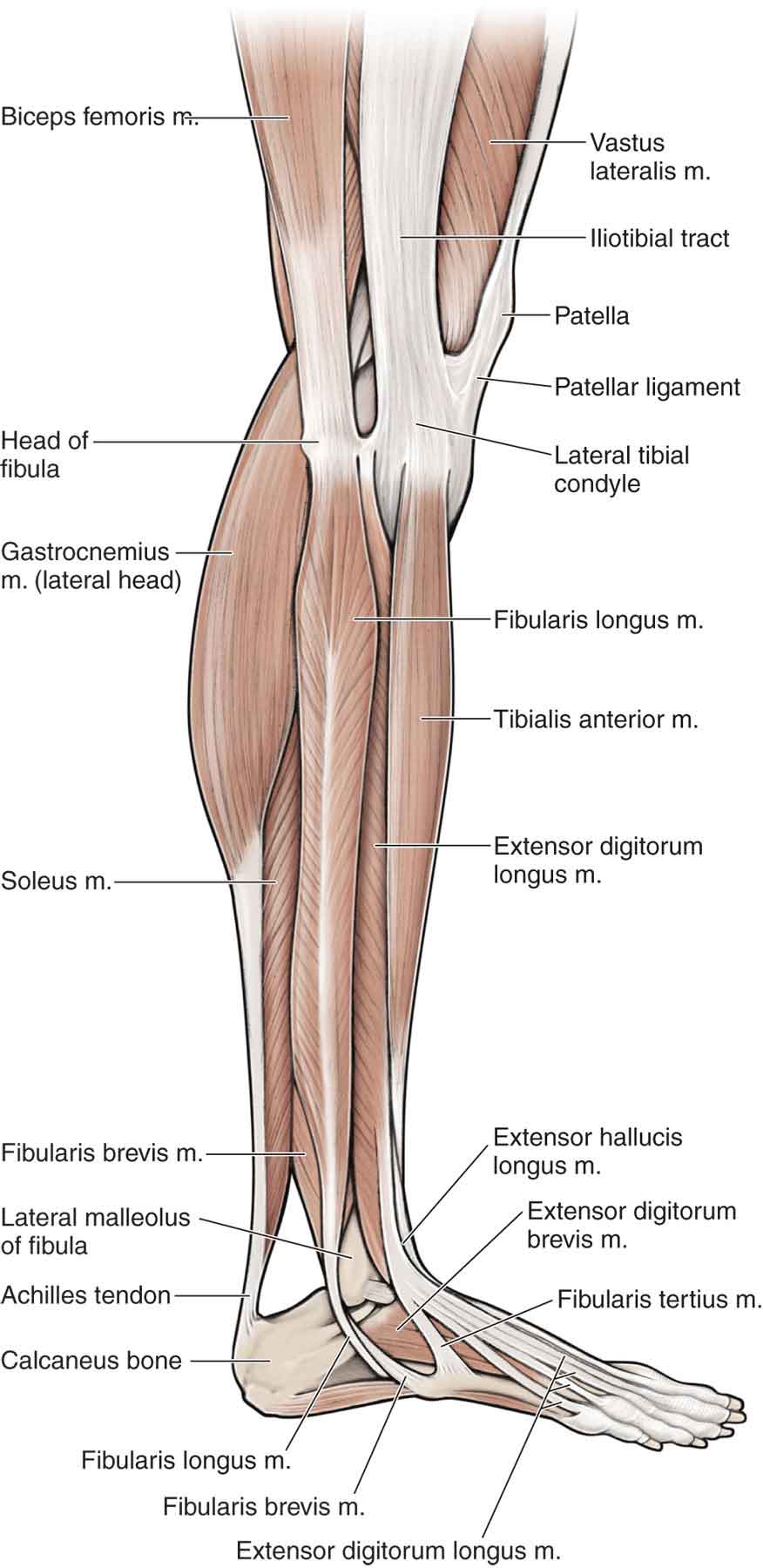
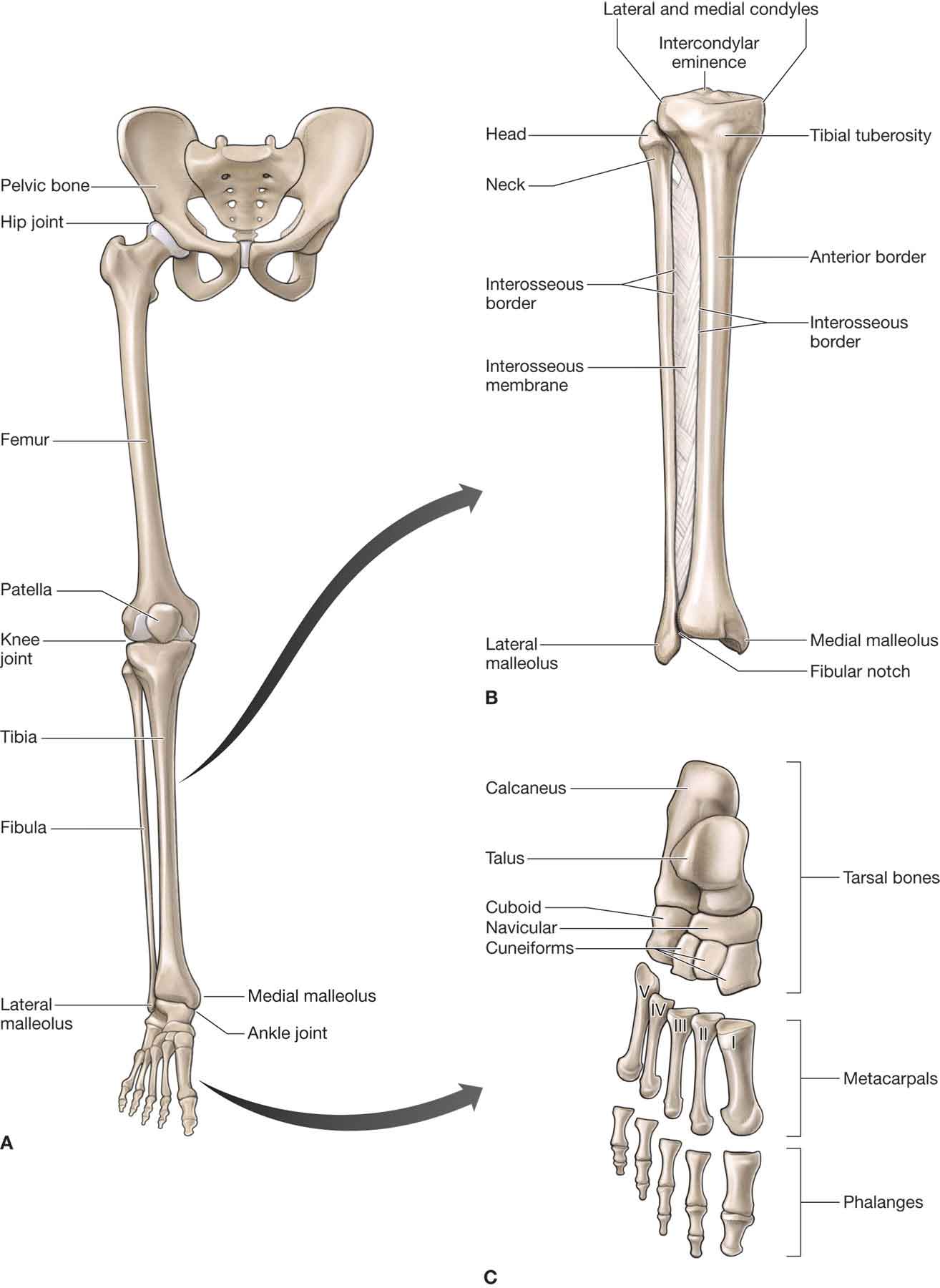
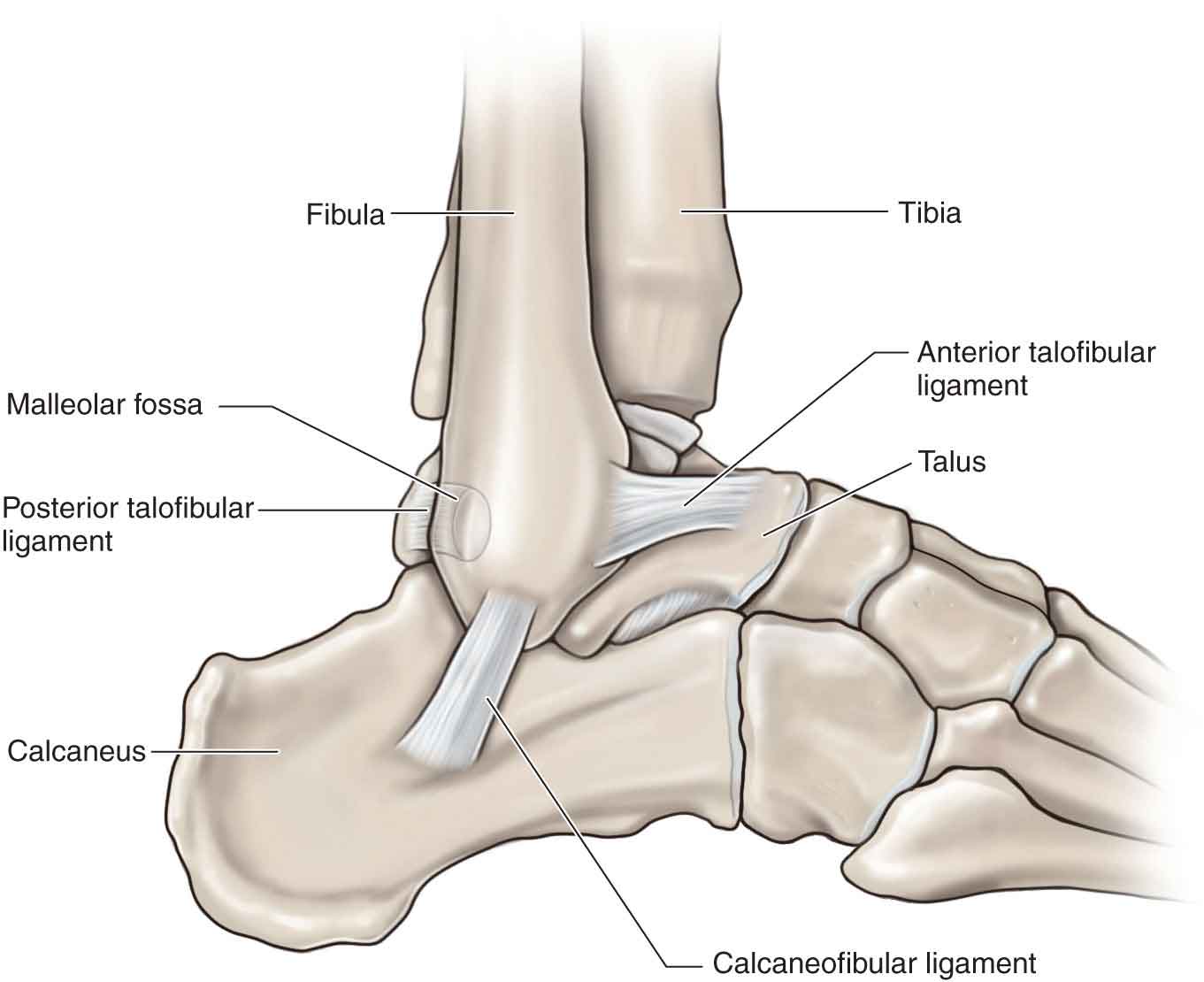
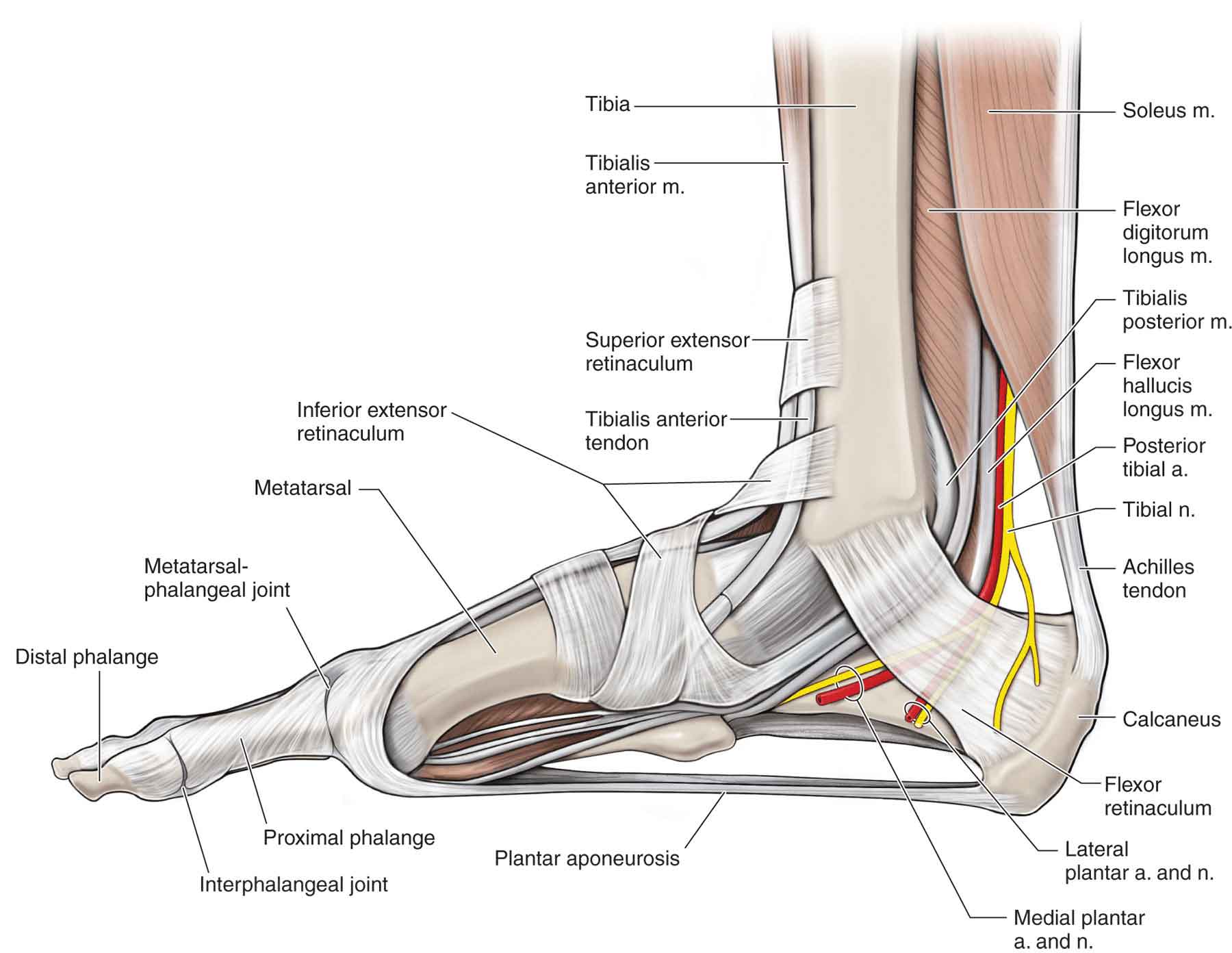
The ankle and foot is a complex structure of 28 bones, also known as tarsals, (including two sesamoid bones) and 27 articulations (including 20 synovial joints), interconnected by more than 100 ligaments and muscles. The foot and ankle are uniquely differentiated to provide enough mobility to adapt to different surfaces and attenuate shock, yet maintain sufficient stability for effective locomotion.1 In order to perform these diverse functions, the foot has undergone a number of evolutionary adaptations. First, the foot has become plantigrade, which allows most of the sole to be a weight-bearing surface. Second, the great toe has come to lie in a position with the other toes and, because of the relative immobility of the first metatarsal at the metatarsophalangeal (MTP) joint, is now relatively nonprehensile. Third, the metatarsals and phalanges have progressively shrunk and become small in comparison to the hypertrophied tarsus. Last, the medial side of the foot has become larger and stronger than that of any other primate. Unfortunately, when the requirements for foot and ankle mobility and stability are exceeded, structural breakdown occurs. Increasing the potential for breakdown is the fact that the ankle joint sustains the greatest load per surface area of any joint of the body.2 Peak vertical forces reach 120% of body weight during walking, and they approach 275% while running.3 The joints and ligaments of the ankle and foot complex act as stabilizers against these forces and constantly adapt during weight-bearing activities, especially on uneven surfaces. It is estimated that an average 180-lb man absorbs 76.2 tons on each foot while walking 1 mile and that the same man absorbs 121.5 tons per foot while running 1 mile.4 Approximately 60% of this weight-bearing load is carried out by the hindfoot,5 and 28% by the metatarsal heads.6 Although the ankle and foot complex normally adapts well to the stresses of everyday life, sudden or unanticipated stresses to this region have the potential to produce dysfunction. Anatomically and biomechanically, the foot can be subdivided into the hindfoot, sometimes referred to as the rear foot (tibia, talus, and calcaneus), the midfoot (the navicular, cuboid, and the three cuneiforms), and the forefoot (the 14 bones of the toes, the five metatarsals, and the medial and lateral sesamoids) (Table 21-1 and Fig. 21-1). The seven tarsal bones occupy the proximal half of the foot (see Fig. 21-1). TABLE 21-1 The Joints of the Foot and Ankle: Their Open- and Close-Packed Positions and Capsular Patterns Joints of the Hindfoot Open-Packed Position Close-Packed Position Capsular Pattern Tibiofibular joint Plantarflexion Maximum dorsiflexion Pain on stress Talocrural joint 10 degrees of plantarflexion and midway between inversion and eversion Maximum dorsiflexion Plantarflexion and dorsiflexion Subtalar joint Midway between the extremes of ROM Supination Varus and valgus Joints of the Midfoot Midtarsal joints Midway between the extremes of ROM Supination Dorsiflexion, plantarflexion, adduction, and internal rotation Joints of the Forefoot Tarsometatarsal joints Midway between the extremes of ROM Supination None Metatarsophalangeal joints 10 degrees of extension Full extension Great toe: extension and flexion of second to fifth toes: variable Interphalangeal joints Slight flexion Full extension Flexion and extension FIGURE 21-1 Bones of the lower extremity and foot. (Reproduced, with permission, from Chapter 34. Overview of the Lower Limb. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The ankle and foot complex is a sophisticated musculoskeletal arrangement designed to facilitate numerous and various weight-bearing and non–weight-bearing functions.7 Although described separately, the joints of the lower leg, ankle, and foot act as functional units and not in isolation. The joints of the foot and ankle, their open- and close-packed positions, and capsular patterns are outlined in Table 21-1. The shapes of the articulating surfaces of the leg and foot are outlined in Table 21-2. An appreciation of the shapes of the articulating surfaces is important when examining the joint glides and when performing joint mobilizations. Most of the stability of the foot and ankle is provided by a vast array of ligaments (Table 21-3). TABLE 21-2 Shapes of the Articulating Surfaces of the Leg and Foot Joint Proximal Bone and Shape of Its Joint Surface Distal Bone and Shape of Its Joint Surface Inferior tibiofibular Tibia—concave Fibula—convex Talocrural Tibia—concave in anterior–posterior direction and concave–convex–concave in mediolateral direction Fibula—convex in anterior–posterior direction and convex–concave–convex in mediolateral direction Talocalcaneal Talus—posterior facet biconcave, middle facet biconvex, and anterior facet convex Calcaneus—posterior facet biconvex, middle facet biconcave, and anterior facet concave Talonavicular Talus—biconvex Navicular—biconcave Calcaneocuboid Calcaneus—convex in mediolateral direction and concave in superior–inferior direction (saddle shaped) Cuboid—concave in mediolateral direction and convex in superior–inferior direction (saddle shaped) Cuboideonavicular Navicular—planar Cuboid—planar Cuneonavicular Navicular—slightly convex Cuneiforms—slight concave Intercuneiform Cuneiforms (medial and middle)—planar Cuneiforms (middle and lateral)—planar Cuneocuboid Lateral cuneiform—planar Cuboid—planar Tarsometatarsal Cuneiforms and cuboid—planar to slightly convex Bases of metatarsals—planar to slightly concave Metatarsophalangeal Metatarsals—biconvex Proximal phalanges—biconcave Interphalangeal Proximal phalanges—convex in superior–inferior and concave in medial–lateral direction Middle phalanges—concave in superior–inferior and convex in medial–lateral direction TABLE 21-3 Ankle and Foot Joints and Associated Ligaments Joint Associated Ligament Fiber Direction Motions Limited Distal tibiofibular Distolateral Anterior tibiofibular Distal and posterior glide of fibula Posterior tibiofibular Distolateral Distal and anterior glide of fibula Interosseous Distolateral Separation of tibia and fibula Ankle Deltoid (medial collateral) Superficial Tibionavicular Plantar–anterior Lateral translation and external rotation of the talus Calcaneotibial Plantar, plantar–posterior Eversion (abduction of talus, calcaneus and navicular) Posterior talotibial Plantar–posterior Dorsiflexion, lateral translation and external rotation of the talus Deep Anterior talotibial Lateral or fibular collateral Anterior Abduction of the talus when in plantarflexion or eversion Anterior talofibular Anterior–medial Inversion and plantarflexion Anterior displacement of the talus Internal rotation of the talus Calcaneofibular Posterior distal and medial Inversion and dorsiflexion Posterior talofibular Horizontal Dorsiflexion Posterior displacement of foot Inversion Subtalar Lateral (anterior) talocalcaneal Distal anterolateral Joint separation during inversion and dorsiflexion Medial (posterior) talocalcaneal Distal Anterior translation of talus and inversion Cervical ligament Distal–posterior–lateral Inversion Interosseous Distal and lateral Joint separation Main ligamentous support of longitudinal arches Long