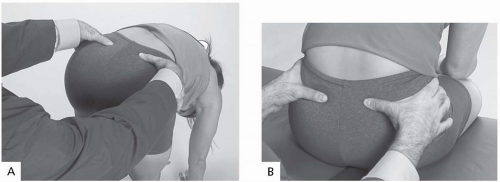
The sacrum is the junction between the lumbar spine and pelvis, and its position makes it a common source of dysfunction. Palpate the sacral sulci formed bilaterally with the junction with L5 and note how shallow or deep they are (
Fig. 21.2.4). Label the sulcus based on whatever side is dysfunctional. For example, if the seated flexion test is positive on the right and the left sulcus is shallower than the right, one would say “deep right sulcus” rather than “shallow left sulcus.” Palpate the inferior lateral angles (ILAs) and note which is more posterior and/or inferior (
Fig. 21.2.5). Examine the sacroiliac joints, both superior and inferior poles, and note any tenderness or loss of joint play or spring.
Always palpate the posterior superior iliac spines (PSIS) when checking the sacral sulci. Often, pain from this articulation between the iliac crest and sacrum mimics lumbar radiculopathy and can be treated quickly.
Dysfunctions of the sacrum can also lead to dysfunctions of the ligaments and muscles directly connected to the sacrum. The iliolumbar ligament is an extension of the quadratus lumborum and runs from the transverse processes of L4-L5 to the iliac crest and sacroiliac joint. It can be palpated just superior to the PSIS and is deeper than the fascia and muscles (
Fig. 21.2.6).
The sacrotuberous ligament runs from the inferior border of the sacrum to the ischial tuberosity. Palpate inferiorly and laterally from the sacral ILAs (
Fig. 21.2.7).
Palpating the sciatic notch can give some information about the piriformis, particularly an acute piriformis syndrome, but this maneuver is not necessarily sensitive for piriformis dysfunction because the sciatic nerve may be irritated independently and tender to palpation.
The relationship between L5 and the sacrum can be assessed. Sacral torsion describes a sacrum that is rotated on an oblique axis and in the opposite direction of L5 (
Fig. 21.2.8). This is the opposite motion of L5 relative to the sacrum and causes the torsion (
6).
Generally, an L5 dysfunction leads to a sacral dysfunction, so the examiner should look closely at this segment. Three common rules apply (
5):
The sacral axis is the same as the side bending of L5.
L5 and the sacrum rotate in opposite directions.
There is decreased motion of the sacroiliac joint at the side opposite the axis.
Another common sacral dysfunction is the sacral shear. A sacral shear occurs when the sacrum rotates anteriorly or posteriorly within the sacroiliac joint on a transverse axis (
6). Shears are the result of two opposing forces at the sacroiliac joint (
7), and are described as being in flexion or extension. Sacral shears can be the result of stepping unexpectedly off a curb or hole, falling on the sacral area, or a short leg (
7). Often unilateral flexion or extension of the sacrum is demonstrated (
Fig. 21.2.9).
A proficient way to distinguish shears and torsions is to look at the side of the positive seated flexion test. In shears as well as torsions, the sacral base on the dysfunctional side is shallow (shallow sulcus) or deep; the difference between the two is the palpatory findings of the inferior lateral angles (ILAs) of the sacrum. In torsions, one can palpate an ILA that is more anterior or posterior
opposite the side of the
positive seated flexion test. With a sacral shear, the examiner places his or her thumbs on the ILAs and notices an abnormality on the
ipsilateral side.
Table 21.2.1 lists the various findings for sacral torsions and sacral shears.
After assessing the relationship between L5 and the sacrum, the evaluation needs to exclude any rotational component of the pelvis. Palpating the PSIS and ASIS and noting their level and relation to the midline can aid in assessing for any rotational component of the innominates. For example, an inferior right ASIS, superior PSIS, and pain over the SI joint could simply be the result of the right innominate rotated anteriorly.
LEG-LENGTH DISCREPANCY
Although the research does not completely support the correlation between a short leg and lumbar pain (
3), most practitioners agree that a short leg can have an effect in such problems as gait and running mechanics and economy, standing posture, postural sway, as well as increased incidence of scoliosis, low back pain, osteoarthritis of the hip and spine, aseptic loosening of a hip prosthesis, and lower extremity stress fractures (
10). The lumbosacral examination should include a leg-length evaluation.
To check for leg-length discrepancy, do the following:
The athlete lies supine on the table with the knees and hips flexed while the clinician holds the ankles.
The athlete sets the hips down while the clinician pulls down on the legs to take up any slack.
The clinician places the thumbs under the medial malleoli and compares for evenness.
