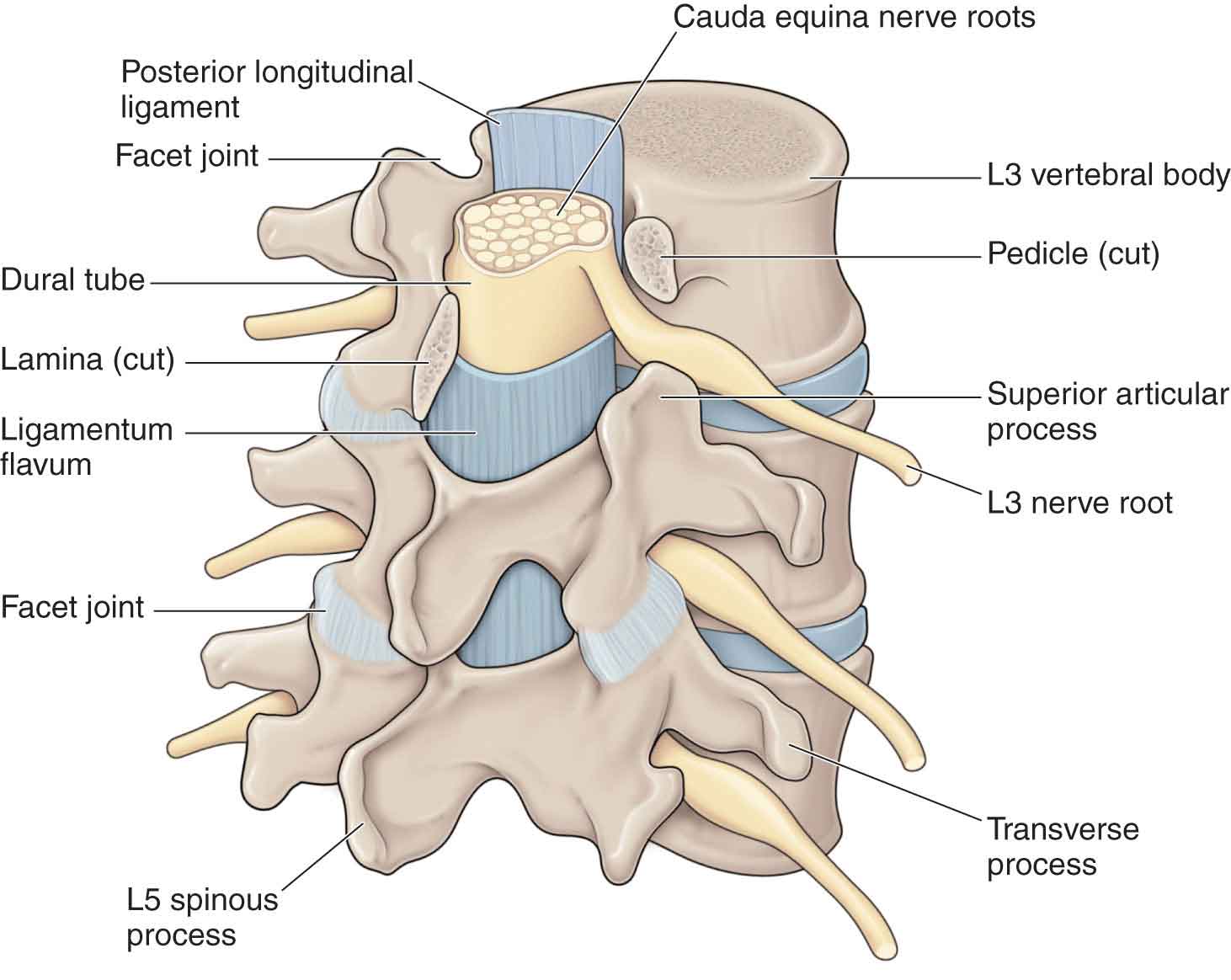
Over the past few decades, low-back pain (LBP) has become increasingly problematic, placing significant burdens on health systems and social-care systems.1,2 Indeed, LBP is one of the most common disorders encountered by physical therapists.3 The clinical course of LBP can be described as acute, subacute, recurrent, or chronic. The first episode of back pain can have differing results: 80–90% will be asymptomatic in 6 weeks, 98% in 24 weeks, and 99% in 52 weeks,4 leading to the assumption that most cases of LBP are benign in nature.5–7 However, the small percentage of people who do become disabled with chronic LBP account for 75–90% of the cost associated with LBP.8 In addition, this population has been associated with a reduced quality of life, poor health, comorbidities, and high medical costs.9,10 A number of risk factors have been associated with LBP. However, current literature does not support a definitive cause for the initial episode of LBP.11 The lumbar spine (Fig. 28-1) consists of five lumbar vertebrae, which, in general, increase in size from L1 to L5 to accommodate progressively increasing loads. Between each of the lumbar vertebrae are the intervertebral disks (IVDs). FIGURE 28-1 Structures of the lumbar spine. The anterior part of each vertebra is called the vertebral body. The pedicles, which project from the posterior aspect of the vertebral body, represent the only connection between the posterior joints of the segment and the vertebral bodies, both of which deliver tensile and bending forces. Noticeably, the muscles that act on a lumbar vertebra pull downward, transmitting the muscular action to the vertebral body. This muscular action is borne through the pedicles, which act as levers, and thus are subjected to a certain amount of bending.12 If the vertebral body slides forward, the inferior articular processes of that vertebra abut against the superior articular processes of the next lower vertebra and resist the slide.12 These resistive forces are transmitted to the vertebral body along the pedicles. The lamina (see Fig. 28-1) functions to absorb the various forces that are transmitted from the spinous and articular processes. The pars interarticularis connects the vertically oriented lamina and the horizontally extending pedicle, which exposes it to appreciable bending forces.12 The two laminae meet and fuse with one another, forming an arch of bone aptly called the vertebral, or neural arch, which serves as a bony tunnel for the spinal cord. Both the transverse and the spinous processes of the vertebral body provide areas for muscle attachments. The first sacral segment, the point at which the sacrum joins the lumbar spine, is usually included in discussions of the lumbar spine. In most cases, this is a fixed segment but, in some cases it may be mobile (lumbarization of S1). At other times, the fifth lumbar segment may be fused to the sacrum or ilium, resulting in a sacralization of that vertebra. It is unclear how these anomalies affect the biomechanics of the spine. In the lumbar spine, the superior and inferior surfaces of the vertebral bodies are comparatively large and flat, reflecting their load-transfer function. The lumbar disk is approximately cylindrical, its shape being determined by the integrity of the annulus fibrosus (AF). The AF consists of approximately 10–12 (often as many as 15–25) concentric sheets of predominantly type I collagen tissue,13 bound together by proteoglycan gel.14 The number of annular layers decreases with age, but there is a gradual thickening of the remaining layers.15 The fibers of the AF are oriented at approximately 65 degrees from vertical. The fibers of each successive sheet or lamella maintain the same inclination of 65 degrees, but in the opposite direction to the preceding lamella, resulting in every second sheet having the same orientation. Thus, only 50% of the fibers are under stress with rotational forces at any given time. This alteration in the direction of fibers in each lamella is vital in enabling the disk to resist torsional (twisting) forces.16 Although each lamella is thicker anteriorly than posteriorly, the lumbar disks are thinner and more tightly packed, posteriorly than anteriorly.17 Consequently, the posterior part of the annulus will have thinner but stronger fibers, and it is capable of withstanding tension applied to this area during flexion activities and postures, which occur more frequently than with extension.12 However, because of the predominance of flexion activities in life, fatigue damage may occur in the posterior aspect of the disk, making it a common site of injury.18 The wedge-shaped appearance of the disk produced by the configuration of the lamellae contributes to the normal lordosis of this region.18 The outermost lamellae insert into the ring apophysis of the upper and lower vertebrae by mingling with the periosteal fibers (fibers of Sharpey). These fibers, attaching them to the bone, may be considered as ligaments and as such are designed primarily to limit motion between adjacent vertebrae.19 The inner portions of the lamellae are attached to the superior and inferior cartilaginous end plates, and form an envelope around the NP.12 The lumbar IVDs of a healthy young adult contain a nucleus pulposus (NP) that is composed of a semifluid mass of mucoid material. This material is clear, firm, and gelatinous.12
CHAPTER 28
Lumbar Spine
OVERVIEW
ANATOMY
VERTEBRAL BODY
Intervertebral Disk
Annulus Fibrosus
Nucleus Pulposus
At birth, the water content of the NP is approximately 80%. In the elderly, the water content is approximately 68%. Most of this water content change occurs in childhood and adolescence, with only approximately 6% occurring in adulthood.20 The portion of the NP that is not water is made up of cells that are largely chondrocytes and a matrix consisting of proteoglycans, collagen fibers, other noncollagenous proteins, and elastin.18,21,22
With the exception of early youth, there is no clear boundary between the NP and AF, and it resembles a transitional zone.23 The biomechanical makeup of the NP is similar to that of the AF, except that the NP contains mostly type II collagen, as opposed to type I.13 The collagen interacts with the ground substance to form a concentration proportional to the viscoelastic requirements of the AF.