plantar Anterior, slightly medial Eversion Short plantar Anterior Eversion Plantar calcaneonavicular Dorsal–anterior–medial Eversion Plantar aponeurosis Anterior Eversion Midtarsal or transverse Bifurcated Joint separation Medial band Longitudinal Plantarflexion Lateral band Horizontal Inversion Dorsal talonavicular Longitudinal Plantarflexion of talus on navicular Dorsal calcaneocuboid Longitudinal Inversion, plantarflexion Intertarsal Dorsal and plantar ligaments Joint motion in direction causing Interosseous ligaments connecting cuneiforms, cuboid, and navicular ligament tautness Flattening of the transverse or longitudinal arch Tarsometatarsal Dorsal, plantar, and interosseous Joint separation Intermetatarsal Dorsal, plantar, and interosseous Joint separation Deep transverse metatarsal Joint separation Flattening of the transverse arch Metatarsophalangeal Fibrous capsule Dorsal, thin—separated from extensor tendons by bursae Flexion Plantar—inseparable from deep surface of plantar and collateral ligaments Extension Collateral Flexion, abduction, or adduction in flexion Interphalangeal Collateral Plantar Flexion, abduction, or adduction in flexion Extension The distal tibiofibular joint (Fig. 21-1) is classified as a syndesmosis, except for approximately 1 mm of the inferior portion, which is covered in hyaline cartilage. The joint consists of a concave tibial surface and a convex or plane surface on the medial distal end of the fibula. The tibia is the second longest bone of the skeleton and is a major weight-bearing bone. There is an elongation into the joint by the synovium of the talocrural joint, the fibers of which are oriented inferiorly and laterally. The fibula serves as a site for muscular and ligamentous attachment, providing stability for the talus at the talocrural joint. A minor amount of fibular elevation and rotation is available at this joint. Sprains of this joint, which are called syndesmotic sprains or high-ankle sprains, typically occur in positions of dorsiflexion with eversion.1 As at the proximal tibiofibular joint (see Chapter 20), support for this joint is provided primarily by ligaments. The joint is stabilized by four ligaments, collectively known as the syndesmotic ligaments. These include the inferior interosseous ligament, the anterior inferior tibiofibular ligament, the posterior inferior tibiofibular ligament, and the inferior transverse ligament. Of these ligaments, the inferior interosseous ligament is the primary stabilizer. The joints of the hindfoot are the talocrural (ankle) joint, and the subtalar (talocalcaneal) joint. The proximal row of tarsals comprises the talus (astragalus) (see Fig. 21-1), and calcaneus (or calcis). The function of the hindfoot is as follows: The joints of the midfoot include the midtarsal (transverse) joint and the tarsometatarsal joints. The midtarsal joint complex consists of the talonavicular and calcaneocuboid joints. The tarsometatarsal joints include the articulations between the cuneiforms, cuboid, and metatarsal bases. The distal tarsal row contains, medial to lateral, the medial, intermediate, and lateral cuneiforms and the cuboid, which is roughly in parallel with the proximal row and which forms a transverse arch, posteriorly (dorsally) convex. Medially, the navicular is positioned between the talus and the cuneiforms (see Fig. 21-1). Laterally, the cuboid is positioned between the calcaneus and the lateral cuneiform and the fourth and fifth metatarsals (see Fig. 21-1). The cuneiforms articulate intimately with the bases of the second and third rays forming a midfoot lever.9 The function of the midfoot is to transmit motions from the hindfoot to the forefoot and to promote stability.8 The joints of the forefoot include the tarsometatarsal joints, the intermetatarsal joints, the MTP joints, and the interphalangeal (IP) joints. The function of the forefoot is to adapt to the terrain, adjusting to uneven surfaces. The first metatarsal is the shortest and the strongest (see Fig. 21-1), whereas the second is the longest and the least mobile, serving as the anatomic touchstone for abduction and adduction of the foot.10 The second and third rays, which are functionally rigid because of their associated osseous and ligamentous configuration, act as the “I-beam” or longitudinal strut of the foot.11 The fourth and fifth rays have the most mobility. The phalanges of the foot, although similar in number and distribution to those in the hand, are shorter and broader than their counterparts. The talocrural (tibiotalar) joint is the synovial articulation between the articulating facets of the talus and the tibiofibular mortise. The talus serves as the link between the foot and the leg through the ankle joint and functions to distribute the body weight posteriorly toward the heel and anteriorly to the midfoot. The talus is divided into an anterior head and a posterior neck and body: The medial malleolus extends distally to approximately one-third of the height of the talus, whereas the lateral malleolus, which is positioned slightly posterior to the medial malleolus, extends distally to approximately two-thirds the height of the talus. Thus, the axis of rotation is inclined distally by 10 degrees and rotated posteriorly by 6 degrees, referencing the lateral side of the joint.1 The fibrous capsule of the ankle joint is relatively thin on its anterior and posterior aspects. It is lined with synovial membrane and reinforced by the collateral ligaments (see later). The talus receives its blood supply from the branches of the anterior and posterior tibial arteries and is very susceptible to aseptic necrosis, particularly with proximal fractures.12 The most important ligaments of the talocrural joint can be divided into two main groups: lateral collaterals and medial (deltoid) collaterals. The lateral collateral ligament complex consists of three separate bands, which function together as the static stabilizers of the lateral ankle. Each of the lateral ligaments has a role in stabilizing the ankle and/or subtalar joint, depending on the position of the foot. As such, these ligaments are commonly involved in ankle sprains.13–17 Anterior Talofibular Ligament. The fibers of this thickening of the anterior capsule course laterally from the talus in the transverse plane and superiorly between the sagittal and frontal planes to attach on the anterior distal tip of the lateral malleolus (Fig. 21-2).18 FIGURE 21-2 Lateral ligaments. (Reproduced, with permission, from Chapter 37. Leg. