INDICATIONS/CONTRAINDICATIONS
Posterior-based osteotomies contraction (PSO) in the lumbar spine encompass a spectrum of techniques that are intended to realign the spine through resection of posterior elements with variable resection of the anterior column of the spine. The spectrum of posterior-based osteotomies is listed in
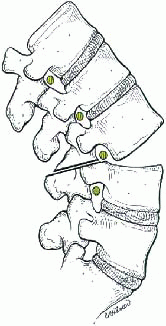
Table 20-1. The spectrum of osteotomies is a continuum, and the osteotomy techniques share steps including resection of the facet joints, decancellation, and partial or complete corpectomy from a posterior approach. The spectrum of osteotomies begins with a resection of the facet joints alone and realignment of the spine with an axis of rotation at the anterior longitudinal ligament in a mobile spine (type 1) or anterior column osteoclasis through a rigid spine (type 2). Decancellation of the vertebral body through the pedicle permits a controlled fracture of the anterior column and may be useful in realigning the spine in the coronal and sagittal plane, as described by Heinig in the “eggshell osteotomy” (type 3). The lumbar pedicle subtraction osteotomy is a wedge resection of the vertebral body from below the pedicle to the anterior cortex of the vertebra, and the wedge resection may be entirely intraosseous with a hinge on the superior third of the vertebral body (type 5) or at the supraadjacent disc (type 6). Finally, a posterior resection of one or more vertebra and discs may be useful in treating more complex deformity including translation of the trunk. The purpose of this chapter is to describe the technique of the lumbar pedicle subtraction osteotomy.
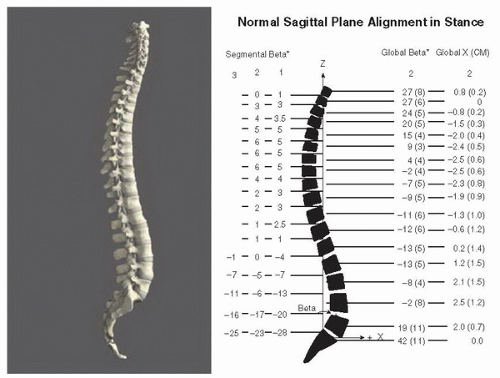
The lumbar pedicle subtraction osteotomy (transpedicular vertebral wedge resection) is a useful technique for the operative correction of both sagittal and coronal plane deformity (
4). The clinical impact of deformity is determined and predicted primarily by the sagittal plane (
12,
18). The primary indication for the technique is correction of sagittal plane deformity in the patient who has had a previous circumferential fusion of the spine. The transpedicular wedge resection technique was first described by Thomasen (
27) in 1989 for the management of fixed sagittal plane deformity in ankylosing spondylitis. Common etiologies of fixed sagittal plane deformity include ankylosing spondylitis, or iatrogenic causes of fixed sagittal plane deformity including flatback syndrome (
8) and kyphotic decompensation syndrome (
10). More generally, lumbar spine kyphosis with variable degrees of rigidity may be the result of degenerative change, congenital anomaly, trauma, neoplastic disease with pathologic fracture, or infection. The rigidity of lumbar kyphosis and the apex of the deformity are important determinants of the surgical approach. In a spine with a mobile anterior column, or a flexible deformity, posterior-based osteotomies with facet resection and deformity correction through the disc space or osteoclasis of the anterior column may be useful. In a spine with an apex of deformity at L4 or L5, a combined anterior and posterior approach to the spine may be useful in recreating lordosis at the lumbosacral segments and correcting a rigid coronal obliquity of a fractional curve from L4 to S1. The lumbar pedicle subtraction osteotomy may be used at any level of the lumbar spine and is most useful for rigid deformity, which requires resection of bone including a portion of the anterior column for mobilization and realignment. The technique may also be used above the level of the conus including the cervical and thoracic spine.
The lumbar pedicle subtraction osteotomy fits best in the spectrum or posterior-based osteotomies as an option for patients with a sagittal deformity that is correctable with an apical resection of approximately 30 degrees and coronal imbalance less than 8 cm (
1). Although the lumbar pedicle subtraction osteotomy may be used in the patient with open disc spaces and mobility of the anterior column of the spine, the authors prefer to use a combined anterior and posterior approach (
5), or posterior-based osteotomies as described by Ponte for the patient with a mobile anterior column as these techniques permit a more gradual and harmonious realignment of the spine through the creation of trapezoidal intervertebral disc spaces (
11). If osteoclasis is possible for the anterior column, the Smith-Peterson osteotomy may be useful to create segmental realignment (
23). In the patient with a severe lumbar kyphosis that requires more than 40 degrees of correction, or trunk translation and coronal imbalance greater than 8 cm, a vertebral column resection may prove more advantageous (
6,
26).