An unequal load distribution to the IVD is a major predisposing factor in radial tearing of the AF.28 The tearing can be caused by the torsional effect of the superior vertebra rotating in a constant direction with sagittal movements. The posterolateral aspect of the AF tends to weaken first.29 If the inner layers of the posterior AF tear in the presence of the NP that is still capable of bulging into the space left by the tear, the symptoms of disk disease are likely to be experienced, with the spinal canal location of disk trespass determining the type of neural compromise, clinical pain pattern, and often the outcome.29 It must be remembered that the degree of neural compromise and potential for pain cannot be judged accurately by the size or type of disk material. Large, free fragments can often cause no neurologic deficit or pain.30
Vertebral End Plates
Each vertebral end plate consists of a layer of hyaline and fibrocartilage approximately 0.6–1-mm thick,31 which covers the top or bottom aspects of the disk and separates the disk from the adjacent vertebral body. Peripherally, the end plate is surrounded by the ring apophysis.12
At birth, the end plate is part of the vertebral body growth plate, but by approximately the 20th year, it has been separated from the body by a subchondral plate. During this time, the plate is bilaminar, with a growth zone and an articular area.32 With aging, the growth zone becomes thinner and disappears, leaving only a thickened articular plate.
Nutrition of the disk comes via a diffusion of nutrients from the anastomosis over the AF and from the arterial plexi underlying the end plate. Although almost the entire AF is permeable to nutrients, only the center portions of the end plate are permeable. Over approximately 10% of the surface of the end plate, the subchondral bone of the centrum is deficient. At these points, the bone marrow is in direct contact with the end plate, thereby augmenting the nutrition of the disk and end plate.33 It is possible that a mechanical pump action produced by spine motion could aid with the diffusion of the nutrients.
The two end plates of each disk, therefore, cover the NP in its entirety but fail to cover the entire extent of the AF.
Between the ages of 20 and 65 years, the end plate thins and the vascular foramina in the subchondral bone become occluded, resulting in decreased nutrition to the disk. At the same time, the underlying bone becomes weaker, and the end plate gradually bows into the vertebral body, becoming more vulnerable centrally, where it may fracture into the centrum.12 The presence of damage to a vertebral body end plate reduces the pressure in the NP of the adjacent disk by up to 57%, and doubles the size of the so-called stress peaks in the posterior aspect of the AF.24
Nerve Root Canal
The nerve root canal is located at the lateral aspect of the spinal canal (Fig. 28-1). The dural sac forms the medial wall of the canal, the internal aspect of the pedicle, and the lateral wall. The posterior border of the nerve root canal is formed by the ligamentum flavum, superior articular process, and lamina. The anterior border of the canal is formed by the vertebral body and IVD.
The nerve root canal can be described according to its location35:
 The entrance zone is medial and anterior to the superior articular process.
The entrance zone is medial and anterior to the superior articular process.
 The middle zone is located under the pars interarticularis of the lamina and below the pedicle.
The middle zone is located under the pars interarticularis of the lamina and below the pedicle.
 The exit zone is the area surrounding the intervertebral foramen.
The exit zone is the area surrounding the intervertebral foramen.
A decrease in the dimension of this canal results in a condition called lateral stenotic syndrome.36
Innervation
The outer half of the IVD, the posterior longitudinal ligament (PLL), and the dura are innervated by the sinuvertebral nerve,37 which is considered to arise from the anterior (ventral) ramus and the sympathetic trunk.38 The nerve endings are simple or complex, are encapsulated and nonencapsulated, and exist as free nerve endings. It has been suggested that apart from a nociceptive function, these nerve endings may also have a proprioceptive function.39,40
Alterations in Disk Structure
Although the lumbar IVD appears destined for tissue regression and destruction, it remains unclear why similar age-related changes remain asymptomatic in one individual yet cause severe LBP in others. The basic changes that influence the responses of the disk to aging appear to be biochemical and may concern the collagen content levels in the NP. Recently, advances in brain and spine imaging have begun to yield encouraging findings of a number of central and peripheral mechanisms thought to be important components of the generation and propagation of LBP.41–43 Among these hypothesized mechanisms is an increase in diffusion of water within various soft tissues of the spine, occurring in response to treatment and movement, which may be linked to pain reduction.43 A recent study found that changes in the diffusion of water within the lumbar IVDs at the L1–2, L2–3, and L5–S1 levels appeared to be related to differences in within-session pain reports following a single treatment of spinal manipulative therapy.43
With aging, there is an increase in the collagen content of both the NP and the AF and a change in the type of collagen present.44 The elastic collagen of the NP becomes more fibrous, whereas the collagen of the AF becomes more elastic.44 Eventually, they come to resemble each other. In addition, the concentration of noncollagenous proteins increases in the NP. The change of the makeup of the collagen alters the biomechanical properties of the disk, making it less resilient, perhaps leading to changes from microtrauma.44
It was traditionally thought that the loss of height that occurs with aging resulted from a loss in the height of the IVD. More recently, it has been demonstrated that between the ages of 20 and 70 years, the disk actually increases its height by approximately 10%, and that the loss of height with age is more likely to be caused by the erosion of the vertebral end plate.45
As the NP becomes more fibrous, its ability to handle compressive loading becomes more compromised, and more weight is taken by the AF, resulting in a separation of the lamellae and the formation of cavities within it.44
Zygapophyseal Joint
The articulations between two consecutive lumbar vertebrae form three joints. One joint is formed between the two vertebral bodies and the IVD. The other two joints are formed by the articulation of the superior articular process of one vertebra and the inferior articular processes of the vertebra above it. These latter joints are known as the zygapophyseal joints.
In the intact lumbar vertebral column, the primary function of the zygapophyseal joint is to protect the motion segment from anterior shear forces, excessive rotation, and flexion.46 Additional functions include
 the production of spinal motions including coupling movements;
the production of spinal motions including coupling movements;
 a minimal restrictor of the physiologic movements of extension and side bending.47
a minimal restrictor of the physiologic movements of extension and side bending.47
From an anteroposterior perspective, the zygapophyseal joints of the lumbar spine appear straight, but when viewed from above, they are seen to be curved into a J or C shape. Their orientation varies both with the level and with the individual subject.48 It is thought that this orientation serves to restrict maximally anterior and rotary movements and that the C-shaped joints do better in preventing anterior displacement than the J-shaped joints, because of the curvature of the joint surfaces.12,49 Both shapes competently prevent rotation. The area of the zygapophyseal joints most involved in resisting anterior shear forces is the anteromedial part of the superior zygapophyseal joint. It is this area that is most vulnerable to fibrillation.12 The tangential splitting and vertical tearing of the cartilage that occur with aging are believed to reflect these forces and appear to be a part of the normal degeneration of the joint.12
A fibrous capsule surrounds the joint on all of its aspects except the anterior aspect, which consists of the ligamentum flavum (LF). Posteriorly, the capsule is reinforced by the deep fibers of the multifidus.53 In lumbar extension, there is a potential for the posterior capsule to become pinched between the apex of the inferior facet and the lamina below. To prevent this, some fibers of the multifidus blend with the posterior capsular fibers and appear to keep the capsule taut.54
Superiorly and inferiorly, the capsule is very loose. Superiorly, it bulges toward the base of the next superior transverse process, whereas, inferiorly, it does so over the back of the lamina. In both the superior and the inferior poles of the joint capsule, there is a very small hole that allows the passage of fat from within the capsule to the extracapsular space.55
Within the zygapophyseal joints, three types of intraarticular meniscoids have been noted12:
- A connective tissue rim
- An adipose tissue pad
- A fibroadipose meniscoid
It is thought that the function of these intraarticular meniscoids is to
 fill the joint cavity;
fill the joint cavity;
 increase the articular surface area without reducing flexibility; and
increase the articular surface area without reducing flexibility; and
 protect the articular surfaces, as they become exposed during extreme flexion and extension.
protect the articular surfaces, as they become exposed during extreme flexion and extension.
These menisci have been inculpated in the cause of some types of LBP when they fail to return to their original position on recovery from a flexion or extension movement and block the joint toward the neutral position.56
Ligaments
Anterior Longitudinal Ligament
The anterior longitudinal ligament (ALL) covers the anterior aspects of the vertebral bodies and IVD (Fig. 28-2). The ALL extends from the sacrum along the anterior aspect of the entire spinal column, becoming thinner as it ascends.57 The ALL is connected only indirectly with the anterior aspect of the IVD by loose areolar tissue.12 Some of the ligament fibers insert directly into the bone or periosteum of the centrum.58 Because of these attachments, and the pull on the bone from the ligament, it is proposed that the anterior aspect of the vertebral body can become the site for osteophytes. The remaining ligament fibers cover two to five segments, attaching to the upper and lower ends of the vertebral body.