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The anterior talofibular ligament (ATFL) is an extracapsular structure of the talocrural joint and is approximately 2–5-mm thick and 10–12-mm long.19 The primary function of the ATFL is to resist anterior displacement of the talus relative to the ankle mortise, talocrural internal rotation and plantarflexion.18,20 When the ankle is positioned in plantarflexion, the ATFL is usually the first ankle ligament to be torn in an inversion injury.19 The accessory functions of the ATFL include providing resistance against anterior talar displacement from the mortise and resistance against internal rotation of the talus within the mortise.21 Calcaneofibular Ligament. The calcaneofibular ligament (CFL) (see Fig. 21-2), an extraarticular structure covered by the fibularis (peroneal) tendons, is larger and stronger than the ATFL. It travels at 10–40 degrees from the tip of the lateral malleolus to the lateral side of the calcaneus, paralleling the horizontal axis of the subtalar joint. The fibers of this ligament span across both the talocrural and subtalar joints, which have markedly different axes of rotation. Thus, its attachment is designed so that it does not restrict motion in either joint, whether they move independently or simultaneously.23–25 Although tension within the ligament increases with dorsiflexion, the CFL resists ankle inversion and calcaneal adduction relative to the fibula throughout the full range of ankle motion. However, as the ankle joint passes from dorsiflexion to plantarflexion, the CFL is less able to resist talar tilt to inversion, but it is still able to resist the varus loading with the foot in a plantigrade position, although the ATFL is better suited to resist this tilt.23 If the ankle is in neutral, the CFL may be injured along with the ATFL or alone.26 However, due to its orientation and function, injury to this ligament may have a more profound functional effect on the ankle complex than isolated injuries to the ATFL.27 Posterior Talofibular Ligament. The posterior talofibular ligament (PTFL) (see Fig. 21-2) which is intracapsular but extrasynovial, runs from the posterior medial portion of the fibula to the lateral tubercle aspect of the talus. The orientation of the ligament is relatively horizontal. Its attachment on the talus involves nearly the entire nonarticular portion of the posterior talus to the groove for the flexor hallucis longus (FHL) tendon, and anteriorly to the digital fossa of the fibula, which transmits the vessels that supply the talus and the fibula.28 The PTFL is the strongest of the lateral ligament complex,19 and serves to indirectly aid posterolateral talofibular stability during dorsiflexion due to its anatomic location, where it can act as a true collateral ligament and prevent talar tilt into inversion (abduction of the talus).23 Along with the CFL, ATFL, and medial collateral ligaments, the PTFL assists to couple movements between the lower extremity and the foot.23 The PTFL is rarely injured in a typical ankle sprain before the CFL and ATFL, but movements that involve extreme ankle dorsiflexion, foot external rotation, along with limb internal rotation may cause injury to this ligament. More commonly, the PTFL is involved in syndesmotic (high ankle) sprains. The lateral talocalcaneal interosseous (LTCIL) ligament is sometimes included in this group as it does play a role in lateral ankle and subtalar stability23,29 (see “Talocalcaneal Ligaments” section). Besides maintaining lateral ankle stability, the lateral ankle ligaments play a significant role in maintaining rotational ankle stability.23 Significant compromise to the ATFL and/or CFL leads to a measurable increase in inversion without any tilting of the talus or subtalar gapping.23 A loss of ATFL function permits an increase in external rotation of the leg and unlocks the subtalar joint, allowing further inversion, which may lead to symptomatic instability.23 Medial Collaterals. Collectively, the medial collateral ligaments form a triangular-shaped ligamentous structure known as the deltoid ligament of the ankle (Fig. 21-3). Wide variations have been noted in the anatomic description of the deltoid ligament of the ankle but is generally agreed that it consists of both superficial and deep fibers. The superficial fibers consist of the following: FIGURE 21-3 Medial ligaments. (Reproduced, with permission, from Chapter 37. Leg. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The deep fibers consist of the following: The medial collateral ligaments are most likely to be damaged by a mechanism of hyper eversion (valgus loading).1 Although the calcaneotibial ligament is very thin and supports only negligible forces before failing, the talotibial ligaments are very strong.36,37 Rasmussen et al.38,39 found that the superficial fibers of the deltoid ligament of the ankle specifically limited talar abduction or negative talar tilt and that the deep layers of the deltoid ligament of the ankle ruptured with external rotation of the leg, without the superficial portion being involved. The subtalar joint, which is the articulation between the distal talus and proximal calcaneus, is a major articulation of the hindfoot and plays a significant role in foot function. The articulation consists of two separate, modified ovoid surfaces with their own joint cavities. The two anterior and posterior articulations are connected by an interosseous membrane. This relationship, which is thought to set up a complex screw-like movement that occurs during subtalar joint motion, ensures that the anterior and posterior aspects can move in opposite directions to each other during functional movements (while the anterior aspect is moving medially, the posterior aspect is moving laterally). From a clinical perspective, it may be important to impart gliding that essentially spins the calcaneus around the oblique axis.26 The calcaneus, the largest tarsal bone and the most frequently fractured, projects further posteriorly than the tibia and fibula. It serves as a weight-bearing bone and as a short lever for muscles of the calf, which are attached to its posterior surface. The skin and fat over the distal-inferior area of the calcaneus are specialized for friction and shock absorption.42 The retrocalcaneal bursa lies anterior to the posterosuperior calcaneal tuberosity of the calcaneus. It lubricates the Achilles tendon anteriorly, as well as the superior aspect of the calcaneus.45 The superior or proximal surface of the calcaneus is divisible into thirds. A number of ligaments provide support to the subtalar joint, although some confusion exists in the descriptions and nomenclature of these ligaments.46 The medial talocalcaneal ligament extends from the medial tubercle of the talus to the posterior aspect of the sustentaculum tali and the area of the calcaneus just posterior to the sustentaculum tali. It functions to stabilize against anterior translation of the talus (especially in the initial contact phase of the gait cycle) by producing passive eversion of the talus. This results in a close packing of the lateral foot and fibula. Damage to this ligament, which typically occurs with inversion sprains and rotational compression fractures of the calcaneus, can permit excessive anterior motion of the talus. This excessive motion may result in posterior tibialis tendinopathy47 and on occasion, Achilles’ tendinopathy.48 The fibers of the lateral talocalcaneal ligament (LTCL) are parallel to and blend in with the posterior fibers of the CFL. Unlike the ATFL, CFL, and PTFL, the LTCL does not cross the ankle joint. Instead, the LTCL crosses the posterior subtalar joint and is considered weaker and smaller than the CFL.29 The lateral aspect of the subtalar joint is further stabilized by the interosseous talocalcaneal ligament (see next).28 This highly innervated structure is typically injured with a dorsiflexion and inversion mechanism.49 The LTCL serves to limit supination at the subtalar joint. A combined injury of the ATFL and the interosseous talocalcaneal ligament can induce anterolateral rotary instability of the ankle joint.50 The interosseous talocalcaneal ligament lies in the spaces running inferior and