The difficulty with the leg-length discrepancy test is the intrusion of factors that can skew results, such as innominate shears and rotations, sacral torsions, and asymmetrical pes planus, particularly in cases of plantar fascia or posterior tibialis insufficiency. A more precise but time-consuming method is as follows:
This method takes into account the compensatory mechanisms the body uses to cope with a structural inequity. It is important to recheck the athlete after any inserted heel lift to see the body’s response. In particular, there should be symmetry between the PSIS and ASIS landmarks, and the standing and seated flexion tests should be improved, if not negative, when the proper heel lift is finally inserted. Follow-up radiographs with the heel lift in place are not necessary, but may be helpful. The best candidate for heel lift correction is an athlete with a leg-length inequity who has lumbosacral dysfunction and pain that resolves with realignment.
INTERSEGMENTAL VERTEBRAL MOTION
One of the crucial elements in making the correct diagnosis in lumbosacral dysfunction is the assessment of the motion of the individual segments relative to each other. The history typically specifies the dysfunction to the lumbosacral spine, but it is the examiner’s challenge to find which specific dysfunctions have led the athlete into the office.
To evaluate intersegmental motion, the examiner places the pads of the thumb on the pillars just lateral to the spinous process and notes which one is more posterior. The athlete flexes and extends the lumbar spine while the examiner monitors for change. The side that protrudes more posteriorly is the dysfunctional facet. If the facet is provoked in flexion, the lesion is restricted in that direction and positionally stuck in the opposite side, and it will get worse in the direction opposite the facet position.
Type I group dysfunctions have no flexion or extension component; rotation and side bending are opposite each other, which contrasts with type II segmental dysfunctions. The apex of the curve should be identified and targeted in treatment.
NEUROVASCULAR EXAMINATION
Sensory testing should focus on the L4-S1 nerve roots where most disc herniations occur (
8,
11). The reflexes for these locations are patellar (L4) and Achilles (S1). There is no reliable reflex for the L5 nerve root (
3). A summary of the dermatomes, reflexes, and myotomes is found in
Table 21.2.2.
Strength testing is quick, but gives invaluable information. Leg extension evaluates L4, while dorsiflexion of the extensor hallucis longus
and plantarflexion of the foot evaluate L5 and S1, respectively. Light touch of the medial (L4), dorsal (L5), and lateral (S1) aspects of the foot assesses the dermatomes (
4,
5). Any asymmetry or abnormality in these regions should be noted and fully evaluated.
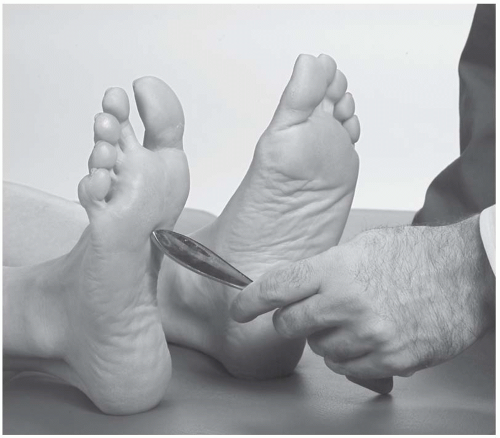
Babinski’s Sign. The examiner takes a sharp object such as a key or the handle of a reflex hammer and rubs it along the lateral aspect of the athlete’s foot, crossing over to the skin overlying the metatarsophalangeal joints (
Fig. 21.2.11).
Positive test: The extensor hallucis longus reflexively dorsiflexes instead of plantarflexes.
Indicates: Upper motor neuron lesion, potentially by herniation.
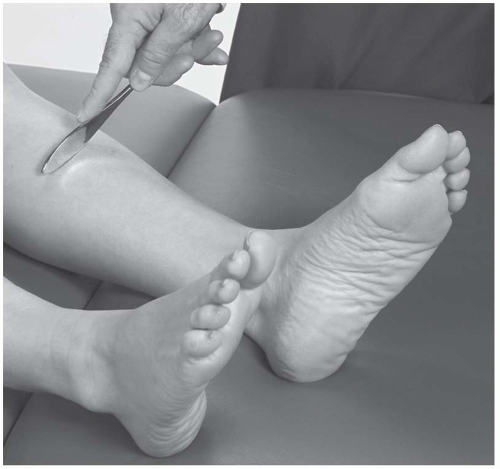
Oppenheimer’s Sign. The examiner takes a blunt object and slides it down the medial aspect of the athlete’s lower leg (
Fig. 21.2.12).
Positive test: The extensor hallucis longus reflexively dorsiflexes instead of plantarflexes.
Indicates: Upper motor neuron lesion, potentially by herniation.
PROVOCATIVE TESTS AND MANEUVERS
Squatting Test. This is a gross function test that can be done at the beginning of the examination to localize the source of pain. The athlete stands facing the examiner and performs a full squat down to maximal knee and hip flexion (
12).
Positive test: Pain produced by squatting localized in the lumbosacral spine, hips, or knee.
Indicates: Pathology in the spine, hip, or knee, depending on the location of the pain.