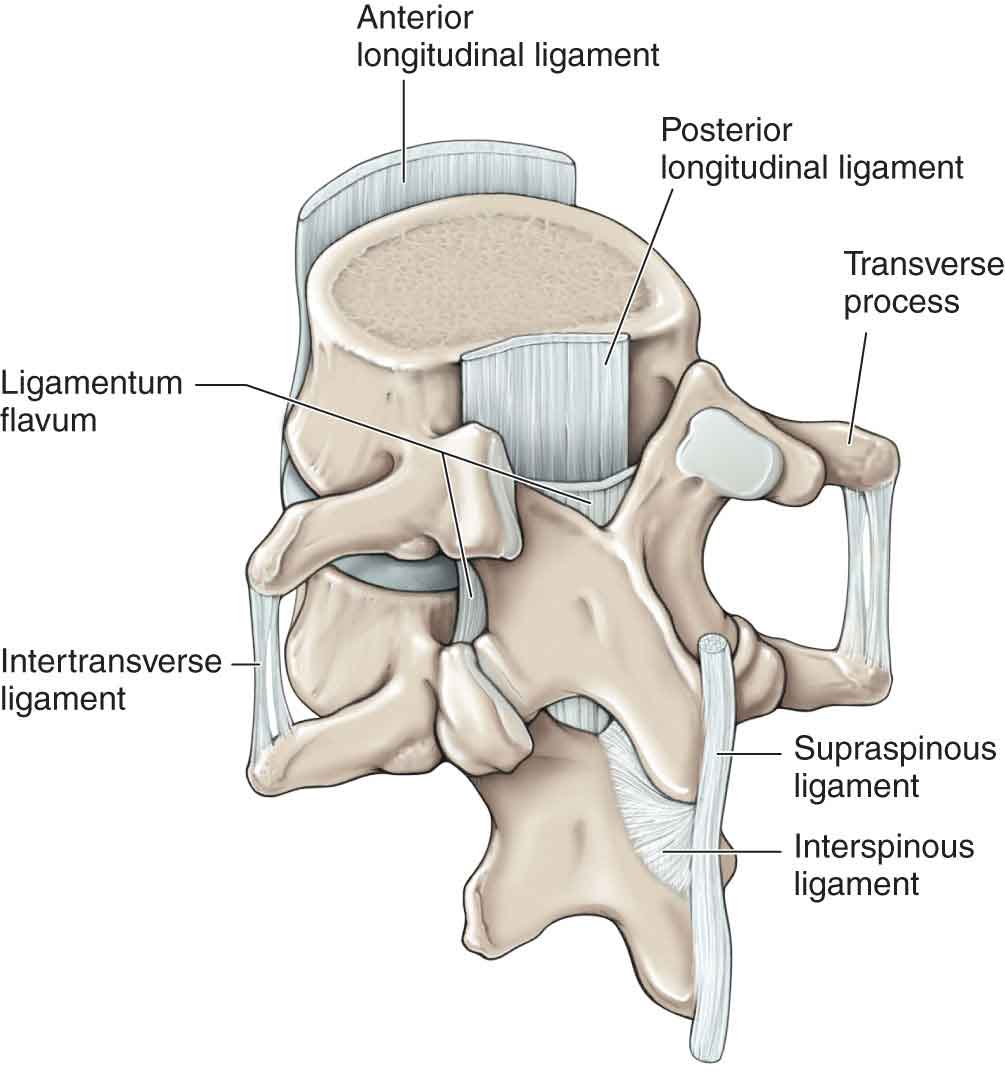
FIGURE 28-2 Ligaments of the lumbar spine. (Reproduced, with permission, from Chapter 1. Back. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The ALL of the lumbar spine is under tension in a neutral position of the spine and functions to prevent overextension of the spinal segments. In addition, the ALL functions as a minor assistant in limiting anterior translation and vertical separation of the vertebral body.
The ALL receives its nerve supply from recurrent branches of the gray rami communicantes.59
Posterior Longitudinal Ligament
The PLL is found throughout the spinal column, where it covers the posterior aspect of the centrum and IVD (see Fig. 28-2). Its deep fibers span two segments, from the superior border of the inferior vertebra to the inferior margin of the superior. These fibers integrate with the superficial annular fibers to attach to the posterior margins of the vertebral bodies.12 The more superficial fibers span up to five segments. In the lumbar spine, the ligament becomes constricted over the vertebral body and widens out over the IVD. It does not attach to the concavity of the body but is separated from it by a fat pad, which acts to block the venous drainage through the basivertebral vein during flexion, as the ligament presses it against the opening of the vein. Although the PLL is rather narrow and is not as substantial as the ALL, it is thought to be important in preventing IVD protrusion.60 Both the ALL and the PLL have the same tensile strength per unit area.61
The PLL tends to tighten in traction and in posterior shearing of the vertebral body. It also acts to limit flexion over a number of segments, although because of its proximity to the center of rotation, it is less of a restraint than the LF.57
The PLL is innervated by the sinuvertebral nerve.
Ligamentum Flavum
The LF connects two consecutive laminae (see Fig. 28-2). This is a bilateral ligament. The medial aspect of the ligament attaches superiorly to the lower anterior surface of the lamina and the inferior surface of the pedicle.62 The LF attaches inferiorly to the back of the lamina and the pedicle of the next inferior vertebra.62
Its lateral portion attaches to the articular process and forms the anterior capsule of the zygapophyseal joint.
The LF is formed primarily from elastin (80%), with the remainder (20%) being collagen.63 Thus, it is an elastic ligament that is stretched during flexion and recovers its neutral length with the neutral position, or extension.
The function of the LF is to resist separation of the lamina during flexion, but there is also appreciable strain in the ligament with side bending.12,64 Although it seems unlikely that the ligament contributes to an extension recovery from flexion, it does appear to prevent the anterior capsule from becoming nipped between the articular margins as it recoils during extension.12 The LF is innervated by the medial branch of the posterior (dorsal) ramus.65
Interspinous Ligament
The interspinous ligament (see Fig. 28-2) lies deeply between two consecutive spinal processes. The ligament is important for stability, as it represents a major structure for the posterior column of the spine. Unlike the longitudinal ligaments, it is not a continuous fibrous band but, instead, consists of loose tissue that fills the gap between the bodies of the spinous processes.12,66 The interspinous ligament is often disrupted in traumatic cases, which results in the posterior column becoming unstable. An extensive anatomic study on the interspinous ligament showed that degenerative changes start as early as the late second decade, with ruptures occurring in more than 20% of the subjects older than 20 years, particularly at L4–5 and L5–S1.67
The ligament has three distinct parts—anterior (ventral), middle, and posterior (dorsal)—of which the middle has the most clinical significance, because it is the part where ruptures tend to occur.66
The interspinous ligament most likely functions to resist separation of the spinous processes during flexion.68 This ligament is supplied by the medial branch of the posterior (dorsal) rami.65
Supraspinous Ligament
The supraspinous ligament (SSL) (see Fig. 28-2) is broad, thick, and cord like, but it is only well developed in the upper lumbar region.12,69 Although it joins the tips of two adjacent spinous processes, the SSL is not considered by some to be a true ligament. This is because part of it is derived from the posterior part of the interspinous ligament, and because it also merges with the insertions of the lumbar posterior (dorsal) muscles.66 Because this ligament is the most superficial of the spinal ligaments and the farthest from the axis of flexion, it has a greater potential for sprains.70 The SSL is supplied by the medial branch of the posterior (dorsal) rami.65
Iliolumbar Ligament
The iliolumbar ligament is one of the three vertebropelvic ligaments, the others being the sacrotuberous and the sacrospinous ligaments. The ligament is variously believed to be a degenerate part of the quadratus lumborum or the iliocostalis and does not fully develop until approximately at the age of 30 years.71
The iliolumbar ligament functions to restrain flexion, extension, axial rotation, and side bending of L5 on S1.72 Motions at the lumbosacral joint increase by approximately 20% in all directions when the ligament is missing or transected.57 The incidences of degenerative instability and isthmic lumbar spondylolisthesis have also been shown to increase in its absence.73,74
Pseudoligaments
These ligaments, the intertransverse, transforaminal, and mamilloaccessory, resemble the membranous part of the fascial system separating paravertebral compartments and do not have any mechanical function.
Intertransverse Ligaments. These ligaments are more membranous than ligamentous. The ligament splits into posterior (dorsal) and anterior (ventral) portions, between which is a fat-filled recess. During flexion and extension movements, the fat can be displaced to accommodate the repositioning of the articular zygapophyseal joint. The main function of the ligament appears to be to compartmentalize the anterior and posterior musculature.12
Transforaminal Ligaments. Occurring in approximately 47% of subjects, the transforaminal ligaments traverse the lateral end of the intervertebral foramen.75 The most significant of these ligaments is the superior corporotransverse ligament. At L5, the fifth lumbar nerve root runs between the ligament and the ala of the sacrum. With marked forward slip and downward descent of L5, or with a loss of IVD height, the corporotransverse ligament can have a guillotine effect on the fifth nerve root, resulting in symptoms that can mimic an IVD herniation or a foraminal occlusion.76
Mamilloaccessory Ligament. This ligament runs from the accessory process of one vertebra to the mammillary process of the same vertebra.77 The ligament forms a tunnel for the medial branch of the posterior (dorsal) ramus, thereby preventing it from lifting off the neural arch. In approximately 10% of adults, the tunnel becomes ossified.77
Muscles
Quadratus Lumborum
The quadratus lumborum muscle is large and rectangular, with fibers that pass medially upward. The fibers attach to
 the anterior inferior surface of the 12th rib;
the anterior inferior surface of the 12th rib;
 the anterior surface of the upper four transverse processes;
the anterior surface of the upper four transverse processes;
 the anterior band of the iliolumbar ligament; and
the anterior band of the iliolumbar ligament; and
 the iliac crest lateral to the attachment of the iliolumbar ligament.
the iliac crest lateral to the attachment of the iliolumbar ligament.