superior between the talus and the calcaneus. The fibers of these ligaments, which run obliquely between the talus and calcaneus, separate the subtalar joint into posterior and anterior chambers.50 Some have described an anterior band (sometimes referred to as the cervical ligament) and posterior band. The talocalcaneal interosseous and cervical ligaments are often collectively referred to as the interosseous ligaments.28 In relation to the sinus tarsi, the anterior band is located more laterally than the posterior band.23 The interosseous talocalcaneal ligament functions as a stabilizer of the subtalar joint keeping the joint surfaces of the talus and calcaneus from separating throughout the entire range of motion (ROM) via a screw-like rotation.26 Severing the interosseous talocalcaneal ligament results in the following51: This ligament is previously described under the talocrural ligaments. The CFL serves to limit supination at the subtalar joint. The transverse tarsal joint complex, which consists of the talonavicular and calcaneocuboid articulations, is also known as the Chopart’s joint. The talonavicular joint is classified as a synovial pivot joint. The joint is actually formed by components of the talus, navicular, calcaneus, and plantar calcaneonavicular (spring) ligament. The convex anterior head of the talus fits into the concavity of the posterior navicular and the anterior component of the subtalar joint and rests on the posterior (dorsal) surface of the spring ligament. The joint capsule is only well developed posteriorly, where it forms the anterior part of the interosseous ligament. Although the plantar calcaneonavicular or spring ligament does not articulate with the talus, it prevents the talar head from plantarflexing (dorsiflexion of the navicular relative to the talus), and also limits the medial longitudinal arch from lowering.52 The talonavicular joint moves three times more than the calcaneocuboid joint, with movement between the navicular and the cuboid being negligible.53 The calcaneocuboid joint is classified as a plane synovial joint. The anterior surface of the calcaneus, which articulates with the reciprocally shaped posterior surface of the cuboid, is relatively convex in an oblique horizontal direction and relatively concave in an oblique vertical direction.54 The cuboid, most lateral in the distal tarsal row, is located between the calcaneus proximally and the fourth and fifth metatarsals distally. To the posterior (dorsal) surface are attached posterior (dorsal) calcaneocuboid, cubonavicular, cuneocuboid, and cubometatarsal ligaments, and to the proximal edge of the plantar ridge, deep fibers of the long plantar ligament. To the projecting proximal–medial part of the plantar surface are attached a slip of the tendon of tibialis posterior and flexor hallucis brevis (FHB). To the rough part of the medial cuboidal surface are attached the interosseous, cuneocuboid, and cubonavicular ligaments, and proximally the medial calcaneocuboid ligament, which is the lateral limb of the bifurcated ligament.28 The capsule is thickened posteriorly (dorsally) to form the posterior (dorsal) calcaneocuboid ligament. The joint has a large plantar phalanx to provide additional support during weight bearing. A number of ligaments help provide support to this region. The spring ligament (plantar calcaneonavicular Fig. 21-3) connects the navicular bone to the sustentaculum tali on the calcaneus. The ligaments of the calcaneocuboid joint include the long plantar ligament and a portion of the bifurcate ligament posterior (dorsally). The plantar calcaneocuboid ligament, sometimes referred to as the short plantar ligament, is a relatively broad and strong strap-like structure that extends from the area of the anterior tubercle of the calcaneus to the adjacent plantar surface of the cuboid bone. It provides plantar support to the joint and possibly helps to limit flattening of the lateral longitudinal arch. The tarsometatarsal (Lisfranc’s) joint includes the articulations between the cuneonavicular joint, intercuneiform joints, the cuneocuboid joint, the cubometatarsal joint, the cubonavicular, and the intermetatarsal joints. The cuneonavicular joint is classified as a plane synovial, joint. The navicular presents a convex surface to the concave surface of the combined cuneiforms. The wedge-like cuneiform bones articulate with the navicular proximally and with the bases of the first to third metatarsals distally (see Fig. 21-1). The medial cuneiform is the largest and the intermediate, the smallest. In the intermediate and lateral cuneiforms, the posterior (dorsal) surface is the base of the wedge, but in the medial, the wedge is reversed, a prime factor in shaping the transverse arch. The wedge shape of these bones also provides a cavity for the neurovascular and musculotendinous structures of the foot. The proximal surface of all three cuneiforms form a concavity for the convex surface of the navicular. In the intermediate and lateral cuneiforms, the posterior (dorsal) surface is the base of the wedge, but in the medial, the wedge is reversed, which assists in the formation of the transverse arch. The medial cuneiform is the largest, the intermediate the smallest. The ligament of Lisfranc’s, also referred to as the cuneometatarsal interosseous ligament, runs between the medial cuneiform and second metatarsal base. Disruption of this ligament can lead to a dislocation of the medial aspect of the foot, as the first metatarsal and medial cuneiform separate from the second metatarsal and intermediate cuneiform. This ligament is often involved in low and high energy injuries to the midfoot.55 The joint cavity and capsule of the cuneonavicular joint is continuous with that of the intercuneiform and cuneocuboid joints, and the synovium is continuous with that of these joints, the second and third cuneometatarsal joints, and the intermetatarsal joints of each base except the fifth. These joints (see Fig. 21-1) are classified as plane synovial joints. The joint capsule and synovium is contiguous between all of these joints and with that of the cuneonavicular joint. Dysfunctions in the cuneocuboid joint result from a collapse of the plantar supporting structures or from direct trauma. Such dysfunctions may result in the cuboid subluxing in a plantar direction (medial border of cuboid moves inferiorly). At the intercuneiform joints, the third cuneiform may sublux on the second cuneiform. Laterally, the cuboid bone articulates with the fourth and fifth metatarsals distally, and with the calcaneus proximally. When considered alone, the cubometatarsal joint is classified as a plane synovial joint. When the cubometatarsal joints are considered together, they form a modified sellar joint. The joint capsule and synovium of the fourth and fifth cubometatarsal joints are separated from the other tarsometatarsal joints by an interosseous ligament. The cubonavicular joint (see Fig. 21-1) is classified as a syndesmosis or a plane synovial joint. If the joint is synovial, the capsule and synovium is continuous with the cuneonavicular joint. The intermetatarsal joints (see Fig. 21-1) are classified as plane synovial joints. If the joint is synovial, the capsule and synovium is continuous with the cuneonavicular joint. Motion at these joints is confined to posterior (dorsal)/anterior (plantar) gliding, producing