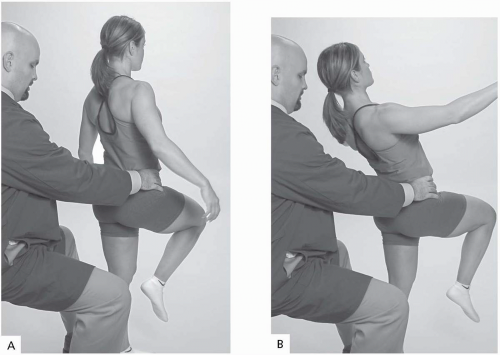
Stork Sign. This provocative test assesses the posterior spine. The athlete stands in front of the examiner, and then lifts one foot off the ground. The athlete then extends the back and reports on any provoked pain (
Fig. 21.2.13A, B) (
4,
5).
Positive test: Pain produced by lumbar extension.
Indicates: Spondylolysis and/or spondylolisthesis of the lumbar pars interarticularis.
The knee lift typically provokes pain in such pathology. Unilateral injuries are usually located on the ipsilateral side of the flexed hip.
Standing Flexion Test. With the athlete standing, the examiner places his or her thumbs over the PSIS joints and asks the athlete to bend forward, which flexes the lumbar spine (
Fig. 21.2.14A).
Positive test: Asymmetrical rise of one thumb above the other (
6,
7).
Indicates: Gross restriction at the sacroiliac joint, either intrinsically in the joint or from extrinsic factors, such as hamstring restriction.
Seated Flexion Test. With the athlete sitting and the feet flat on the floor or stool, the examiner places his or her thumbs over the PSIS joints and asks the athlete to bend forward, which flexes the lumbar spine (
Fig. 21.2.14B).
Positive test: Asymmetrical rise of one thumb above the other.
Indicates: Restricted sacroiliac joint on the positive side. The seated flexion test isolates the sacroiliac joint by anchoring the ischial tuberosities to the table and taking out any hip flexion. This also removes the hamstrings from the equation, so that tightness does not affect the test result, as opposed to the standing flexion test, which looks at gross hip restriction.
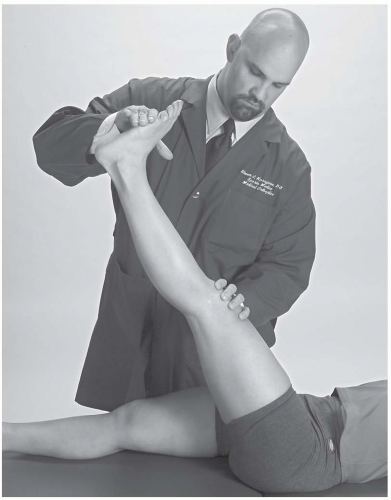
Straight Leg Raising Test. With the athlete supine and seated, the examiner raises the extended leg off the table, which stretches the sciatic nerve in normal athletes without herniation (
Fig. 21.2.15A).
Positive test: Pain starting at the lumbar region that radiates below the knee on the ipsilateral side.
Indicates: Disc herniation, which impinges on the nerve root. The pain elicited by nerve root impingement is between 30 and 60 degrees, and flexion of the knee relieves the pain (
1,
8).
Variation 1. Crossed leg raising test.
Positive test: Pain elicited in the contralateral extremity.
Variation 2. Bench (seated straight leg) test: The athlete is sitting and the examiner extends the leg up to tension (
Fig. 21.2.15B).
Positive test: Pain elicited in the ipsilateral hip and leg.
Lasègue’s Sign. The examiner lifts the athlete’s extended leg off the table to the point of pain. The examiner then lowers the leg just below the level of pain and adds dorsiflexion of the ankle, which stretches the sciatic nerve (
Fig. 21.2.16).
Positive test: Stretching leads to pain radiating below the knee (
13).
Indicates: Disc herniation, neural impingement
Hip Provocative Tests
This aids in narrowing the differential diagnoses down by attempting to provoke the symptoms from the hip.
Indicates: Dysfunction of the iliopsoas, rectus femoris, teasor fascia lata (TFL), or iliotibial band.
Patrick’s (FABER [Flexion, Abduction, External Rotation]) Test. See
Chapter 22.2, Hip and Pelvis Examination (
Fig. 22.2.7).
Positive test: Pain elicited posteriorly or anteriorly in the hip (
1,
3).
Indicates: Anterior groin pain suggests hip joint pathology, while posterior pain suggests sacroiliac joint pathology.
PSYCHOGENIC PAIN
Pain of psychogenic origin is one of the possible causes for low back complaints and one of the most difficult causes to eliminate. In 1980, Waddell found five nonorganic signs to be clinically useful in differentiating between organic and nonorganic causes of low back pain (
Table 21.2.3) (
14). Waddell concluded that three or more positive signs are clinically significant, and the patient should be considered for further psychological testing (
14). Superficial, nonanatomic tenderness describes the finding of the skin being tender over a wide area of the lumbar region and often extends to other parts of the back.


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access