The muscle is active during inspiration, fixing the lowest rib to afford a stable base from which the diaphragm can act. The importance of this muscle from a rehabilitation viewpoint is its contribution as a lumbar spine stabilizer.78 Working unilaterally, it is typically involved with side bending of the lumbar spine, especially with eccentric control of contralateral side bending. The quadratus lumborum is an important, yet often underappreciated, lateral lumbar spine stabilizer that has been shown to be very active in sustained postures and when a heavy weight is held in the opposite hand.79,80 The quadratus lumborum is supplied by the anterior (ventral) rami of T12–L4.81,82
Multifidus
The lumbar multifidus is the largest of the intrinsic back muscles to cross the lumbosacral junction and lies most medially in the spinal gutter (Fig. 28-3).54 It is a fascicular muscle, with each fascicle being layered on another, giving it a laminated appearance.12 The lumbar multifidus originates in three groups, which arise from the same vertebra.
- Laminar fibers arise from the inferoposterior edge of the lamina.
- Basal fibers arise from the base of the spinous process.
- Common tendon fibers arise from a common tendon attached to the inferior tip of the spinous process.
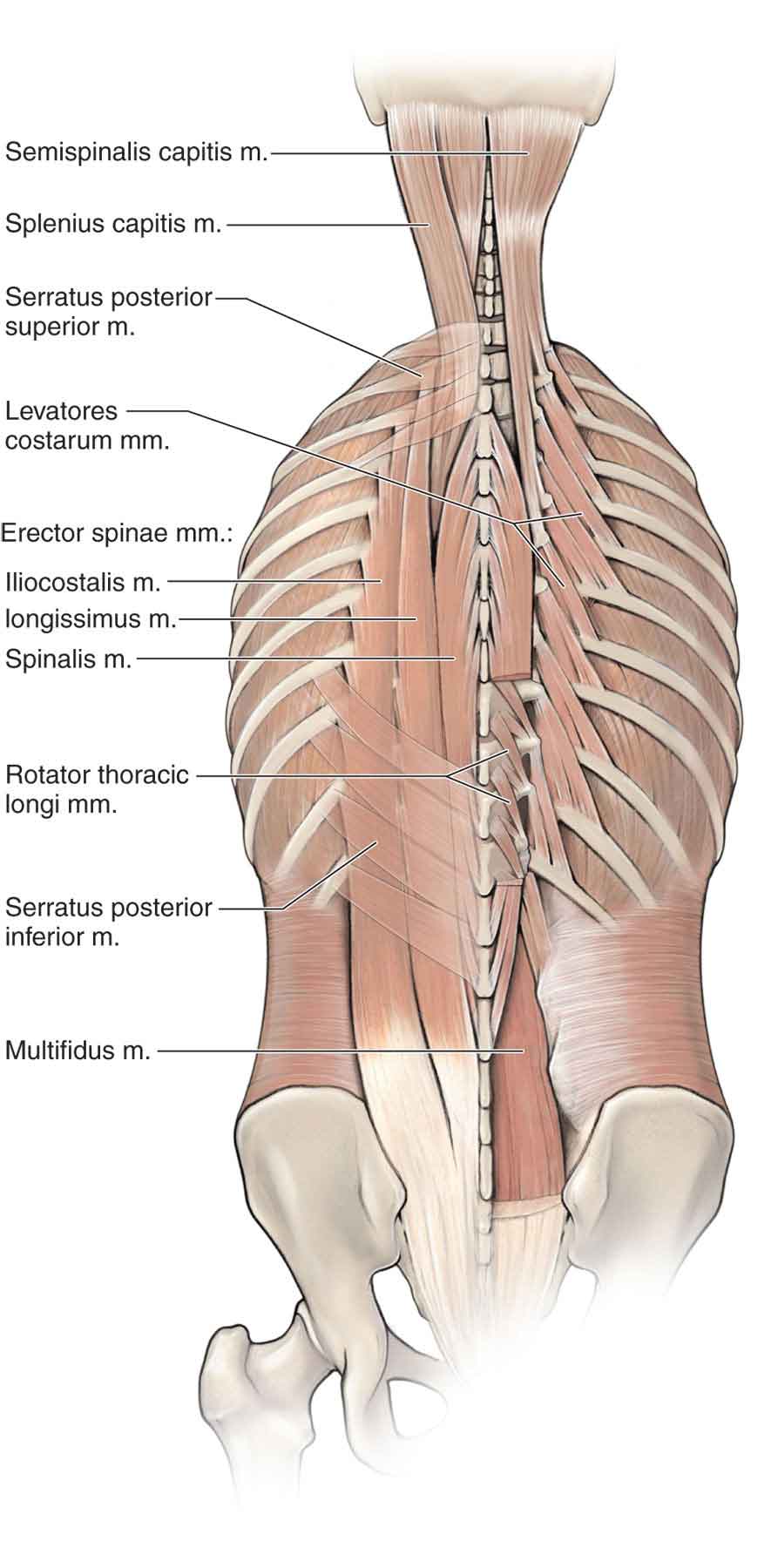
FIGURE 28-3 Multifidus and erector spinae. (Reproduced, with permission, from Chapter 1. Back. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The lumbar multifidus has a complicated insertion (Table 28-1).
TABLE 28-1 | Multifidus Attachments |
Laminar | Basal | Common Tendon |
L1; MP L3 | MP L4 | MP L5, S1, and PSIS |
L2; MP L4 | MP L5 | MP S1 and anterolateral aspect of PSIS |
L3; MP L5 | MP S1 | Inferior to PSIS and lateral sacrum |
L4; MP S1 | As common tendon | Sacrum, lateral to foramina |
L5; common | As common tendon | Sacrum, medial to tendon foramina |
MP, mammillary process; PSIS, posterior-superior iliac spine. Data from Meadows J, Pettman E. Manual Therapy: NAIOMT Level II & III Course Notes. Denver, CO: North American Institute of Manual Therapy, Inc.; 1995; Bogduk N, Twomey LT. Anatomy and biomechanics of the lumbar spine. In: Bogduk N, Twomey LT, eds. Clinical Anatomy of the Lumbar Spine and Sacrum. 3rd ed. Edinburgh: Churchill Livingstone; 1997: 2–53, 81–152, 171–176. | ||
Over the past several decades, there has been much research regarding the lumbar multifidus, with particular reference to its relationship to LBP, and its importance in lumbar spine stabilization. In vitro biomechanical studies have shown that the lumbar multifidus is an important muscle for lumbar segmental stability through its ability to provide segmental stiffness and to control motion.83–85 Wilke et al.86 concluded that the multifidus is responsible for two-thirds of the stiffness of the lumbar spine. The multifidus is active in nearly all antigravity activities and appears to contribute to the stability of the lumbar spine by compressing the vertebrae together.44 Hides et al.87 found reductions in ipsilateral multifidus cross-sectional area in patients with unilateral LBP and speculated that this may be a direct result of reflex inhibition.88 This loss of multifidus cross-sectional area was shown to persist after remission of LBP.82 Isolated multifidus strengthening has been shown to restore the muscle size at the segmental level of the dysfunction.88
MacIntosh and Bogduk54 analyzed the lumbar multifidus to determine the possible actions of the muscle and its individual fibers. The study revealed that when working bilaterally, the multifidus muscles can produce the rocking component of extension, but because of the muscle’s vertical orientation, it cannot produce the accompanying translation.54 In addition, the muscle, by “bow stringing” over a number of segments, can increase the lumbar lordosis, working in a postural role.89
Although not considered a primary lumbar rotator,90 the multifidus is consistently active during both ipsilateral and contralateral spinal rotation, and both multifidi are simultaneously active regardless of which way the spine is turning.54,55The major function of the multifidus from a biomechanical perspective is one of arthrokinematic control. It is believed that the lumbar multifidus acts as an antagonist to flexion and opposes the flexing moment of the abdominals as they rotate the trunk.54,89,91 This synergistic function may be compromised with an injury to the multifidus. Using magnetic resonance imaging (MRI), the signal intensities of the multifidus during lumbar hyperextension have been found to be markedly diminished in patients with chronic LBP compared with normal patients.92
Unilaterally, the multifidus muscle should also be able to produce side bending. However, its horizontal vector is very small, and it is unlikely to be an efficient side bender of the spine.12,54
The multifidus shares a close association with the gluteus maximus and the sacrotuberous ligament, factors that are thought to enhance sacroiliac joint and lumbar spine stability.93–95
The lumbar multifidus has the distinction of being innervated segmentally by the medial branch of the posterior (dorsal) ramus of the same level or the level below the originating spinous process.96,97 Because the multifidus is segmental in origin and innervation, any impairment of this muscle can produce palpable changes in the muscle, thus directing the clinician to the segment that is dysfunctional.98
Erector Spinae
The erector spinae is a composite muscle consisting of the iliocostalis lumborum and the thoracic longissimus (Fig. 28-3). Both of these muscles are subdivided into the lumbar and thoracic longissimi and iliocostallii.12 As a group, the muscles of the erector spinae play an important role in lumbar stabilization by providing compressive forces along the spine that stabilize the spinal curvatures.99 The nerve supply to the erector spinae muscles is by the medial branch of the posterior (dorsal) ramus of the thoracic and lumbar spinal nerves.