a fanning and folding motion of the foot. Proximally, the five metatarsals articulate with the tarsals and with themselves through broad concavities.10 Available movements at the tarsometatarsal joint complex are a pronation twist and a supination twist, which mainly occur in closed kinetic chain at the end range of hindfoot and ankle movements. For example, in extreme closed kinetic chain plantarflexion, such as when standing on tip toes, the tarsometatarsal joints provide a compensatory pronation twist to prevent an excessively inverted position of the metatarsal heads and allow the forefoot to remain in contact with the ground.1 Conversely, during extreme closed kinetic chain dorsiflexion, such as at the end ROM during a squat, the tarsometatarsal joints provide a compensatory supination twist to prevent excessive eversion of the metatarsal heads, so the forefoot can remain in contact with the ground.1 The MTP joints (see Fig. 21-1) are classified as condyloid synovial joints. The capsule and synovium in each of these joints are confined to its own joint and posteriorly (dorsally) is thin, whereas plantarly (anteriorly), it is blended with the plantar and collateral ligaments. The rotation that occurs in the early stages of development of the limbs results in the thumb being the most lateral digit in the hand, whereas the hallux (great toe) is the most medial digit in the foot.56 The concave bases of the proximal phalanges (see Fig. 21-1) articulate with the convex heads of the metatarsals. The first MTP joint, with its more extensive articular surface on the anterior (plantar) aspect of the metatarsal than on the posterior (dorsal), allows for a greater freedom of motion,56 and its anterior (plantar) surface forms two grooves for articulation with the hallucal sesamoids (see next section). The fifth metatarsal has a lateral styloid process at its base, which serves as the insertion site for the tendon of the fibularis (peroneus) brevis. The styloid area is often avulsed during acute inversion injuries of the foot.10 Three types of forefoot are recognized based on the length of the metatarsal bones, although it is unclear whether these various types affect foot function in any way.56 Stability of the MTP joints is primarily provided by a musculocapsular ligamentous complex anteriorly (plantarly), and medially and laterally by the medial and lateral collateral ligaments, respectively. The first MTP joint is the articulation between the head of the first metatarsal and the proximal phalanx. Although there is some anatomic variation from patient to patient, the first MTP joint is typically a cam-shaped, bicondylar-hinged joint that has 2 degrees of freedom.57 The first MTP joint has little inherent stability because the proximal phalanx has a fairly shallow cavity in which the metatarsal head articulates. The joint is stabilized posteriorly (dorsally) by the capsule and expansion of the extensor hallucis tendon. Fan-shaped medial and lateral collateral ligaments provide valgus and varus stability, respectively. The plantar surface of the capsule is reinforced by a fibrocartilaginous plate, called the plantar accessory ligament. In addition, the MTP joint is dynamically stabilized by the short flexor complex (FHB and the two sesamoids embedded in the FHB tendons), the adductor hallucis, and the abductor hallucis tendons. The sesamoids are connected distally to the base of the proximal phalanx by extensions of the FHB called the plantar plate. Typically, the sesamoids are anterior (plantar) to the medial and lateral condyles of the metatarsal pad. The sesamoids are separated on the anterior (plantar) aspect of the first metatarsal head by a cresta, which helps to stabilize the sesamoids, and are connected to one another by the intersesamoidal ligament. The abductor hallucis inserts into the medial sesamoid, and the adductor hallucis inserts into the lateral sesamoid. The FHL (Fig. 21-4) pierces the two heads of the FHB muscle to run just anterior (plantar) to the intersesamoidal ligament. In normal gait, the capsuloligamentous complex of the first MTP joint must withstand 40–60% of body weight, but in athletic activity, this can reach as much as eight times body weight.59–65 While there are many conditions that can affect first-ray function, the most prevalent include progressive first MTP joint degeneration, hallux abducto-valgus (HAV), hallucal sesamoid syndrome, flexor hallucal longus tendinopathies, turf toe, metatarsalgia, and interdigital neuroma.11 FIGURE 21-4 Medial aspect of the ankle and foot. (Reproduced, with permission, from Chapter 38. Foot. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The IP joints are classified as condyloid synovial joints. The hallux has two phalanges, whereas each of the remaining toes have three (see Fig. 21-1). The IP joints are classified as simple, synovial, modified sellar joints. The saddle-shaped articular fossa of the head of the proximal phalanx articulates with the base of the intermediate phalanx. This in turn receives the smaller and flatter distal phalanx. An accessory ossicle (accessory bone) is an anomalous bone that fails to unite during developmental ossification. Common locations include the fibular malleolus, tibial malleolus, navicular, and talus. The accessory navicular is the most common accessory bone in the foot.66 It occurs on the medial, anterior (plantar) border of the navicular, at the site of the tibialis posterior tendon insertion.67 The incidence in the general population has been reported to be 4–14%67,68 The posterior aspect of the talus often exhibits a separate ossification center, appearing at 8–10 years of age in girls and 11–13 years of age in boys. Fusion usually occurs 1 year after its appearance.69,70 When fusion does not occur, an os trigonum is formed (see Chapter 5). The terms plantar fascia and plantar aponeurosis (Fig. 21-4) are often used interchangeably, although strictly speaking only the central part of the plantar fascia is extensively aponeurotic.71 The plantar fascia is the investing fascial layer of the anterior (plantar) aspect of the foot that originates from the os calcis and inserts through a complex network to the anterior (plantar) forefoot. It is a tough, fibrous layer, composed histologically of both collagen and elastic fibers. The plantar fascia is often regarded as being analogous to the palmar fascia of the hand. However, unlike the fascial layer of the palm, which is generally thin, the plantar fascia is a thick structure, and not only serves a supportive and protective role, but is also intricately involved with the weight-bearing function of the foot.71 The load to failure of the plantar fascia is estimated in the range of 1,000 N.72 The plantar fascia is divided into three major areas: a central portion and medial and lateral sections, each oriented longitudinally on the anterior (plantar) surface of the foot.33 With standing and weight bearing, the plantar fascia plays a major role in the support of the weight of the body, by virtue of its attachments across the medial longitudinal arch. During the different phases of gait, the plantar fascia assumes different biomechanical functions, which have been described as a windlass mechanism or a truss mechanism: During the initial contact, and during the first half of the stance phase of the gait cycle (see Chapter 6) with the toes in neutral, the plantar fascia relaxes, flattening the arch. This allows the foot to accommodate to irregularities in the walking surface and to absorb shock.73 As the foot proceeds from midstance to terminal stance, the foot pressure migrates anteriorly and the toes dorsiflex and, through its attachments to the toes via the plantar plate, the plantar fascia tightens. The tension in the plantar fascia is directly related to dorsiflexion of the MTP of the toes.75 The plantar fascia is pulled over the metatarsal heads, causing the metatarsal heads to be depressed and the longitudinal arch to rise.71 During the swing phase of gait, the plantar fascia is under little tension and appears to serve no important functional role. The extensor and fibular (peroneal) retinacula contribute to ankle and hindfoot stability primarily due to their anatomical orientation. There are four important ankle retinacula, which function to tether the leg tendons as they cross the ankle to enter the foot (Fig. 21-4).10 Twenty-three muscles are involved with motion at the foot and ankle, 12 of which originate on the tibia or fibula, and 11 on the foot itself. For simplicity sake, the muscles of the leg and foot are divided into extrinsic muscles (those that originate at the tibia or fibula), and intrinsic (those that originate from the foot itself) muscles. The extrinsic muscles of the foot (Table 21-4) are further subdivided based on location into anterior, posterior superficial, posterior deep, and lateral compartments. TABLE 21-4 Extrinsic Muscle Attachments and Innervation Muscle Proximal Distal Innervation Gastrocnemius Medial and lateral condyle of femur Posterior surface of calcaneus through Achilles tendon Tibial S2 (S1) Plantaris Lateral supracondylar line of femur Posterior surface of calcaneus through Achilles tendon Tibial S2 (S1) Soleus Head of fibula, proximal third of shaft, soleal line and midshaft of posterior tibia Posterior surface of calcaneus through Achilles tendon Tibial S2 (S1) Tibialis anterior Distal to lateral tibial condyle, proximal half of lateral tibial shaft, and interosseous membrane First cuneiform bone, medial and plantar surfaces, and base of first metatarsal Deep fibular (peroneal) L4 (L5) Tibialis posterior Posterior surface of tibia, proximal two-thirds posterior of fibula, and interosseous membrane Tuberosity of navicular bone and tendinous expansion to other tarsals and metatarsals Tibial L4 and L5 Fibularis (peroneus) longus Lateral condyle of tibia, head, and proximal two-thirds of fibula Base of first metatarsal and first cuneiform, lateral side Superficial fibular (peroneal) L5 and S1 (S2) Fibularis (peroneus) brevis Distal two-thirds of lateral fibular shaft Tuberosity of fifth metatarsal Superficial fibular (peroneal) L5 and S1 (S2) Fibularis (peroneus) tertius Lateral slip from extensor digitorum longus Tuberosity of fifth metatarsal Deep fibular (peroneal) L5 and S1 Flexor hallucis longus Posterior distal two-thirds fibula Base of distal phalanx of great toe Tibial S2 (S3) Flexor digitorum longus Middle three-fifths of posterior tibia Base of distal phalanx of lateral four toes Tibial S2 (S3) Extensor hallucis longus Middle half of anterior shaft of fibula Base of distal phalanx of great toe Deep fibular (peroneal) L5 and S1 Extensor digitorum longus Lateral condyle of tibia proximal anterior surface of shaft of fibula One tendon to each lateral four toes, to middle phalanx, and extending to distal phalanges Deep fibular (peroneal) L5 and S1 This compartment contains the dorsiflexors (extensors) of the foot. These include the tibialis anterior, fibularis tertius, EDL, and EHL (see Fig. 21-5). FIGURE 21-5 Lateral aspect of foot and ankle. (Reproduced, with permission, from Chapter 37. Leg. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
CHAPTER 21
Lower Leg, Ankle, and Foot
OVERVIEW
ANATOMY
DISTAL TIBIOFIBULAR JOINT
HINDFOOT
 to influence the function and movement of the midfoot and forefoot;
to influence the function and movement of the midfoot and forefoot;
 to convert the transverse rotations of the lower extremity into sagittal, transverse, and frontal plane movements.8
to convert the transverse rotations of the lower extremity into sagittal, transverse, and frontal plane movements.8
MIDFOOT
FOREFOOT
THE TALOCRURAL (ANKLE) JOINT
 Body. The superior dome-shaped surface of the body articulates with the tibia. The body is convex in the anteroposterior (A-P) direction and slightly concave in the mediolateral (M-L) and superior directions. The shape of this articulating surface can be compared with that of a cone, with the base of the cone facing laterally and the apex medially. Since the superior aspect of the body of the talus is wedge shaped with the wider portion anterior, no varus/valgus movement is possible when the ankle is positioned in maximum dorsiflexion, unless the mortise or the tibiofibular ligaments are compromised.
Body. The superior dome-shaped surface of the body articulates with the tibia. The body is convex in the anteroposterior (A-P) direction and slightly concave in the mediolateral (M-L) and superior directions. The shape of this articulating surface can be compared with that of a cone, with the base of the cone facing laterally and the apex medially. Since the superior aspect of the body of the talus is wedge shaped with the wider portion anterior, no varus/valgus movement is possible when the ankle is positioned in maximum dorsiflexion, unless the mortise or the tibiofibular ligaments are compromised.
 Neck. The neck of the talus is a narrow region between the head and the body of the talus, and it is medially inclined. Its rough surfaces serve as attachments for ligaments. Inferior to the neck of the talus is the sulcus tali, which, when the talus and the calcaneus are articulated, roofs the sinus tarsi (a cylindrical cavity located between the talus and calcaneus on the lateral aspect of the foot that separates the anterior and posterior aspects of the subtalar joint—see later) and is occupied by the talocalcaneal interosseous and cervical ligaments.
Neck. The neck of the talus is a narrow region between the head and the body of the talus, and it is medially inclined. Its rough surfaces serve as attachments for ligaments. Inferior to the neck of the talus is the sulcus tali, which, when the talus and the calcaneus are articulated, roofs the sinus tarsi (a cylindrical cavity located between the talus and calcaneus on the lateral aspect of the foot that separates the anterior and posterior aspects of the subtalar joint—see later) and is occupied by the talocalcaneal interosseous and cervical ligaments.
 Head. The plantar surface of the head has three articular areas separated by smooth ridges. The most posterior and largest of the articular areas is oval, slightly convex, and rests on a shelf-like medial calcanean projection called the sustentaculum tali. The other two articulating facets connect the talus with the navicular and the plantar calcaneonavicular ligament.
Head. The plantar surface of the head has three articular areas separated by smooth ridges. The most posterior and largest of the articular areas is oval, slightly convex, and rests on a shelf-like medial calcanean projection called the sustentaculum tali. The other two articulating facets connect the talus with the navicular and the plantar calcaneonavicular ligament.