Longissimus Thoracis Pars Lumborum. This is a fascicular muscle that arises from the accessory processes of the lumbar vertebrae to insert into the posterior-superior iliac spine (PSIS) and the iliac crest lateral to it. The upper four tendons converge to form the lumbar aponeurosis that inserts laterally to the L5 fascicle.
The longissimus thoracis pars lumborum muscles have both a vertical and a horizontal vector. The vertical vector is much the larger of the two and can produce extension or side bending, depending on whether it is functioning bilaterally or unilaterally.100 Because of its attachment to the transverse rather than the spinous process, which results in reduced leverage, the longissimus thoracis pars lumborum is much less efficient than the lumbar multifidus in producing posterior sagittal rotation.97,101 Indeed, mathematical analysis of the lumbosacral portion of the muscle suggests that the net effect of its pull would be to produce an anterior, and not a posterior, shear.12
Iliocostalis Lumborum Pars Lumborum. There are four overlying fascicles arising from the tip of the upper four transverse processes and the adjoining middle layer of the thoracolumbar fascia (TLF). The fibers insert onto the iliac crest, with the lower and deeper fibers attaching lateral to the PSIS.101
There is no muscular fiber from L5, but it is believed that this is represented by the iliolumbar ligament, which is completely muscular in children, becoming collagenous by approximately 30 years of age.
The vectors and actions of this muscle are similar to those of the longissimus. However, the lower and deeper fibers produce strong axial rotation and act with the multifidus as synergists to produce rotation during abdominal muscle action.101
Longissimus Thoracis Pars Thoracis. This muscle group consists of 11–12 pairs of muscles, which extend from the transverse processes of T2 and their ribs, and run inferomedially to attach to the spinous processes of L3–5 and the sacral spinous processes, as well as the PSIS.
The orientation and various attachments of this muscle group allow it to act indirectly on the lumbar spine. The main action of the muscle appears to be the extension of the thoracic spine on that of the lumbar. An anatomic-mathematical study102 suggests that 70–80% of the force required to extend the upper lumbar spine is produced from the thoracic fibers of the erector spinae, which also generate 50% of the force at the lower levels.
Iliocostalis Lumborum Pars Thoracis. The thoracic iliocostalis serves as the thoracic part of the iliocostalis lumborum and not the iliocostalis thoracic. It is a layered muscle consisting of inferomedially orientated fascicles attached to the following points101:
 lateral part of the lower eight rib angles;
lateral part of the lower eight rib angles;
 PSIS; and
PSIS; and
 the posterior (dorsal) surface of the sacrum, distal to the multifidus.
the posterior (dorsal) surface of the sacrum, distal to the multifidus.
This muscle completely spans the lumbar spine and is in an excellent position to extend and side bend the spine, as well as to increase the lumbar lordosis. It is a weak rotator because the amount of rib separation on ipsilateral rotation is minor, but on contralateral rotation, it is better. It is, therefore, possible that the muscle is an effective derotator of the spine.12
Abdominal Muscles
Rectus Abdominis. The rectus abdominis (Fig. 28-4) originates from the cartilaginous ends of the fifth through seventh ribs and xiphoid and inserts on the superior aspect of the pubic bone. The linea alba (Fig. 28-4) is the anterior abdominal aponeurosis or rectus sheath in the midline. It is formed by the interlacing of the aponeurosis of the external oblique, internal oblique (IO), and transverse abdominis (TrA) muscles from both sides. It is broader superiorly, where the recti are separated at a considerable interval, and narrower inferiorly, where the recti are closely packed (Fig. 28-4). Above the umbilicus, the linea alba is a single layer, whereas below the umbilicus it has a double layer.103
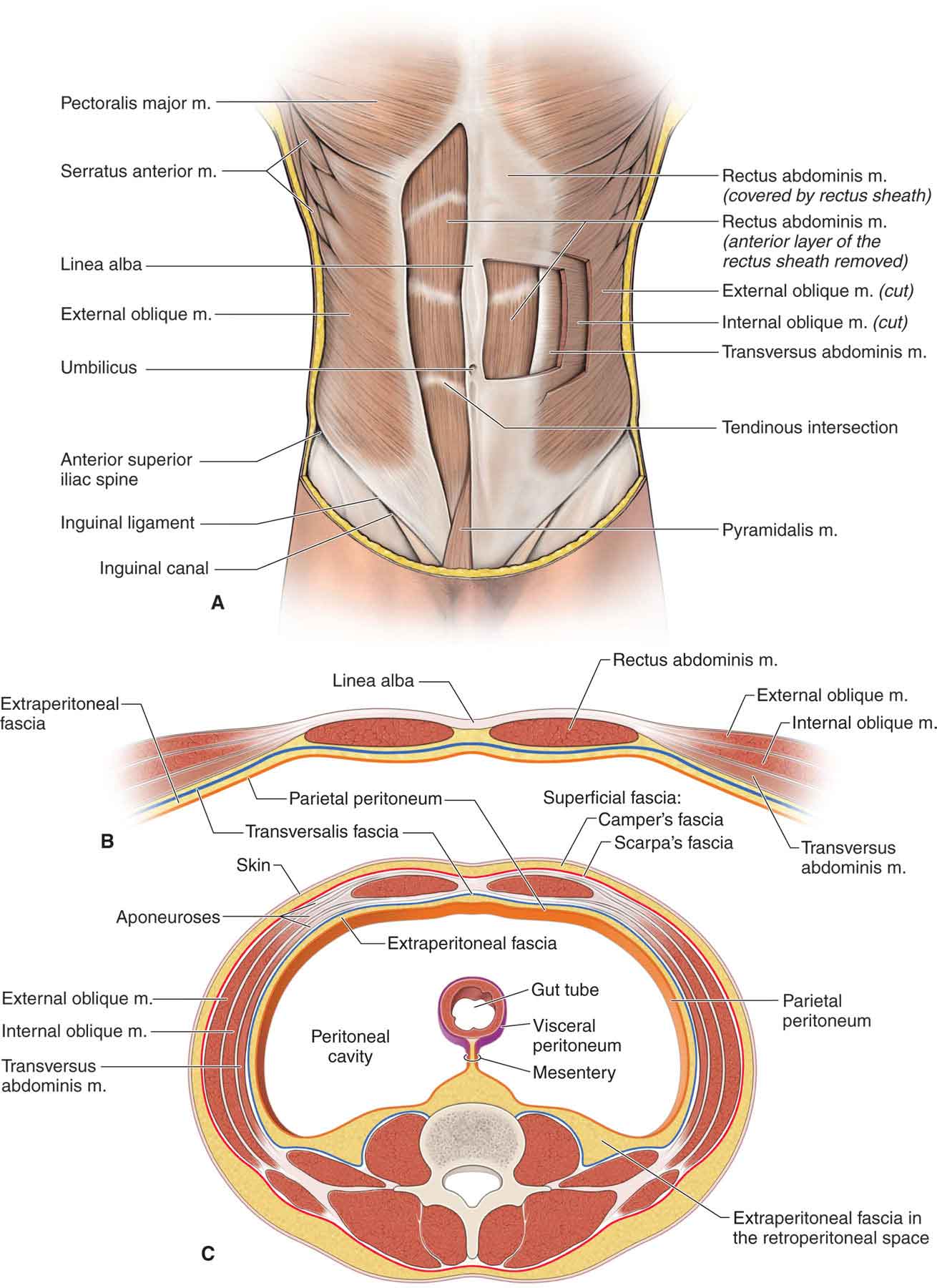
FIGURE 28-4 Abdominal muscles. (Reproduced, with permission, from Chapter 7. Anterior Abdominal Wall. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The rectus abdominis muscle functions to produce torque during flexion of the vertebral column, as it approximates the thorax and pelvis anteriorly.109 The muscle appears to serve a beneficial role in helping to stabilize the lumbar spine in the sagittal plane.88
Transversus Abdominis. The TrA muscle (Fig. 28-4) originates from the lateral one-third of the inguinal ligament, the anterior two-thirds of the inner lip of the iliac crest, the lateral raphe of the TLF, and the internal aspects of the lower six costal cartilages, where it interdigitates with the diaphragm.110 Its upper and middle fibers run transversely around the trunk and blend with the fascial envelope of the rectus abdominis muscle, while the lower fibers blend with the insertion of the IO muscle on the pubic crest.111 A number of differences in the fiber orientation of the upper, middle, and lower regions of the TrA have been noted112:
 Upper fibers: these fibers, which include the fibers from the sixth costal cartilage to the inferior border of the rib cage, have been found to be oriented superomedially.
Upper fibers: these fibers, which include the fibers from the sixth costal cartilage to the inferior border of the rib cage, have been found to be oriented superomedially.
 Middle fibers: these fibers, which include the fibers from the inferior border of the rib cage to a line connecting the superior borders of the iliac crest, have been found to be oriented inferomedially.
Middle fibers: these fibers, which include the fibers from the inferior border of the rib cage to a line connecting the superior borders of the iliac crest, have been found to be oriented inferomedially.
 Lower fibers: these fibers, which include those from the iliac crest and the pubic symphysis, were found to be oriented more inferomedially than the middle fibers.