Talocrural Ligaments
Lateral Collaterals
Lateral Talocalcaneal Interosseous
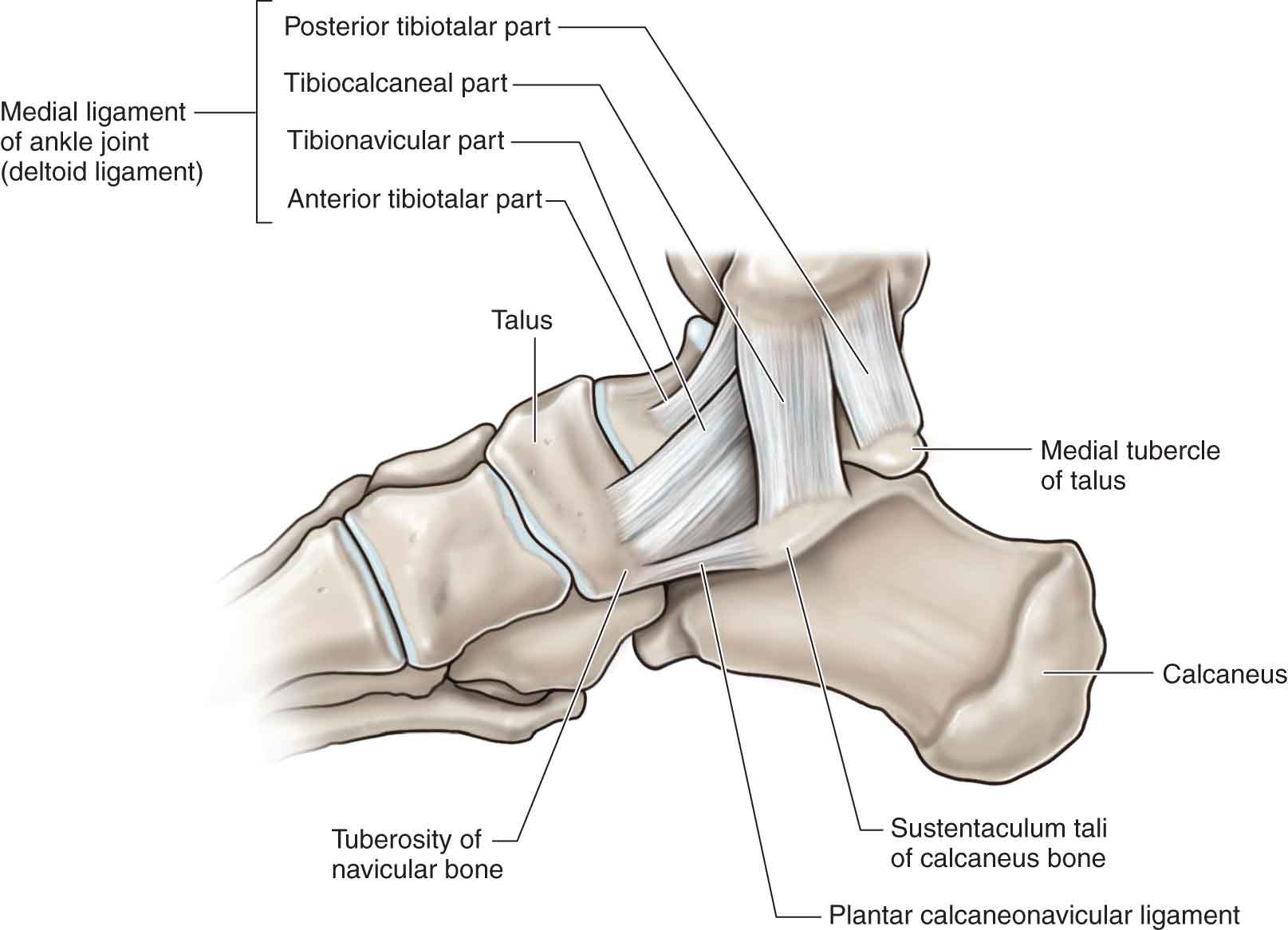
 Tibionavicular fibers (see Fig. 21-3). These fibers extend from the medial malleolus to the tuberosity of the navicular and serve to resist lateral translation and external rotation of the talus.
Tibionavicular fibers (see Fig. 21-3). These fibers extend from the medial malleolus to the tuberosity of the navicular and serve to resist lateral translation and external rotation of the talus.
 Posterior tibiotalar fibers (see Fig. 21-3). These fibers travel in a posterolateral direction from the medial malleolus to the medial side of the talus and medial tuberosity of the talus. These fibers resist ankle dorsiflexion and lateral translation and external rotation of the talus.
Posterior tibiotalar fibers (see Fig. 21-3). These fibers travel in a posterolateral direction from the medial malleolus to the medial side of the talus and medial tuberosity of the talus. These fibers resist ankle dorsiflexion and lateral translation and external rotation of the talus.
 Tibiocalcaneal fibers (see Fig. 21-3). These thin fibers extend from the medial malleolus to the sustentaculum tali. The fibers are oriented in such a way that they resist abduction of the talus, calcaneus and navicular when the foot and ankle are positioned in plantarflexion and eversion.34 The tibiocalcaneal ligament is usually the first ruptured with an eversion injury.35
Tibiocalcaneal fibers (see Fig. 21-3). These thin fibers extend from the medial malleolus to the sustentaculum tali. The fibers are oriented in such a way that they resist abduction of the talus, calcaneus and navicular when the foot and ankle are positioned in plantarflexion and eversion.34 The tibiocalcaneal ligament is usually the first ruptured with an eversion injury.35
 Anterior tibiotalar fibers (see Fig. 21-3). The fibers of this strong ligament extend from the tip of the medial malleolus to the anterior aspect of the medial surface of the talus. These fibers are oriented in such a way that they resist abduction of the talus when it is in plantarflexion and eversion. Such is the strength of these fibers that an injury to this ligament rarely occurs with an eversion sprain but is often associated with an avulsion fracture in more traumatic injuries.
Anterior tibiotalar fibers (see Fig. 21-3). The fibers of this strong ligament extend from the tip of the medial malleolus to the anterior aspect of the medial surface of the talus. These fibers are oriented in such a way that they resist abduction of the talus when it is in plantarflexion and eversion. Such is the strength of these fibers that an injury to this ligament rarely occurs with an eversion sprain but is often associated with an avulsion fracture in more traumatic injuries.
SUBTALAR (TALOCALCANEAL) JOINT
 The anterior joint consists of two to three concave facets on the superior aspect of the calcaneus and a convex facet on the inferior aspect of the talus. Typically there is an anterior, medial, and posterior articular facet on the calcaneus. The anterior and medial facets sometimes form a single articular surface resulting in two rather than three articular facets.26 The anterior component is situated more medial than the posterior, giving the plane of the joint an average 42 degrees (±9 degrees) superior from the transverse foot plane and 23 degrees (±11 degrees) medial from the sagittal foot plane.41
The anterior joint consists of two to three concave facets on the superior aspect of the calcaneus and a convex facet on the inferior aspect of the talus. Typically there is an anterior, medial, and posterior articular facet on the calcaneus. The anterior and medial facets sometimes form a single articular surface resulting in two rather than three articular facets.26 The anterior component is situated more medial than the posterior, giving the plane of the joint an average 42 degrees (±9 degrees) superior from the transverse foot plane and 23 degrees (±11 degrees) medial from the sagittal foot plane.41
 The posterior joint consists of a cone-shaped facet on the superior aspect of the calcaneus and a concave facet on the inferior aspect of the talus.26
The posterior joint consists of a cone-shaped facet on the superior aspect of the calcaneus and a concave facet on the inferior aspect of the talus.26
 The posterior third. This is a roughened surface that is concavoconvex in extension, the convexity transverse. It supports fibroadipose tissue between the calcaneal tendon and the ankle joint. Distal to the posterior articular facet is a rough depression that narrows into a groove on the medial side—the sulcus calcanei—which completes the sinus tarsi with the talus.
The posterior third. This is a roughened surface that is concavoconvex in extension, the convexity transverse. It supports fibroadipose tissue between the calcaneal tendon and the ankle joint. Distal to the posterior articular facet is a rough depression that narrows into a groove on the medial side—the sulcus calcanei—which completes the sinus tarsi with the talus.
 The middle third. This surface carries the posterior talar facet and is oval and convex anteroposteriorly.
The middle third. This surface carries the posterior talar facet and is oval and convex anteroposteriorly.
 The anterior third. This surface is only partly articular.
The anterior third. This surface is only partly articular.
Subtalar (Talocalcaneal) Ligaments
Medial Talocalcaneal
Lateral Talocalcaneal
Interosseous Talocalcaneal
 increased range of the subtalar joint motion especially toward supination
increased range of the subtalar joint motion especially toward supination
 instability of the subtalar joint
instability of the subtalar joint
 a disconnect between the calcaneus and talus resulting in marked motion between the tibia and calcaneus.
a disconnect between the calcaneus and talus resulting in marked motion between the tibia and calcaneus.