Lower fibers: these fibers, which include those from the iliac crest and the pubic symphysis, were found to be oriented more inferomedially than the middle fibers.
Although much emphasis has traditionally been placed on the strengthening of the rectus abdominis during lumbar spine rehabilitation, attention has switched to the contraction of the hoop-like TrA that creates a rigid cylinder, resulting in enhanced stiffness of the lumbar spine and stabilization of the lumbar motion segment (see “Biomechanics” section).2,79,113–116 Since the midportion of the TrA attaches to the cross-hatch arrangement of the middle layer of the TLF (see later), contraction of the TrA has been thought to increase spinal stability and a motor control via tensioning of the TLF in the middle and lower regions of the lumbar spine or by producing a mild stabilizing compressive force on the lumbar vertebrae.88,110,116 The TLF creates a pressurized visceral cavity anterior to the spine when the TrA contracts. This force is theorized to increase the stability of the lumbar spine during a variety of postures and movements.117
Internal Oblique. The IO (see Fig. 28-4), which forms the middle layer of the lateral abdominal wall, is located between the TrA and the external oblique muscles.118 It has multiple attachments to the inguinal ligament, lateral raphe, iliac crest, pubic crest, TrA, and costal cartilages of the seventh through ninth costal cartilages. Because of these multiple attachment sites, the different fascicles of the muscle can have very different force vectors.
The IO is active during a number of functions, including gait (most often close to initial contact119) and erect sitting and standing postures.120 Acting bilaterally, the IOs flex the vertebral column and assist in respiration. Acting in unison, the muscle, in conjunction with the external obliques, can produce rotation of the vertebral column, bringing the thorax backward (when the pelvis is fixed) or the pelvis forward (when the thorax is fixed).109,121
External Oblique. The external oblique (see Fig. 28-4) originates from the lateral aspect of the fifth through twelfth ribs, and through interdigitations with the serratus anterior and latissimus dorsi. The muscle travels obliquely, medially, and inferiorly to insert into the linea alba, inguinal ligament, anterior-superior iliac spine (ASIS), iliac crest, and pubic tubercle.
When acting bilaterally, the external obliques flex the vertebral column and tilt the pelvis posteriorly. Acting in unison, the muscle, in conjunction with the IOs, can produce side bending of the vertebral column, approximating the thorax and the iliac crest laterally.109
Researchers have suggested that the IOs, and to a lesser extent the external obliques, may contribute to the production of intraabdominal pressure and thus stability of the lumbar spine.122
Psoas Major
Although traditionally viewed as a muscle of the hip, the psoas major muscle combines with the iliacus muscle to directly attach the lumbar spine to the femur.123 The psoas major originates from
 anterolateral aspects of the vertebral bodies;
anterolateral aspects of the vertebral bodies;
 IVDs of T12–L5;
IVDs of T12–L5;
 transverse processes of L1–5; and
transverse processes of L1–5; and
 tendinous arch spanning the concavity of the sides of the vertebral bodies.
tendinous arch spanning the concavity of the sides of the vertebral bodies.
The iliacus is attached superiorly to the iliac fossa and the inner lip of the iliac crest. Joining with the psoas major, the combined tendon passes over the superior lateral aspect of the pubic ramus and attaches to the lesser trochanter of the femur.
Taken individually, the iliacus and psoas major serve different functions.
 The psoas major is electromyographically active in many different positions and movements of the lumbar spine, and its activity can add a stabilizing effect on the lumbar spine with compressive loading.124 With the foot fixed on the ground (closed chain), contraction of the psoas major increases the flexion of the lumbar-pelvic unit on the femur.125
The psoas major is electromyographically active in many different positions and movements of the lumbar spine, and its activity can add a stabilizing effect on the lumbar spine with compressive loading.124 With the foot fixed on the ground (closed chain), contraction of the psoas major increases the flexion of the lumbar-pelvic unit on the femur.125
 With the foot fixed on the ground, contraction of the iliacus produces an anterior torsion of the ilium and extension of the lumbar zygapophyseal joints. If there is a decrease in the length of the iliopsoas as a result of adaptive shortening or increased efferent neural input to the muscle, the result is an anteriorly rotated pelvis and an increase in lordosis. This may increase the anterior shear stress at the lumbosacral junction in any posture.124
With the foot fixed on the ground, contraction of the iliacus produces an anterior torsion of the ilium and extension of the lumbar zygapophyseal joints. If there is a decrease in the length of the iliopsoas as a result of adaptive shortening or increased efferent neural input to the muscle, the result is an anteriorly rotated pelvis and an increase in lordosis. This may increase the anterior shear stress at the lumbosacral junction in any posture.124
From a clinical perspective, the iliacus and psoas major usually are considered together as the iliopsoas. Working bilaterally (insertion fixed), the iliopsoas can produce flexion of the trunk on the femur as in the sit-up from a supine position, or in bending over to touch one’s toes. The iliopsoas muscle also side bends the spine ipsilaterally.124
Working from a stable spine above (origin fixed), the iliopsoas muscle flexes the hip joint by flexing the femur on the trunk.
The iliopsoas is innervated by the anterior (ventral) rami of L1 and L2.
Thoracolumbar Fascia
The TLF travels from the spinous process of T12 to the PSIS and iliac crest. The TLF consists of three layers of connective tissue that envelop the lumbar muscles and separate them into anterior, middle, and posterior compartments or layers126:
- The anterior layer covers the anterior surface of the quadratus lumborum muscle. It is attached to the anterior transverse processes and then to the intertransverse ligaments. On the lateral side of the quadratus lumborum, it blends with the other layers of the fascia.
- The middle layer is posterior to the quadratus lumborum, with its medial attachment to the tips of the transverse processes and the intertransverse ligaments. Laterally, it gives rise to, or is attached to, the transverse abdominal aponeurosis.
- The posterior layer covers the lumbar musculature and arises from the spinous processes, wrapping around the muscles. It blends with the other layers of the fascia along the lateral border of the iliocostalis lumborum in a dense thickening of the fascia called the lateral raphe.126 This layer consists of two laminae, a superficial one with its fibers orientated inferomedially, and a deep lamina whose fibers are inferolateral. The superficial fibers are derived from the latissimus dorsi.
The functions of the TLF are varied. The TLF
 provides muscle attachment for the transversus abdominis;
provides muscle attachment for the transversus abdominis;
 stabilizes the spine against anterior shear and flexion moments;
stabilizes the spine against anterior shear and flexion moments;
 resists segmental flexion via tension generated by the TrA on the spinous process; and
resists segmental flexion via tension generated by the TrA on the spinous process; and
 assists in the transmission of extension forces during lifting activities. The posterior ligamentous system has been proposed as a model to explain some of the forces required for lifting. It is believed to transmit forces by passive resistance to flexion, from the joint capsule and extracapsular ligaments, and from the more dynamic effects of the TLF.127
assists in the transmission of extension forces during lifting activities. The posterior ligamentous system has been proposed as a model to explain some of the forces required for lifting. It is believed to transmit forces by passive resistance to flexion, from the joint capsule and extracapsular ligaments, and from the more dynamic effects of the TLF.127
Lumbopelvic Fascia
The lumbopelvic fascia connects the proximal structures of the trunk to the hip girdle. The TrA, obliques, erector spinae, and multifidus all have attachments with the lumbopelvic fascia and connect the latissimus dorsi superiorly to the gluteal muscles inferiorly. It has been theorized that the lumbar fascia has a specialized function as an elastic structure storing energy from isometric actions of the latissimus dorsi and contralateral gluteus maximus during ambulation.128 The latissimus dorsi and gluteus maximus are linked through this structure and provide a “pathway for uninterrupted mechanical transmission between pelvis and trunk” through muscular “slings.”129 Vleeming et al.129 have proposed four sling systems130:
 The anterior oblique system, which is comprised of the external oblique, contralateral IO, and contralateral adductors. This system contributes to force closure of the pubic symphysis and sacroiliac joint.
The anterior oblique system, which is comprised of the external oblique, contralateral IO, and contralateral adductors. This system contributes to force closure of the pubic symphysis and sacroiliac joint.
 The posterior oblique system which is comprised of the latissimus dorsi, contralateral gluteus maximus, and TLF. This system contributes to the force closure of the sacroiliac joint and is a significant contributor to load transference through the pelvic girdle during rotational activities and gait. The fibers of the latissimus dorsi and contralateral gluteus maximus are in line with each other, and perpendicular to the sacroiliac joint, providing external support.
The posterior oblique system which is comprised of the latissimus dorsi, contralateral gluteus maximus, and TLF. This system contributes to the force closure of the sacroiliac joint and is a significant contributor to load transference through the pelvic girdle during rotational activities and gait. The fibers of the latissimus dorsi and contralateral gluteus maximus are in line with each other, and perpendicular to the sacroiliac joint, providing external support.
 The deep longitudinal system, which is comprised of the erector spinae, sacrotuberous ligament, and multifidus, biceps femoris, fibularis (peroneus) longus, and anterior tibialis. This system is engaged when the foot is in contact with the ground and serves to transmit energy from the upper trunk through the thoracic or lumbar fascia and erector spinae muscles to the biceps femoris and the lower extremity musculature.