Posterior Talocalcaneal
Calcaneofibular
TRANSVERSE TARSAL JOINT COMPLEX
Talonavicular
Calcaneocuboid
 The long and strong plantar ligament attaches to the plantar surface of the calcaneus, the tuberosity on the plantar surface of the cuboid bone, and to the bases of the second, third, and fourth (and possibly fifth) metatarsals.28 The plantar ligament functions to provide indirect plantar support to the joint, by limiting the amount of flattening of the lateral longitudinal arch of the foot. Together with the groove in the cuboid bone, it forms a tunnel for the passage of the fibularis (peroneus) longus tendon across the plantar surface of the foot.28 The perpendicular arrangement of the long and short plantar ligaments may compress the calcaneocuboid joint increasing its stability.26 During inversion, the cuboid inverts approximately twice as much of the calcaneus.53
The long and strong plantar ligament attaches to the plantar surface of the calcaneus, the tuberosity on the plantar surface of the cuboid bone, and to the bases of the second, third, and fourth (and possibly fifth) metatarsals.28 The plantar ligament functions to provide indirect plantar support to the joint, by limiting the amount of flattening of the lateral longitudinal arch of the foot. Together with the groove in the cuboid bone, it forms a tunnel for the passage of the fibularis (peroneus) longus tendon across the plantar surface of the foot.28 The perpendicular arrangement of the long and short plantar ligaments may compress the calcaneocuboid joint increasing its stability.26 During inversion, the cuboid inverts approximately twice as much of the calcaneus.53
 The bifurcate ligament functions to support the medial and lateral aspects of the foot when weight bearing in a plantarflexed position (twisted).
The bifurcate ligament functions to support the medial and lateral aspects of the foot when weight bearing in a plantarflexed position (twisted).
TARSOMETATARSAL JOINT
CUNEONAVICULAR
INTERCUNEIFORM AND CUNEOCUBOID JOINTS
CUBOMETATARSAL
CUBONAVICULAR
INTERMETATARSAL
METATARSOPHALANGEAL
 Index plus. This type is characterized by the first metatarsal being longer than the second, with the other three of progressively decreasing lengths, so that 1 > 2 > 3 > 4 > 5.
Index plus. This type is characterized by the first metatarsal being longer than the second, with the other three of progressively decreasing lengths, so that 1 > 2 > 3 > 4 > 5.
 Index plus–minus. In this type, the first metatarsal is of the same length as the second, with the others progressively diminishing in length, so that 1 = 2 > 3 > 4 > 5.
Index plus–minus. In this type, the first metatarsal is of the same length as the second, with the others progressively diminishing in length, so that 1 = 2 > 3 > 4 > 5.
 Index minus. With this type, the second metatarsal is longer than the first and third metatarsals. The fourth and fifth metatarsals are progressively shorter than the third, so that 1 < 2 > 3 > 4 > 5.
Index minus. With this type, the second metatarsal is longer than the first and third metatarsals. The fourth and fifth metatarsals are progressively shorter than the third, so that 1 < 2 > 3 > 4 > 5.
First MTP Joint
INTERPHALANGEAL
ACCESSORY OSSICLE
PLANTAR FASCIA/PLANTAR APONEUROSIS
 Central portion. The central portion is the major portion of the plantar fascia both anatomically and functionally.71 This portion is the thickest and the strongest and is narrowest proximally where it attaches to the medial process of the calcaneal tuberosity, proximal to the flexor digitorum brevis (FDB). This attachment site is often involved in a condition called plantar heel pain (see “Intervention Strategies” section); however, pain can occur anywhere in the structure. From its insertion, the central portion of the fascia fans out and becomes thinner distally. Its fibers are longitudinally oriented and adhere to the underlying FDB muscle.71 The central portion envelops the FDB muscle on both sides, forming the medial and lateral intermuscular septums, which anchor the plantar fascia to the deep plantar pedis.71 At the midshaft of the second to fifth MTP joints, the body of the central portion branches into five superficial longitudinal tracts.71 All five superficial longitudinal tracts terminate by inserting into, and blending with, the overlying subcutaneous tissues and skin. Due to the anatomical connections of the central portion, dorsiflexion of the toe slides the plantar pads distally, placing tension on the plantar aponeurosis. The central portion of the fascia primarily functions as a dynamic stabilizer of the medial longitudinal arch during weight-bearing activities.
Central portion. The central portion is the major portion of the plantar fascia both anatomically and functionally.71 This portion is the thickest and the strongest and is narrowest proximally where it attaches to the medial process of the calcaneal tuberosity, proximal to the flexor digitorum brevis (FDB). This attachment site is often involved in a condition called plantar heel pain (see “Intervention Strategies” section); however, pain can occur anywhere in the structure. From its insertion, the central portion of the fascia fans out and becomes thinner distally. Its fibers are longitudinally oriented and adhere to the underlying FDB muscle.71 The central portion envelops the FDB muscle on both sides, forming the medial and lateral intermuscular septums, which anchor the plantar fascia to the deep plantar pedis.71 At the midshaft of the second to fifth MTP joints, the body of the central portion branches into five superficial longitudinal tracts.71 All five superficial longitudinal tracts terminate by inserting into, and blending with, the overlying subcutaneous tissues and skin. Due to the anatomical connections of the central portion, dorsiflexion of the toe slides the plantar pads distally, placing tension on the plantar aponeurosis. The central portion of the fascia primarily functions as a dynamic stabilizer of the medial longitudinal arch during weight-bearing activities.
 Lateral and medial portions. The smaller and thinner lateral and medial portions are thin and cover the undersurface of the abductor digiti minimi and abductor hallucis muscles, respectively.
Lateral and medial portions. The smaller and thinner lateral and medial portions are thin and cover the undersurface of the abductor digiti minimi and abductor hallucis muscles, respectively.
 Windlass. The windlass effect on the plantar fascia helps to reconstitute the medial longitudinal arch and generates a more rigid foot for propulsion during the toe-off portion of the gait cycle.73 The plantar fascia, which serves as the cable of the windlass mechanism, wraps around the head of the metatarsal, which serves as the cylinder of the windlass, and raises the medial longitudinal arch to attach to the medial tubercle of the calcaneus.74
Windlass. The windlass effect on the plantar fascia helps to reconstitute the medial longitudinal arch and generates a more rigid foot for propulsion during the toe-off portion of the gait cycle.73 The plantar fascia, which serves as the cable of the windlass mechanism, wraps around the head of the metatarsal, which serves as the cylinder of the windlass, and raises the medial longitudinal arch to attach to the medial tubercle of the calcaneus.74
 Truss. In the truss system of the foot, the triangular unit is the medial longitudinal arch with the ankle joint functioning as the apex of the triangle, the calcaneus and talus are the posterior struts, and the first ray is the anterior strut. The plantar fascia stabilizes the two rigid struts inferiorly by limiting the ability of the struts to spread apart.
Truss. In the truss system of the foot, the triangular unit is the medial longitudinal arch with the ankle joint functioning as the apex of the triangle, the calcaneus and talus are the posterior struts, and the first ray is the anterior strut. The plantar fascia stabilizes the two rigid struts inferiorly by limiting the ability of the struts to spread apart.
RETINACULA
 Inferior extensor retinaculum. The inferior extensor retinaculum runs from the tip of the lateral malleolus to insert on the lateral calcaneus and sinus tarsi. It also blends with the inferior fibular retinaculum and may improve evertor muscle function.76 It consists of two parts: superior and inferior. The superior part functions to contain the tendons of the extensor digitorum longus (EDL), extensor hallucis longus (EHL), tibialis anterior, and fibularis (peroneus) tertius. The Y-shaped inferior part consists of an upper and a lower band, which prevent “bow-stringing” of the posterior (dorsal) tendons.
Inferior extensor retinaculum. The inferior extensor retinaculum runs from the tip of the lateral malleolus to insert on the lateral calcaneus and sinus tarsi. It also blends with the inferior fibular retinaculum and may improve evertor muscle function.76 It consists of two parts: superior and inferior. The superior part functions to contain the tendons of the extensor digitorum longus (EDL), extensor hallucis longus (EHL), tibialis anterior, and fibularis (peroneus) tertius. The Y-shaped inferior part consists of an upper and a lower band, which prevent “bow-stringing” of the posterior (dorsal) tendons.
 Superior fibular (peroneal) retinaculum. The superior fibular retinaculum, which courses from the lateral malleolus to the calcaneus, parallel with the posterior fibers of the CFL,50 firmly tethers the fibularis (peroneus) longus and brevis tendons behind the fibular malleolus.
Superior fibular (peroneal) retinaculum. The superior fibular retinaculum, which courses from the lateral malleolus to the calcaneus, parallel with the posterior fibers of the CFL,50 firmly tethers the fibularis (peroneus) longus and brevis tendons behind the fibular malleolus.
 Flexor retinaculum. The flexor retinaculum provides a firm support structure for the flexor digitorum longus (FDL), FHL, tibialis posterior, and the neurovascular bundle.
Flexor retinaculum. The flexor retinaculum provides a firm support structure for the flexor digitorum longus (FDL), FHL, tibialis posterior, and the neurovascular bundle.
EXTRINSIC MUSCLES OF THE LEG AND FOOT
Anterior Compartment