The deep longitudinal system, which is comprised of the erector spinae, sacrotuberous ligament, and multifidus, biceps femoris, fibularis (peroneus) longus, and anterior tibialis. This system is engaged when the foot is in contact with the ground and serves to transmit energy from the upper trunk through the thoracic or lumbar fascia and erector spinae muscles to the biceps femoris and the lower extremity musculature.
 The lateral system which is comprised of the gluteus medius and minimus, contralateral adductors, and contralateral quadratus lumborum. The muscles of this system provide essential frontal plane stability by indirectly facilitating pelvic girdle control during standing and ambulation.
The lateral system which is comprised of the gluteus medius and minimus, contralateral adductors, and contralateral quadratus lumborum. The muscles of this system provide essential frontal plane stability by indirectly facilitating pelvic girdle control during standing and ambulation.
Nerve Supply of the Lumbar Segment
The nerve supply to the lumbar spine follows a general pattern. The outer half of the IVD is innervated by the sinuvertebral nerve37 and the gray rami communicantes,131 with the posterolateral aspect innervated by both the sinuvertebral nerve59 and the gray rami communicantes. The lateral aspect receives only sympathetic innervation.
The zygapophyseal joints are innervated by the medial branches of the posterior (dorsal) rami.37,65,132 Each joint receives its nerve supply from the corresponding medial branch above and below the joint.37,65 For instance, the L4–5 joint receives its nerve supply from the medial branches of L3 and L4. The lateral branches cross the subjacent transverse process and pursue a sinuous course inferiorly, laterally, and posteriorly through the iliocostalis lumborum.65 They innervate that muscle, and eventually the L1–3 lateral branches pierce the posterior (dorsal) layer of TLF and become cutaneous, supplying the skin over the lateral buttock as far as the greater trochanter.37,65 The intermediate branches run posteriorly and inferiorly from the intertransverse spaces. They form a series of intersegmental communications within the longissimus thoracis.37,65
At the L1 and L2 levels, the nerves exit the intervertebral foramen above the disk. From L2 downward, the nerves leave the dura slightly more proximally than the foramen through which they pass, and at a decreasing angle of obliquity and an increasing length of the spinal canal. The L3 nerve root travels behind the inferior aspect of the vertebral body and the L3 disk. The L4 nerve root crosses the whole vertebral body to leave the spinal canal at the upper aspect of the L4 disk, at an angle of approximately 60 degrees. The L5 nerve root emerges at the inferior aspect of the fourth lumbar disk at an angle of approximately 45 degrees and crosses the fifth vertebral body to exit at the upper aspect of the L5 disk. The S1 nerve root emerges at a 30-degree angle and crosses the L5–S1 disk.
Lumbar Spine Vascularization
The blood supply to the lumbar spine is provided by the lumbar arteries (Fig. 28-5), and its venous drainage occurs via the lumbar veins (Fig. 28-5).
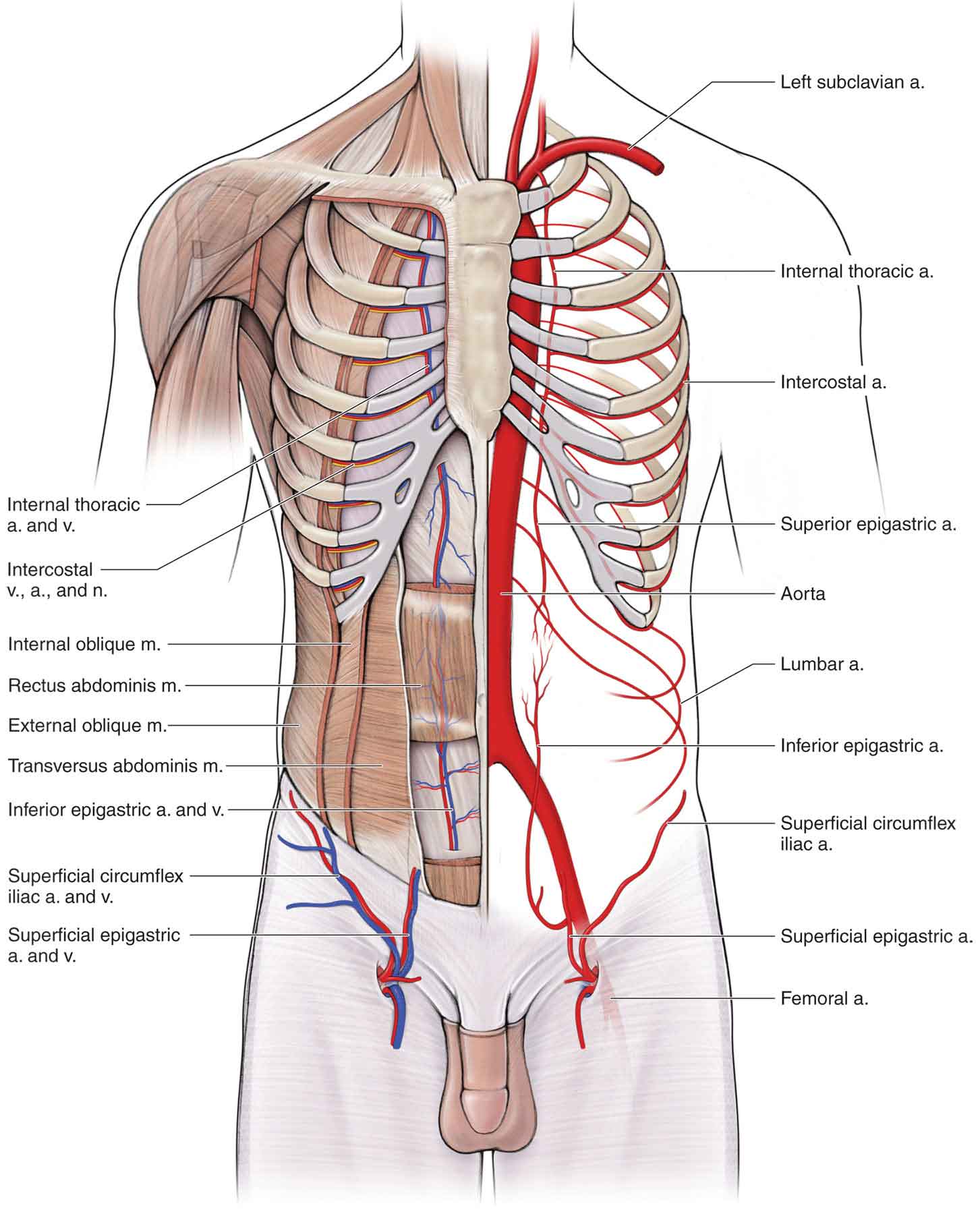
FIGURE 28-5 Vasculature of the spine. (Reproduced, with permission, from Chapter 7. Anterior Abdominal Wall. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
BIOMECHANICS
Physiologic motions at the lumbar spine joints can occur in three cardinal planes: sagittal (flexion and extension), coronal (side bending), and transverse (rotation). Including accessory motions, six degrees of freedom are available at the lumbar spine.60
The amount of segmental motion at each vertebral level varies. Most of the flexion and extension of the lumbar spine occurs in the lower segmental levels, whereas most of the side bending of the lumbar spine occurs in the midlumbar area.110,133,134 Rotation, which occurs with side bending as a coupled motion, is minimal and occurs most at the lumbosacral junction.110,133,134 The amount of range available in the lumbar spine generally decreases with age.135
Flexion
The lumbar spine is well designed for flexion, which is its most commonly used motion in daily activities. Flexion of the lumbar spine from erect standing involves an unfolding or straightening of the lumbar lordosis, followed by, at most, a small reversal of the lordotic curve.136 The flexion–extension range of the lumbar spine that occurs between vertebral segments is approximately 12 degrees in the upper lumbar spine, increasing by 1–2 degrees per segment to reach a maximum motion of 20–25 degrees between L5 and S1.12,134
During lumbar flexion in standing, which normally is initiated by the abdominal muscles, the entire lumbar spine leans forward, and there is a posterior sway of the pelvis as the hips flex.
At the segmental level, lumbar flexion produces a combination of an anterior roll and an anterior glide of the vertebral body, and a straightening, or minimal reversal, of the lordosis.110,134 At L4–5, reversal may occur, but at the L5–S1 level, the joint will straighten but not reverse138 unless there is pathology present. During the anterior rocking motion of the segment that occurs with flexion, the inferior facets of the superior vertebra lift upward and backward, opening a small gap between the facets. The superior vertebra translates anteriorly by approximately 5–7 mm, closing the gap and enhancing stability through increased tension of the joint capsule.55 The anterior sagittal translation, or shear, is also resisted by
 the superoanterior orientation of the lateral fibers of the AF;
the superoanterior orientation of the lateral fibers of the AF;
 the iliolumbar and SSLs at the L5–S1 segment, with the longitudinal ligaments helping to a lesser extent;
the iliolumbar and SSLs at the L5–S1 segment, with the longitudinal ligaments helping to a lesser extent;
 the semisagittal and sagittal orientation of the zygapophyseal joints, which cause the superior facet to come against the inferior one during an anterior shear, with the highest pressure occurring on the anteromedial portion of the superior zygapophyseal joint surface. The zygapophyseal joints are, therefore, vital in the limitation of this anterior shear.139
the semisagittal and sagittal orientation of the zygapophyseal joints, which cause the superior facet to come against the inferior one during an anterior shear, with the highest pressure occurring on the anteromedial portion of the superior zygapophyseal joint surface. The zygapophyseal joints are, therefore, vital in the limitation of this anterior shear.139
 the horizontal vector of the erector spinae and the multifidus, which acts to pull the vertebrae posteriorly.
the horizontal vector of the erector spinae and the multifidus, which acts to pull the vertebrae posteriorly.
Flexion is also limited by the compressibility of the anterior structures, such as the IVD, and by the extensibility of the posterior structures of the segment (ligaments, IVD, and muscles). These structures have varying contributions to the resistance of segmental flexion, depending on the degree of flexion140:
 The joint capsule resists approximately 39%.
The joint capsule resists approximately 39%.
 The supraspinous and interspinous ligaments resist approximately 19%.
The supraspinous and interspinous ligaments resist approximately 19%.
 The LF ligament resists approximately 13%.
The LF ligament resists approximately 13%.
 The IVD resists approximately 29%.
The IVD resists approximately 29%.
Extension
Extension movements of the lumbar spine produce a reverse of those that occur in flexion. Theoretically, true extension of the lumbar spine is pathologic and depends on one’s definition: pure extension involves a posterior roll and glide of the vertebra and a posterior and inferior motion of the zygapophyseal joints, but not necessarily a change in the degree of lordosis.134 During lumbar extension, the inferior zygapophyseal joint of the superior vertebra moves downward, impacting with the lamina below and producing a buckling of the interspinous ligament between the two spinous processes. This impaction is accentuated when the joint is subjected to the action of the back muscles.141 If the extending force continues to be applied, especially unilaterally, the superior facets can pivot on their inferior counterparts, producing a strain on the opposite zygapophyseal joint, and potentially damaging or tearing the capsule.12
An anterior pelvic tilt increases the lumbar lordosis and results in an anterior motion of the vertebrae and their associated structures. Although the differing terminology between true extension and the extension created by increasing the lordosis is seemingly esoteric, there are clinical implications during the examination, when the clinician is assessing the ability of the patient to assume the extended position of the lumbar spine.
Pure lumbar extension is limited by
 the ability of structures anterior to the fulcrum to be elongated;
the ability of structures anterior to the fulcrum to be elongated;
 the ability of the IVD to allow compression;
the ability of the IVD to allow compression;
 joint capsule tension; and
joint capsule tension; and
 the passive tension of the psoas major muscle.
the passive tension of the psoas major muscle.
AXIAL ROTATION
Intervertebral Disk
Approximately 65% of the resistance to IVD torsion is resisted by a combination of tension and impaction of the contralateral zygapophyseal joint, and tension of the supraspinous and interspinous ligaments, with the disk contributing approximately 35% of the resistance.144 During axial rotation, which produces torsion of the IVD, those collagen fibers of the AF that are orientated in the same direction as the twist are stretched and resist the torsional force, while the others remain relaxed, thereby sharing the stress of twisting.
During forced segmental torsion, the first structure to fail is the zygapophyseal joint, which normally occurs at approximately 1–2 degrees of segmental rotation.144 As collagen can only elongate approximately 4% before damage, the maximum segmental rotation at each segmental level is typically limited to approximately 3 degrees.16,60 Macroscopic failure of the IVD is likely to occur only in the presence of extreme trauma, with an accompanying fracture of the zygapophyseal joint.28 However, surgical incision of the zygapophyseal joint, or facetectomy, which increases the amount of rotation the segment is capable of handling, also significantly increases the stress in the posterior AF fibers.28,144
In the absence of zygapophyseal joint damage, surgical or otherwise, axial rotation must be coupled with other motions to cause disk injury.49 For example, the combination of maximal lumbar flexion and rotation, which increases the amount of rotation before the contralateral zygapophyseal joint makes contact, has been associated with trauma to the AF.145,146
Other Structures
Rotational movements of the lumbar spine do appear to produce the appropriate motor patterns for optimal trunk muscle cocontraction and spinal stability.114,147 The axis of rotation in the sagittal plane passes through the anterior aspect of the IVD and vertebral body.148 For axial displacements, the axis of rotation tends to be located within the posterior annulus.148 Axial rotation of the lumbar spine amounts to approximately 13 degrees to both sides. The greatest amount of segmental rotation, approximately 5 degrees, occurs at the L5 and S1 segments. Axial rotation of the segment involves
 twisting, or torsion, of the IVD fibers;
twisting, or torsion, of the IVD fibers;
 compression of the contralateral zygapophyseal joint, for example, with left axial rotation, the right inferior zygapophyseal joint will impact on the superior zygapophyseal joint of the bone below; and
compression of the contralateral zygapophyseal joint, for example, with left axial rotation, the right inferior zygapophyseal joint will impact on the superior zygapophyseal joint of the bone below; and
 stress on those annular fibers inclined toward the direction of rotation.
stress on those annular fibers inclined toward the direction of rotation.
In normal segments, the zygapophyseal joints protect the IVD from torsional injuries by coming into contact before microfailure of the IVD can occur. During axial rotation, tension is built in the interspinous and SSLs, and the contralateral joint becomes impacted after 1–2 degrees of rotation.144 Further movement is accommodated by compression of the articular cartilage. If this range is exceeded, any further rotation that occurs is impure. Impure rotation of the segment forces the upper vertebra to pivot backward on the impacted joint, around the newly created axis of rotation. This causes the vertebra to swing laterally and backward, increasing the potential for a lateral shear force on the annulus. At this extreme, the IVD is vulnerable to either torsional or shear forces, and the other joint capsule is placed under severe tension.28 This combination can result in a failure of any one of these structures, resulting in any or all of the following: compression fractures of the contralateral lamina, subchondral fractures, fragmentation of the articular surface and tearing, avulsion of the ipsilateral joint capsule, or a pars interarticularis fracture.12
The ipsilateral joint does not normally gap during normal axial rotation, except during therapeutic manipulation.149 Abnormal gapping has been found to occur in segments with degenerative or traumatic instability, questioning the role of therapeutic manipulation in such cases.149
SIDE BENDING
Side bending is a complex and highly variable movement involving side bending and rotatory movements of the interbody joints and a variety of movements at the zygapophyseal joints.136 The means of how this is achieved has been the subject of debate for many years, and it is difficult to ascertain how an impaired segment would behave, compared with a healthy one.150 The general pattern of coupled motion is for side bending to be associated with contralateral axial rotation at the mid and upper lumbar levels but ipsilateral axial rotation at L5–S1.136 However, there is at present little evidence for strict rules of coupled motion that determine whether an individual has abnormal ranges or directions of coupling in the lumbar spine.136,151
Bending motions can occur in any direction, producing both a rocking motion and a translation shearing effect on the IVD. The NP tends to be compressed and the AF buckles in the direction of the rocking motion,152 and there is a tendency for the AF to be stretched in the opposite direction, while the pressure on the posterior aspect of the NP is relieved. Although the deformation can occur in a healthy disk, displacement of the NP is prevented by the AF that encapsulates it. The AF will buckle at its compressed aspect because it is not braced by the NP, which is exerting that effect on the AF fibers at the opposite side of the disk.16
AXIAL LOADING (COMPRESSION)
Axial compression or spinal loading occurs in weight bearing, whether in standing or sitting.
Intervertebral Disk
It has been demonstrated experimentally that the AF, even without the NP, can withstand the same vertical forces that an intact disk can for short periods,153 provided that the lamellae do not buckle. However, if the compression is prolonged, or if the lamellae are not held together, the sheets buckle and the system collapses on itself.
The extent and magnitude of the compression depend on the amount of applied compressive force, the disk height, and the cross-sectional area of the disk. Variations in disk height can be divided into two categories: primary disk height variations and secondary disk height changes.
- Primary disk height variations are related to intrinsic individual factors, such as body height, gender, age, disk level, and geographic region.154,155
- Secondary disk height changes are associated with extrinsic factors, such as degeneration, abnormality, or clinical management. Surgical procedures, such as nucleotomy, diskectomy, and chemonucleolysis cause a decrease in disk height, resulting from the removal of a portion of the NP or damage to the water-binding capacity of the extracellular matrix.156–158 In addition, there are diurnal changes in disk height, which are caused by fluid exchange and creep deformation.159
With variations in disk height, one would expect changes in the mechanical behavior of the disk. An important result to emerge from a recent study is that axial displacement, posterolateral disk bulge, and tensile stress in the peripheral AF fibers are a function of axial compressive force and disk height.160 Under the same axial force, disks with a higher height-to-area ratio generate higher values of axial displacement, disk bulge, and tensile stress on the peripheral AF fibers.
The NP is deformable but relatively incompressible. Therefore, when a load is applied to it vertically, the nuclear pressure rises, absorbing and transmitting the compression forces to the vertebral end plates and the AF.12
 The resistance of the end plate is dependent on the strength of the bone beneath and the blood capacity of the vertebral body.
The resistance of the end plate is dependent on the strength of the bone beneath and the blood capacity of the vertebral body.
 The AF bulges radially,161 delaying and graduating the forces.
The AF bulges radially,161 delaying and graduating the forces.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




